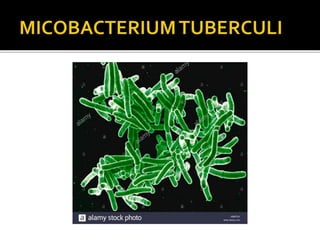
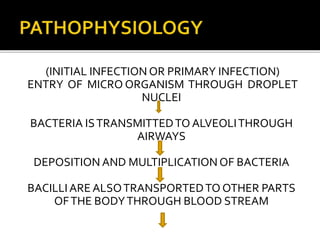
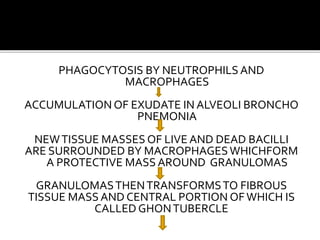
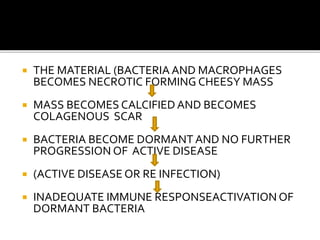
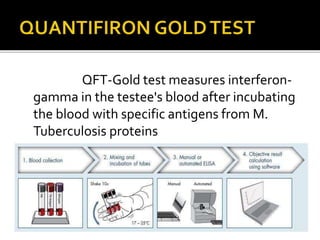
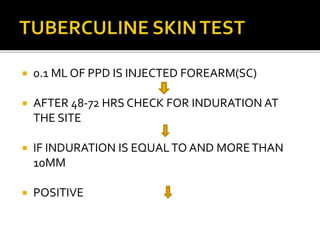
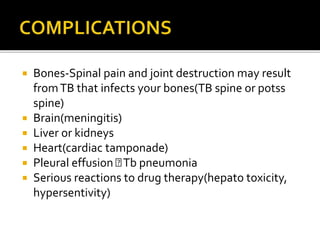
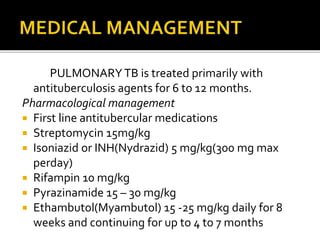
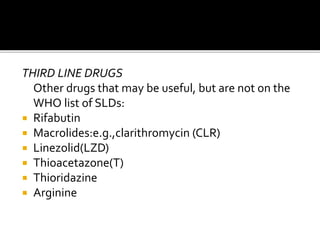
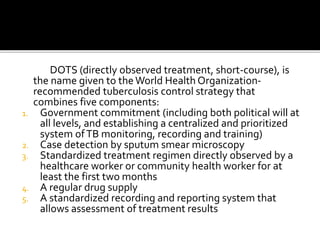
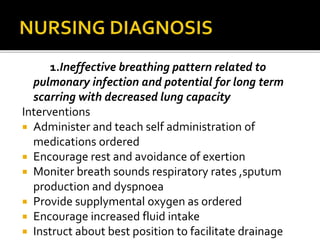
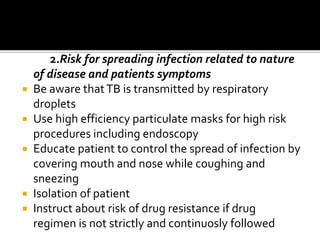
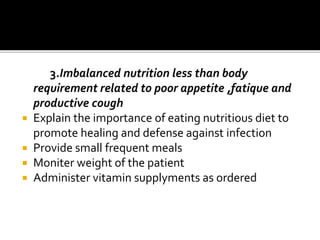
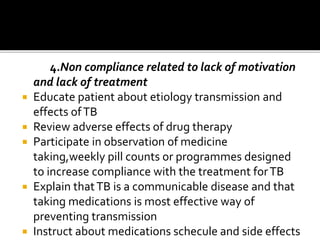
The document outlines the prevalence and transmission of pulmonary tuberculosis (TB), a significant global health issue caused primarily by Mycobacterium tuberculosis, resulting in millions of deaths annually. It discusses symptoms, diagnostic methods, treatment protocols, and the importance of adherence to medication regimens, particularly in the context of drug-resistant TB. Additionally, it emphasizes the socio-economic burden of TB and the need for increased awareness among healthcare professionals and the community.