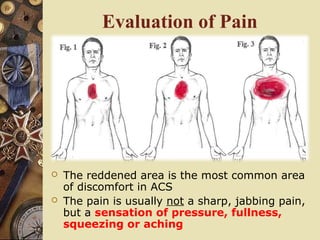
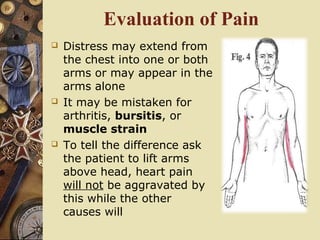
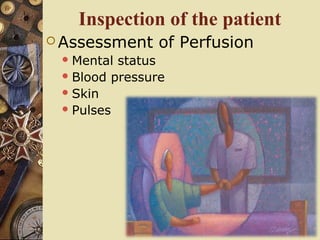
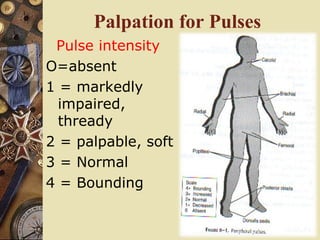
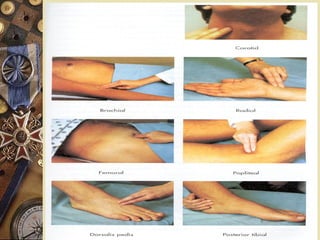
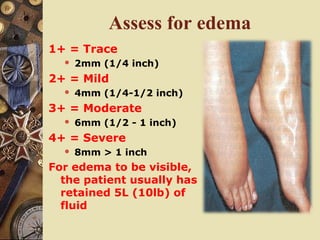
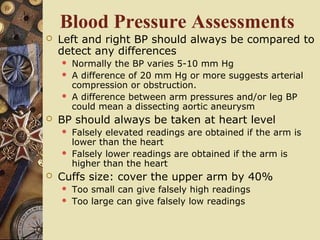
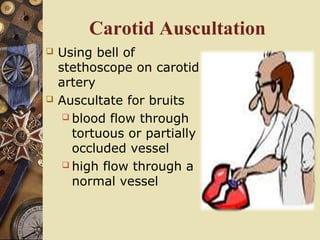
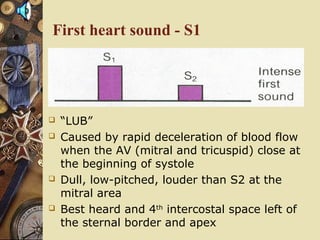
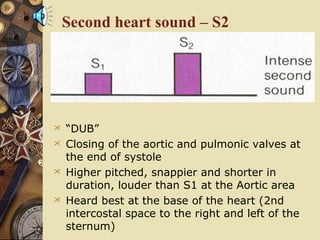
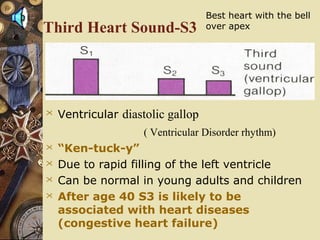
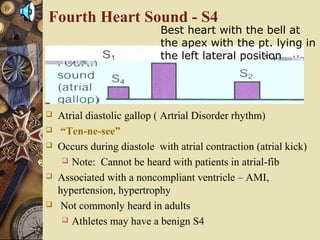
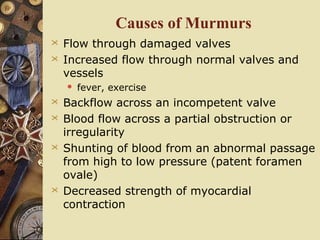
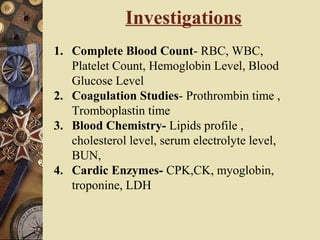
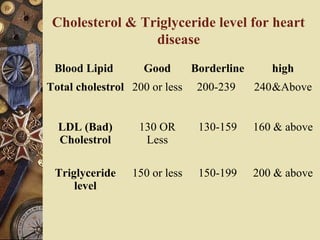
This document provides information on assessing patients for cardiac issues. It discusses important risk factors and symptoms of heart disease. The physical assessment includes inspecting the skin, measuring vital signs, auscultating heart sounds, and evaluating the lungs and extremities for edema. The assessment also involves taking a health history and reviewing diagnostic tests such as echocardiograms, EKGs, and blood work including cardiac enzyme levels and lipid profiles. A thorough cardiac assessment provides valuable information to identify underlying heart conditions.