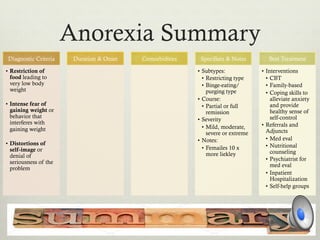
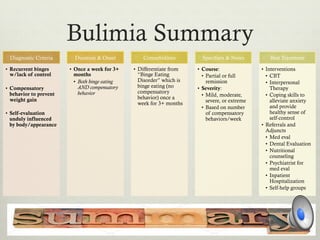
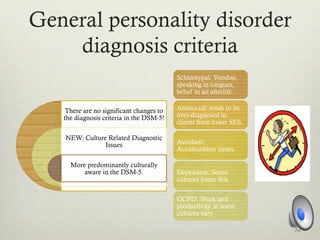
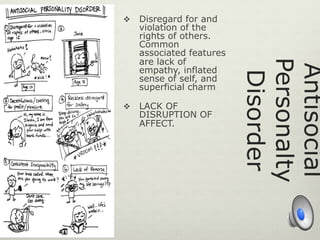
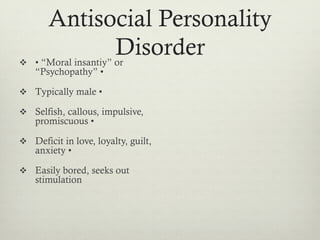
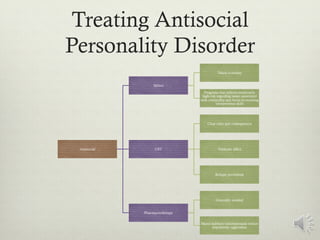
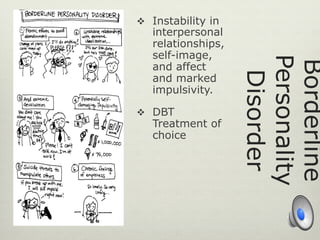
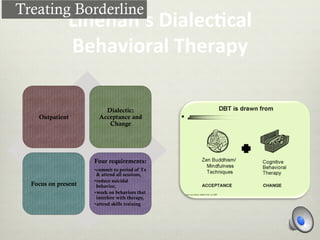
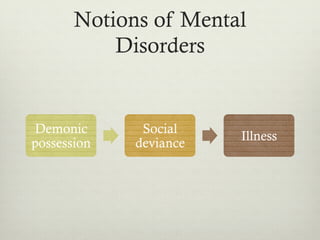
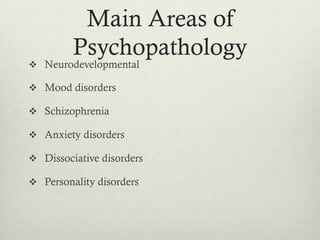
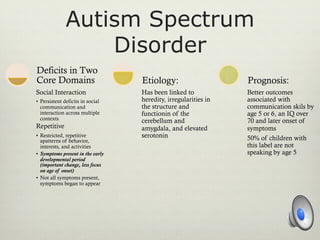
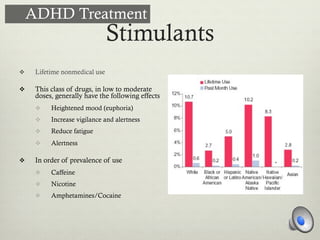
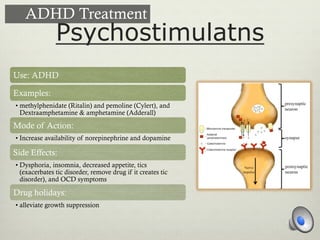
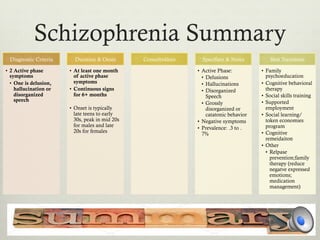
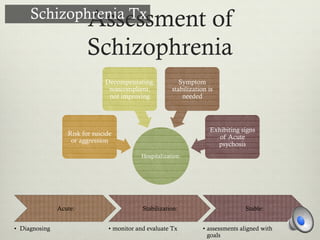
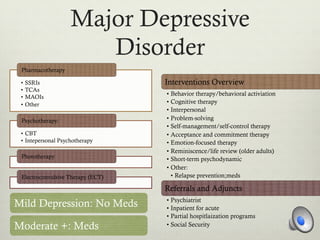
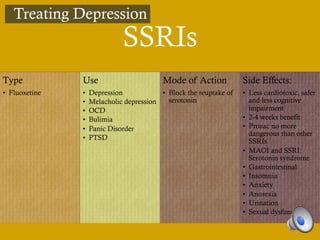
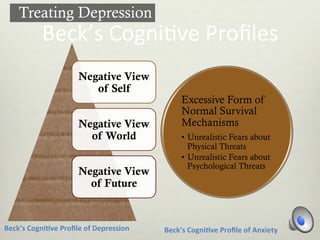
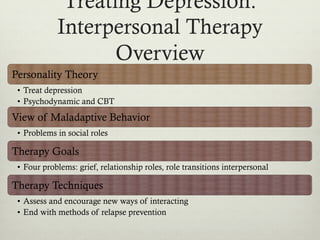
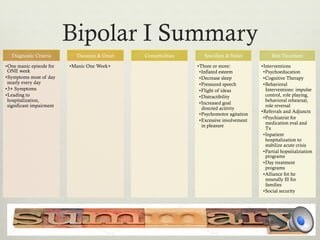
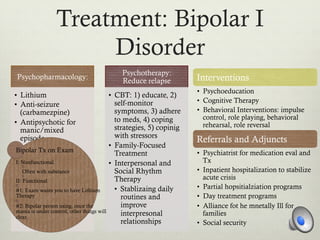
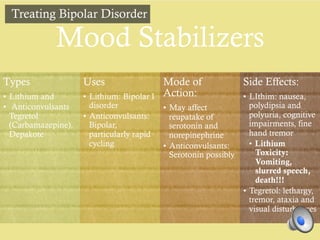
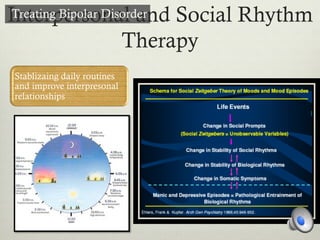
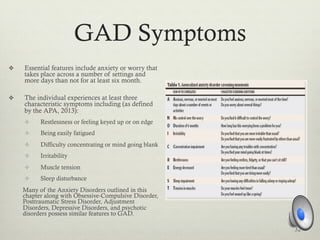
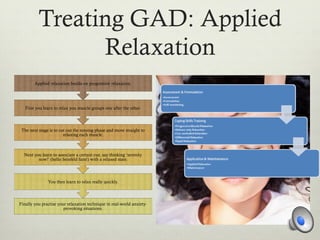
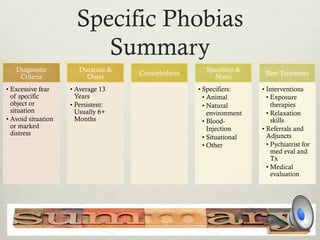
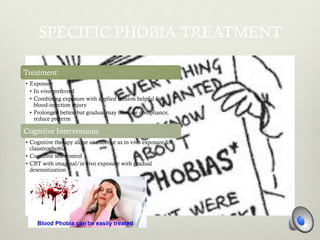
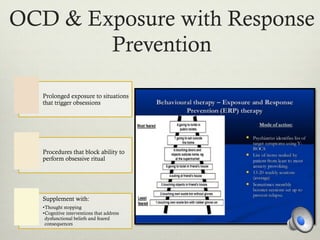
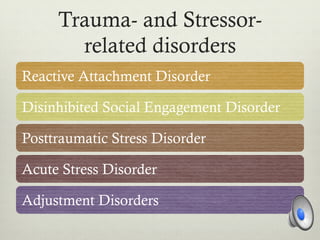
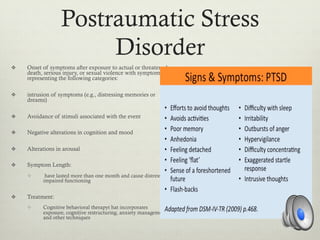
The document discusses various types of mental disorders and their treatment, covering topics such as psychopathology, neurodevelopmental disorders like autism and ADHD, mood disorders, schizophrenia, anxiety disorders, and more. For each topic, diagnostic criteria and treatment options are presented, including pharmacological and psychotherapeutic approaches. The goal of treatment is symptom management and improving functioning for those suffering from mental illnesses.




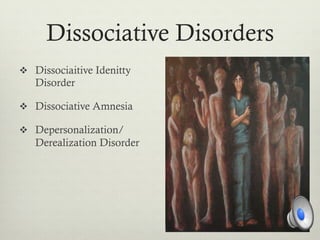
![Causes of Dissociative
Disorders?
v Abuse +[Plus]
v Abuse plus an ability to put onself in a hypnotic
trance to cope with abusive situations](https://image.slidesharecdn.com/psychopathologyslideshare-150721015626-lva1-app6891/85/Psychopathology-46-320.jpg)