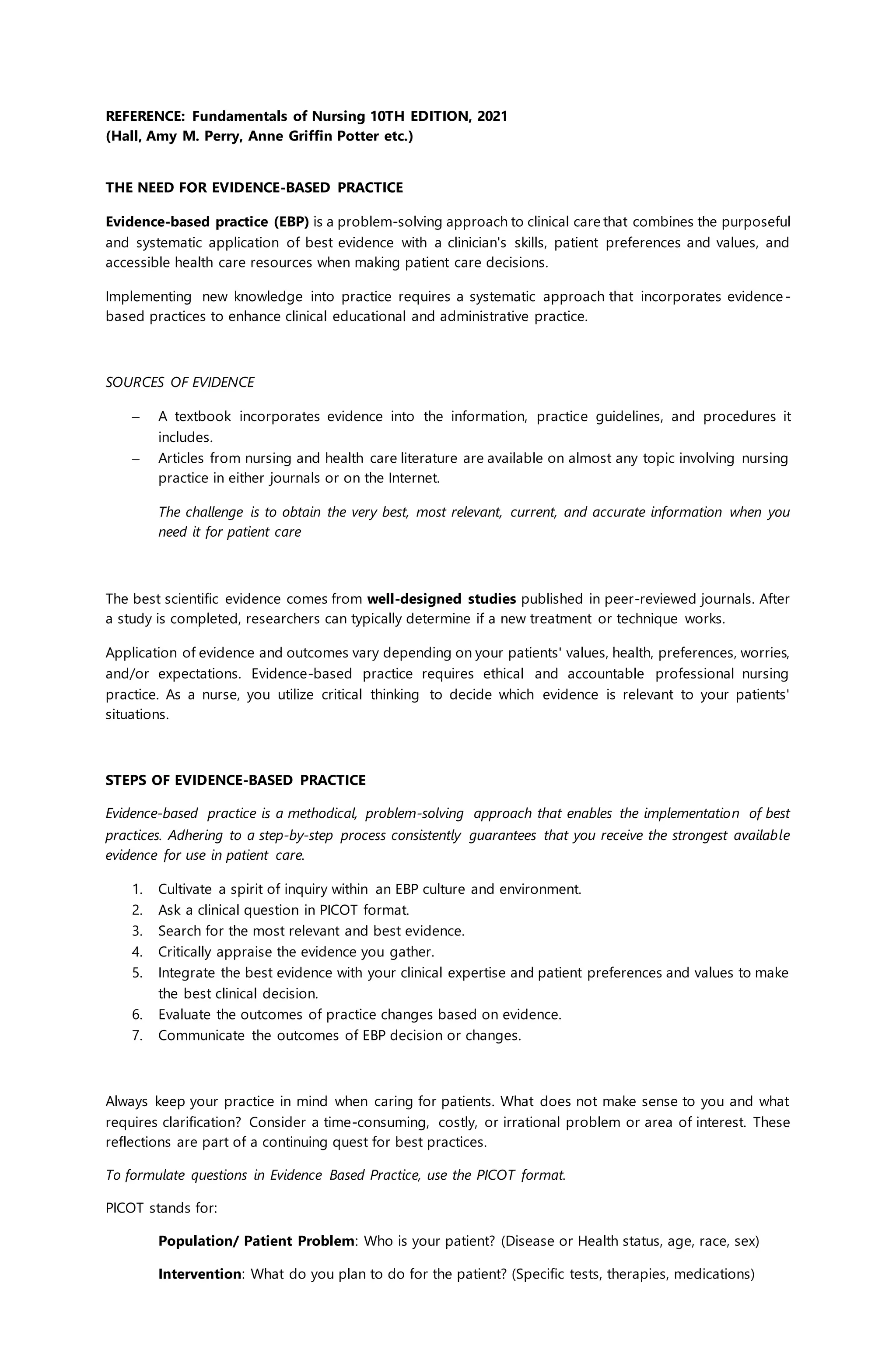
The document outlines the principles and steps of evidence-based practice (EBP) in nursing, emphasizing its importance in combining clinical expertise with the best available evidence and patient preferences to make informed care decisions. It describes the systematic approach to integrating research into practice, defining steps such as formulating clinical questions using PICOT format, searching for and appraising evidence, and evaluating the outcomes of decisions. Additionally, it highlights the relationship of EBP with nursing research and performance improvement, reinforcing the need for continual adaptation and integration of evidence in clinical practice.