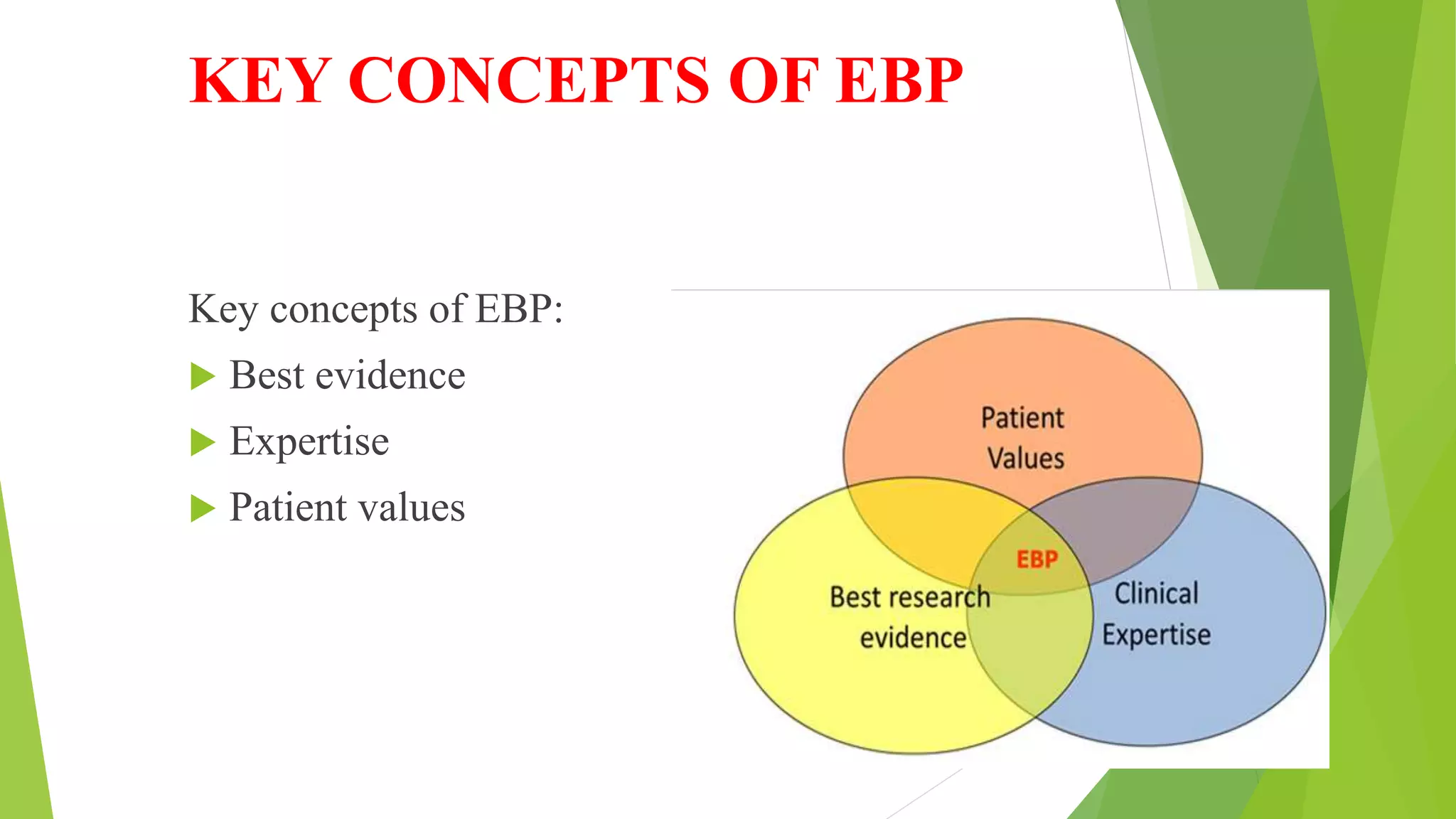
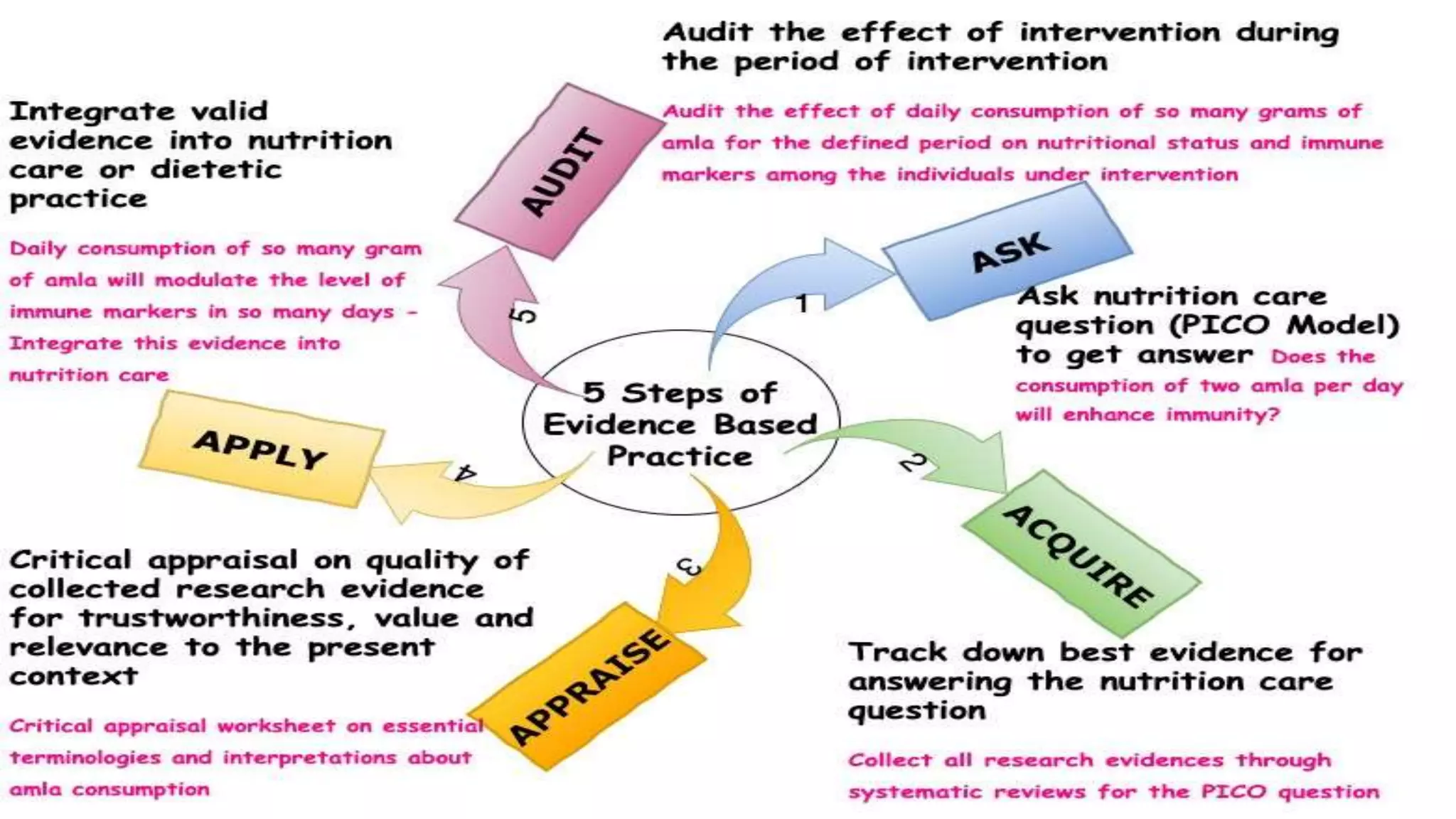
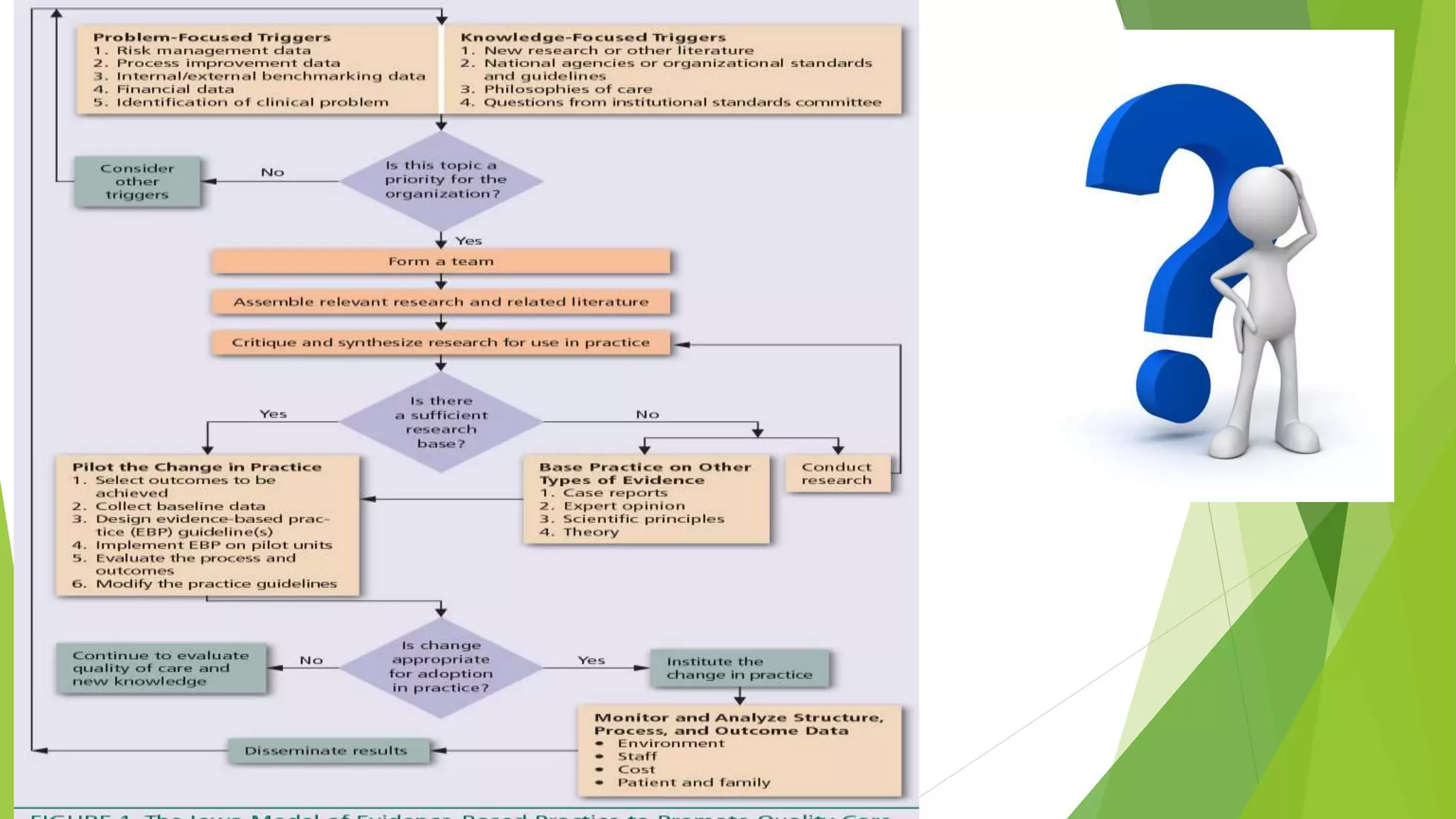
The document discusses evidence-based practice (EBP) in nursing. It defines EBP as using the best available research evidence, clinical expertise, and patient values to make decisions about patient care. The document outlines the steps of EBP, which include asking questions, finding evidence, appraising evidence, applying it to practice, and assessing outcomes. It also discusses popular EBP models like the Johns Hopkins Nursing EBP model and the Iowa model. Barriers to EBP and its advantages are summarized as well.