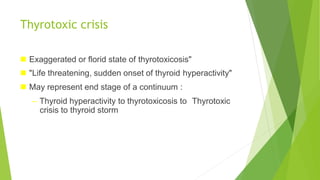
Hyperthyroidism and thyrotoxicosis occur when the thyroid gland overproduces thyroid hormones. Thyroid storm is a life-threatening exacerbation of thyrotoxicosis caused by factors like infection, surgery, or medication changes. It involves fever, sweating, tachycardia, anxiety, and heart failure. Treatment focuses on cooling the patient, blocking further hormone production with antithyroid drugs and iodine, and supporting heart and brain function with beta-blockers and glucocorticoids. Thyroidectomy may be required for severe cases not responding to medical management.
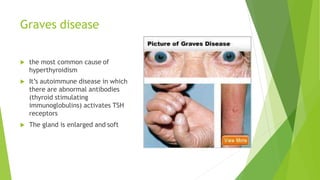
![Hyperthyroidism
is a condition in which the thyroid gland produces and secretes excessive
amounts of the free (not protein bound circulating in the blood[1]) thyroid
hormones -triiodothyronine (T3) and/or thyroxine (T4)](https://image.slidesharecdn.com/thyroidstorm-190607062459/85/Thyroidstorm-ppt-2-320.jpg)


![Cardiac symptoms
Hypertension with wide pulse pressure
Hypotension in later stages with shock
Tachycardia disproportionate to fever
Signs of high-output heart failure
Cardiac arrhythmia (Supraventricular arrhythmias are
more common, [eg, atrial flutter and fibrillation], but
ventricular tachycardia may also occur.)](https://image.slidesharecdn.com/thyroidstorm-190607062459/85/Thyroidstorm-ppt-14-320.jpg)
![causes
Thyroid storm is precipitated by the following factors in individuals with thyrotoxicosis:
Sepsis
Surgery
Anesthesia induction
Radioactive iodine (RAI) therapy
Drugs (anticholinergic and adrenergic drugs such as pseudoephedrine; salicylates;
nonsteroidal anti-inflammatory drugs [NSAIDs]; chemotherapy and iodinated contrast
agents
Excessive thyroid hormone (TH) ingestion
Withdrawal of or noncompliance with antithyroid medications
Diabetic ketoacidosis
Direct trauma to the thyroid gland
Vigorous palpation of an enlarged thyroid
Toxemia of pregnancy and labor in older adolescents; molar pregnancy](https://image.slidesharecdn.com/thyroidstorm-190607062459/85/Thyroidstorm-ppt-15-320.jpg)