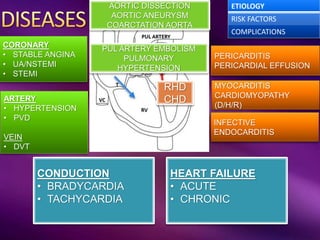
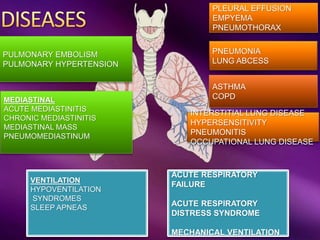
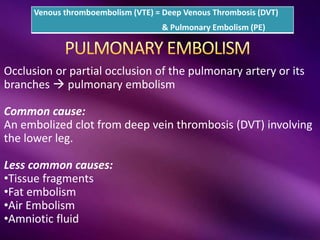
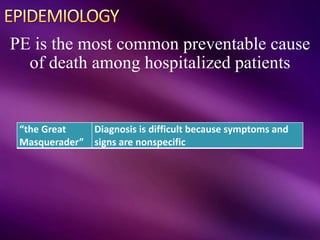
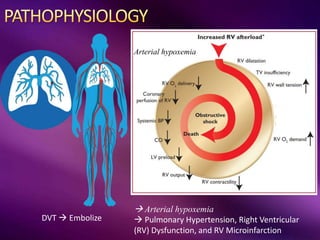
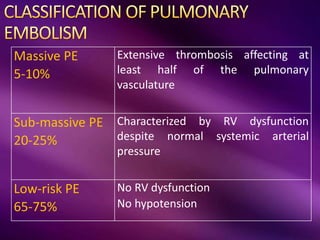
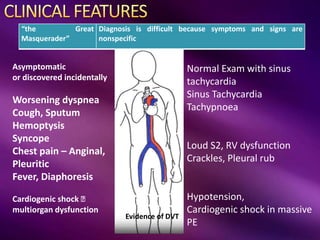
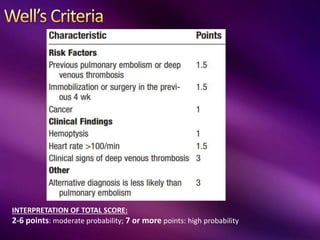
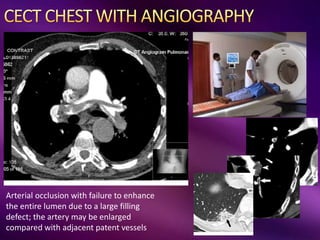
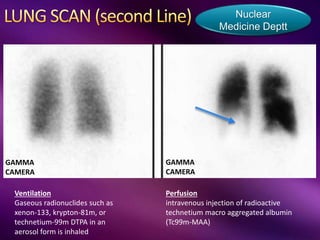
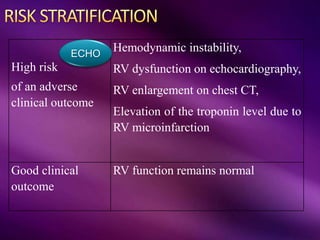
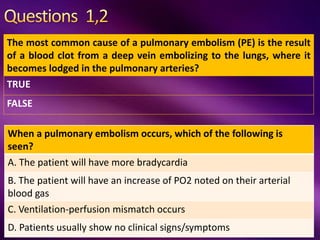
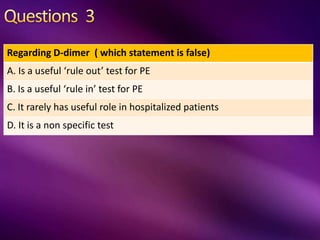
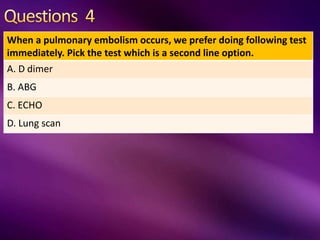
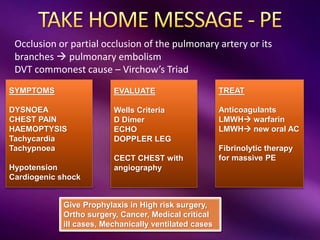
A pulmonary embolism occurs when a blood clot or other material occludes the pulmonary artery or its branches. This most commonly results from a deep vein thrombosis in the lower leg that embolizes to the lung. When a PE occurs, it causes ventilation-perfusion mismatching in the lungs. Diagnosis is difficult due to nonspecific symptoms but evaluation involves a Wells criteria assessment, D-dimer testing, echocardiogram, and CT pulmonary angiogram. Treatment consists of anticoagulation with low molecular weight heparin or novel oral anticoagulants. Fibrinolytic therapy may be used in massive PEs. Prevention focuses on prophylaxis in high risk hospitalized patients.