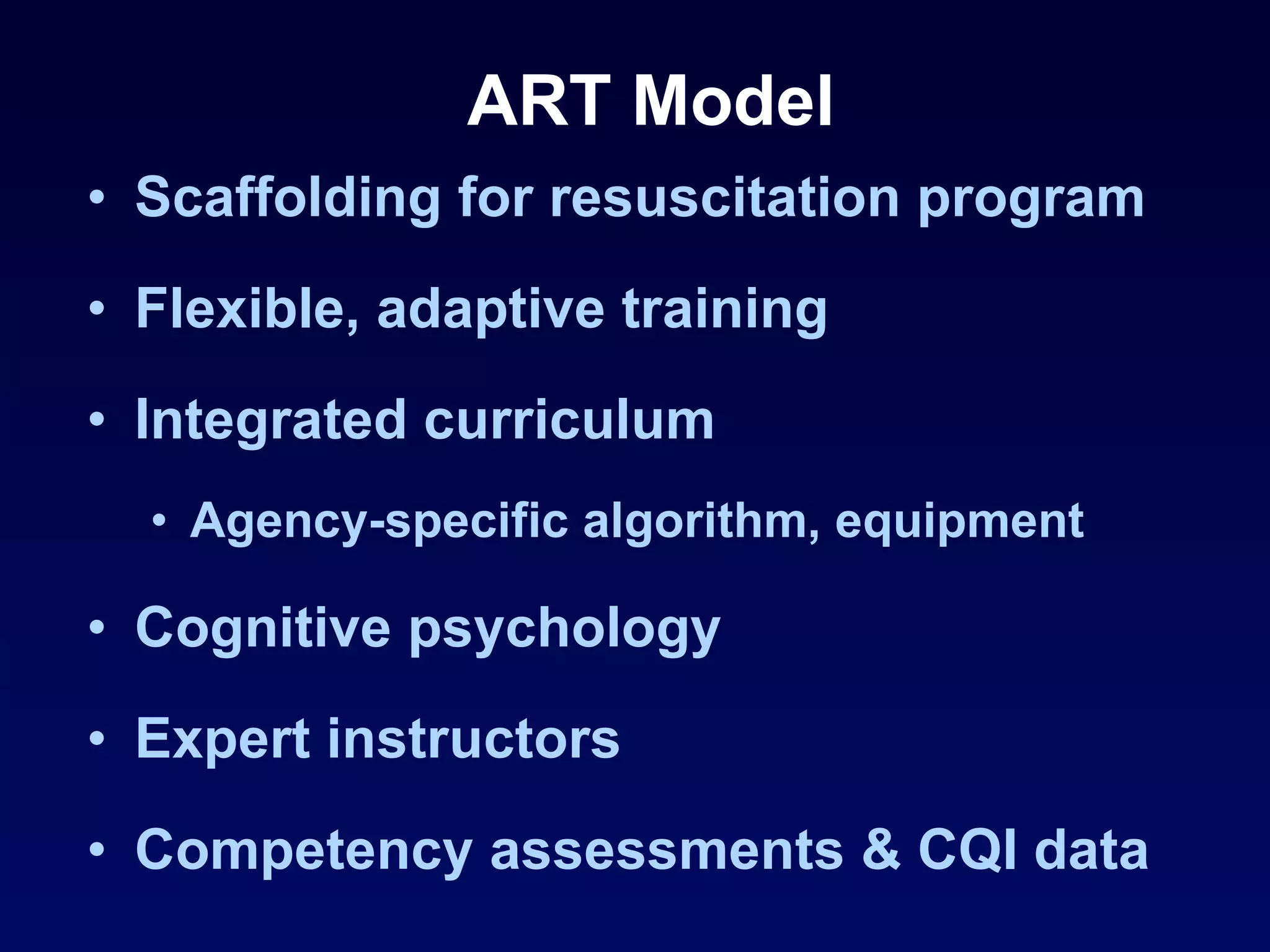
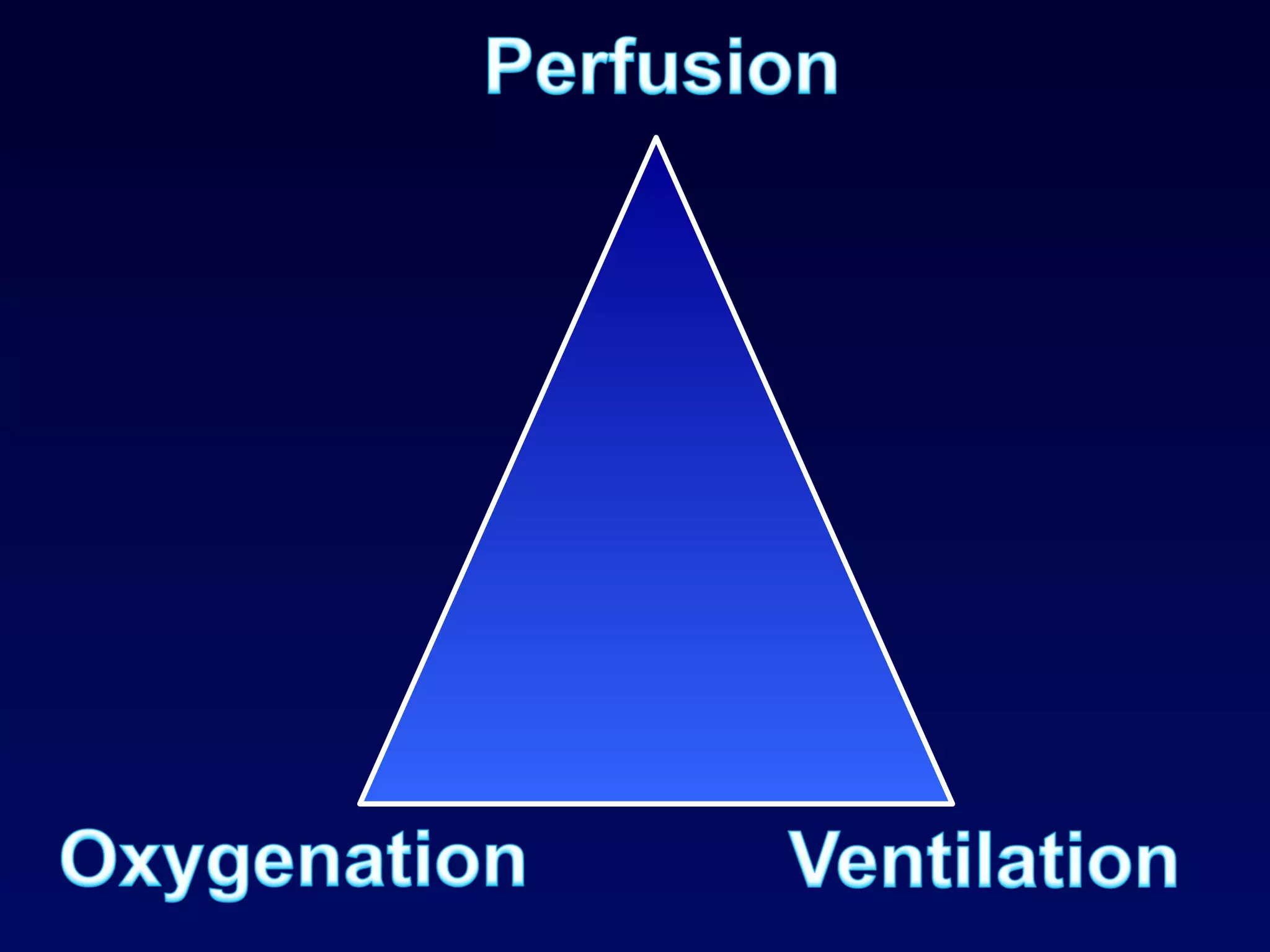
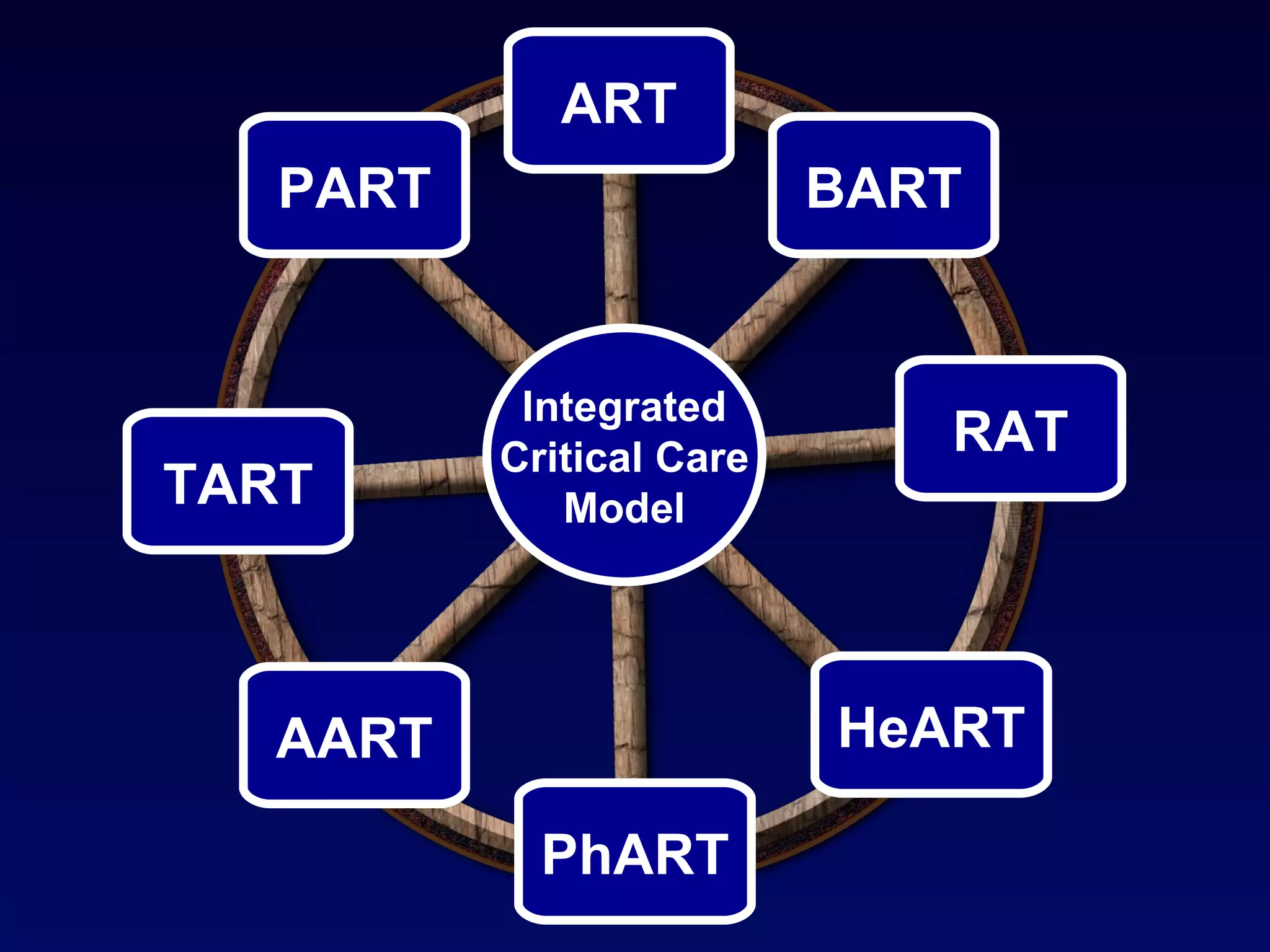
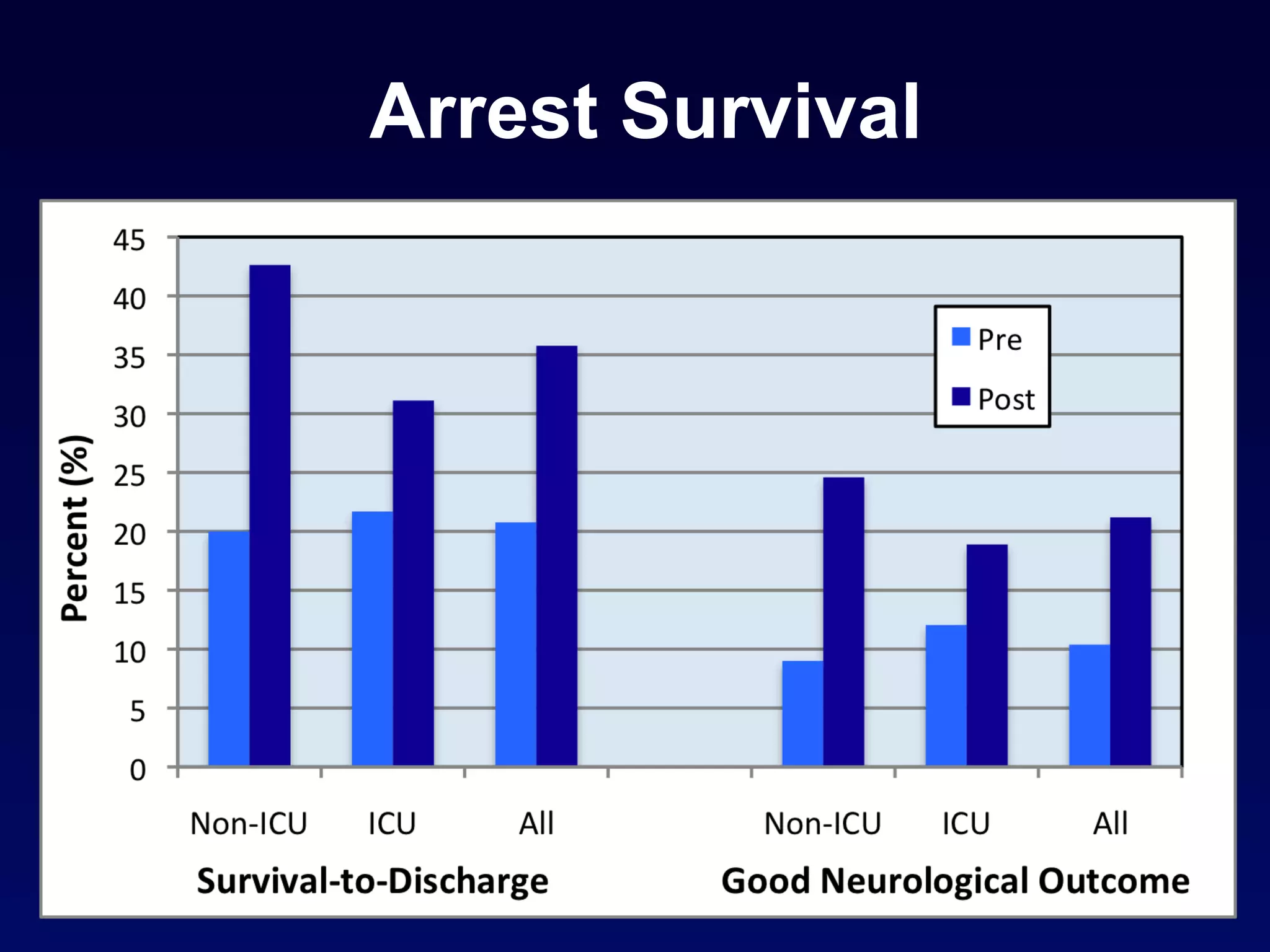
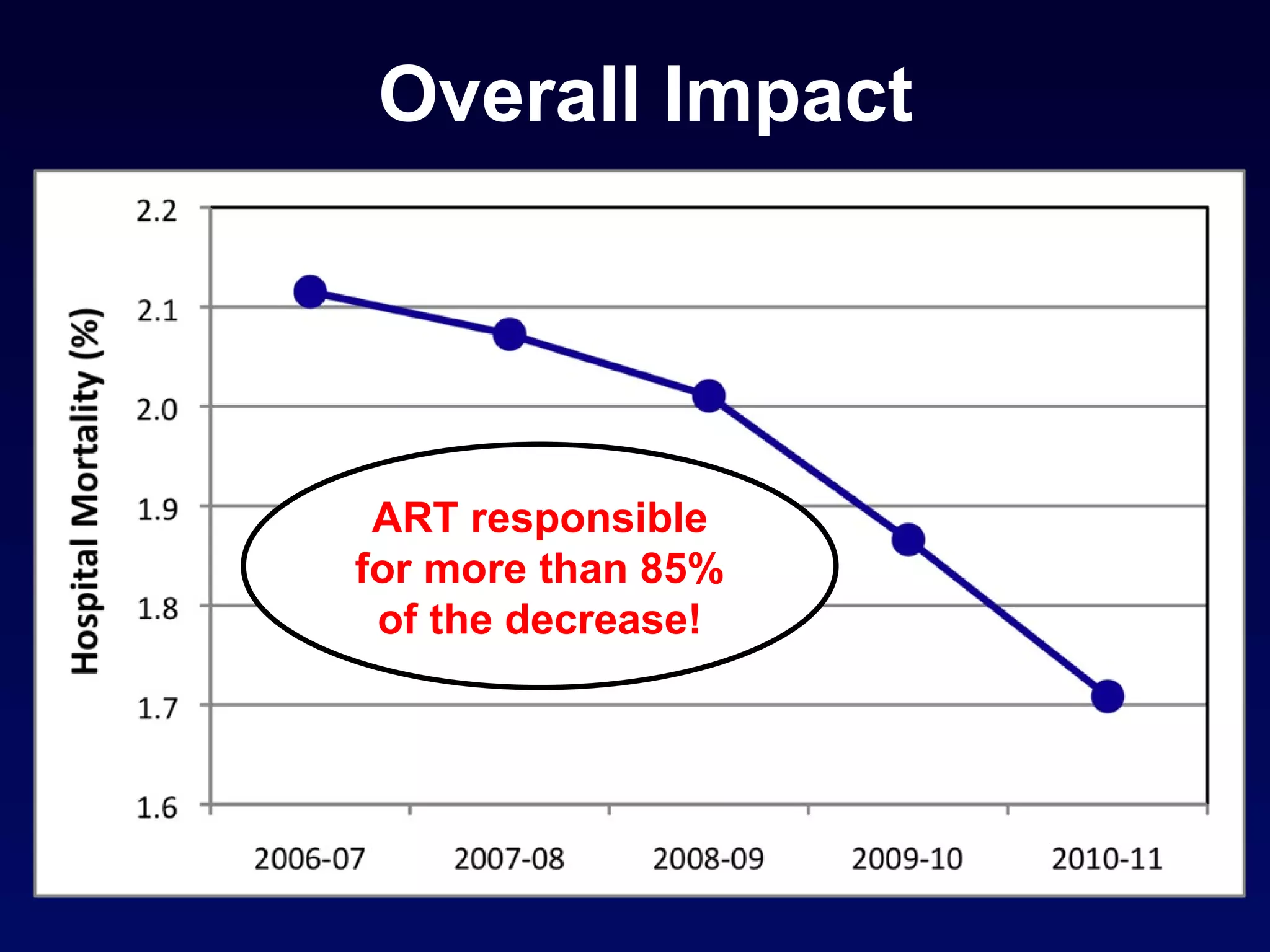
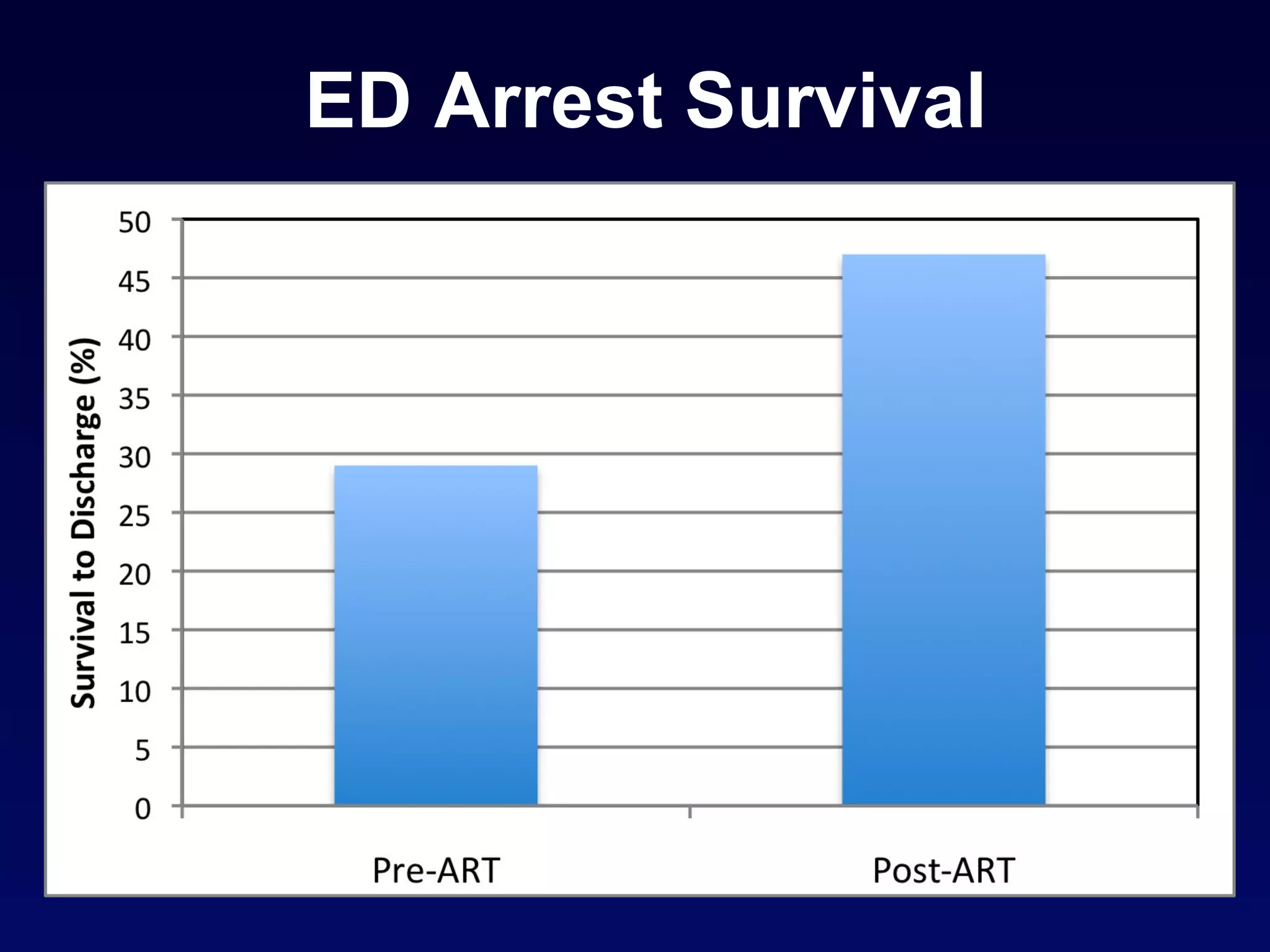
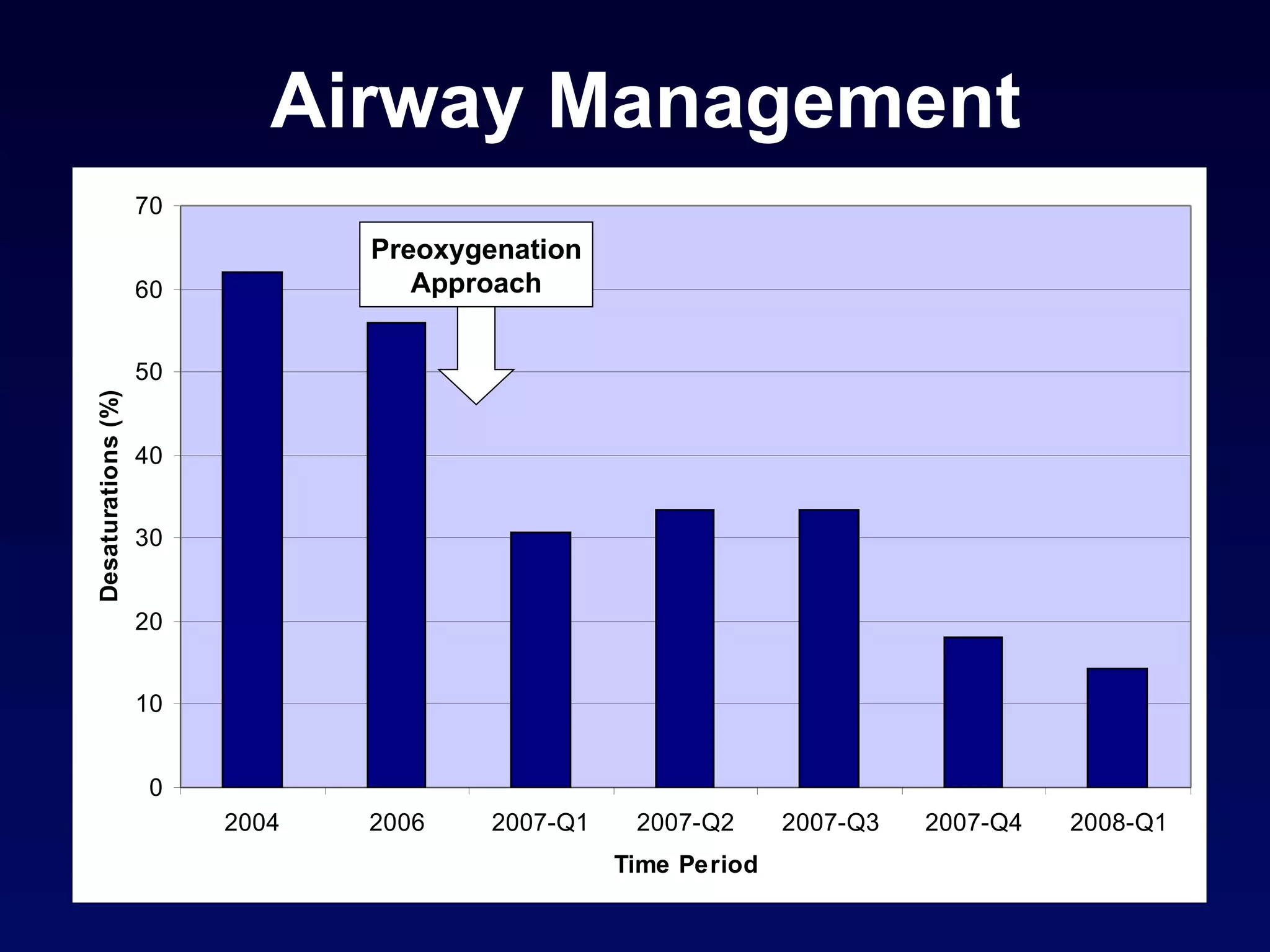
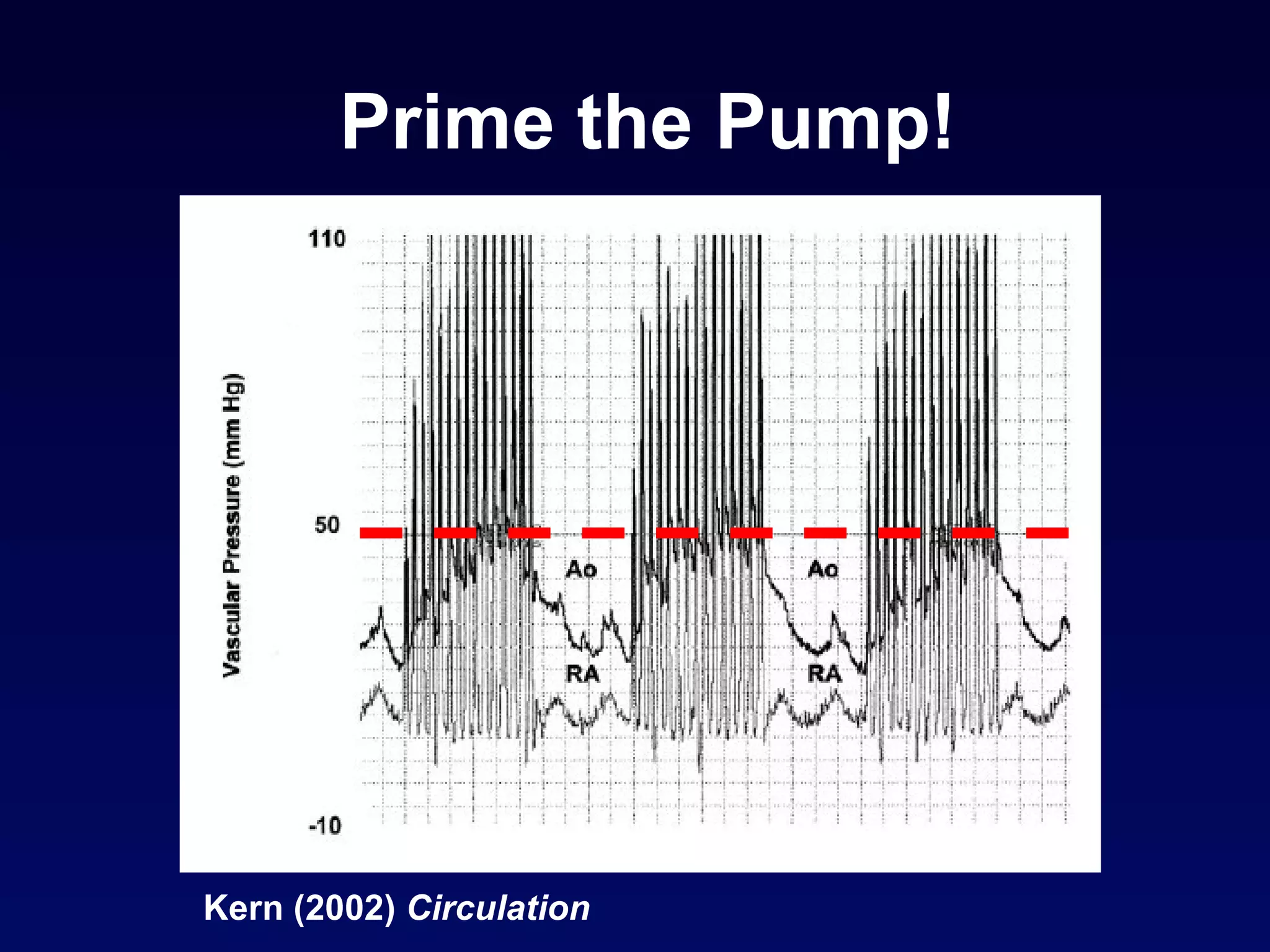
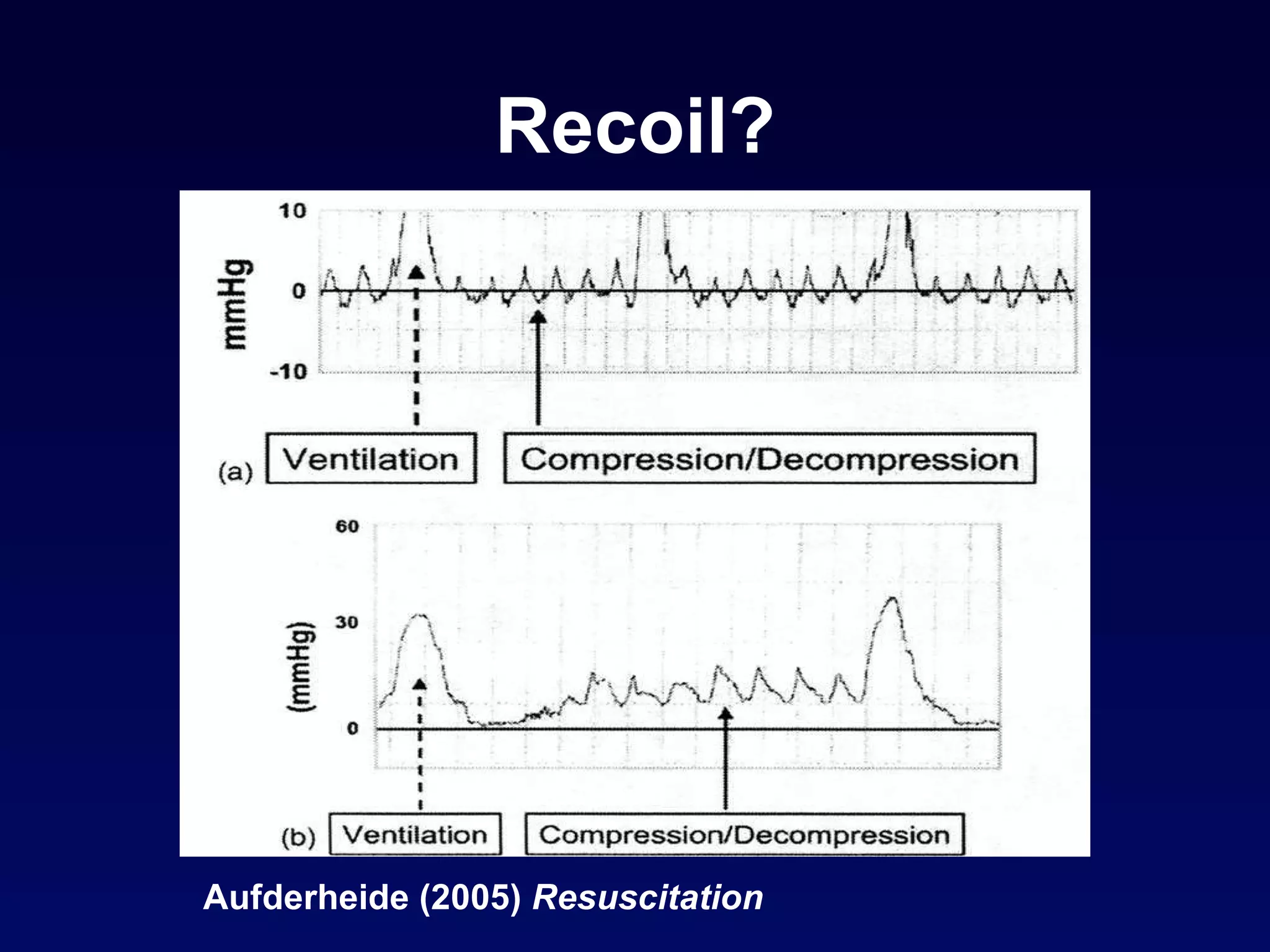
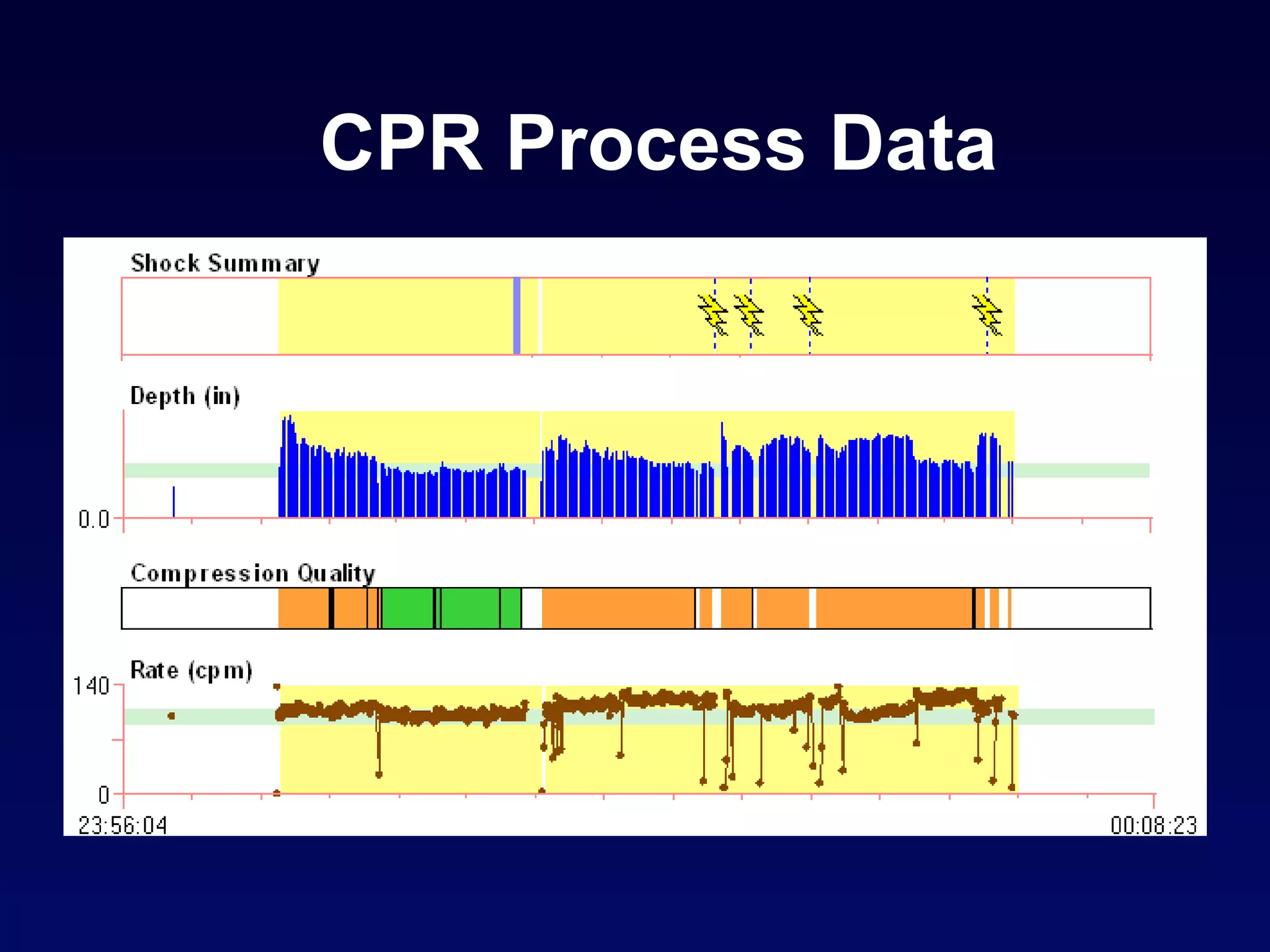
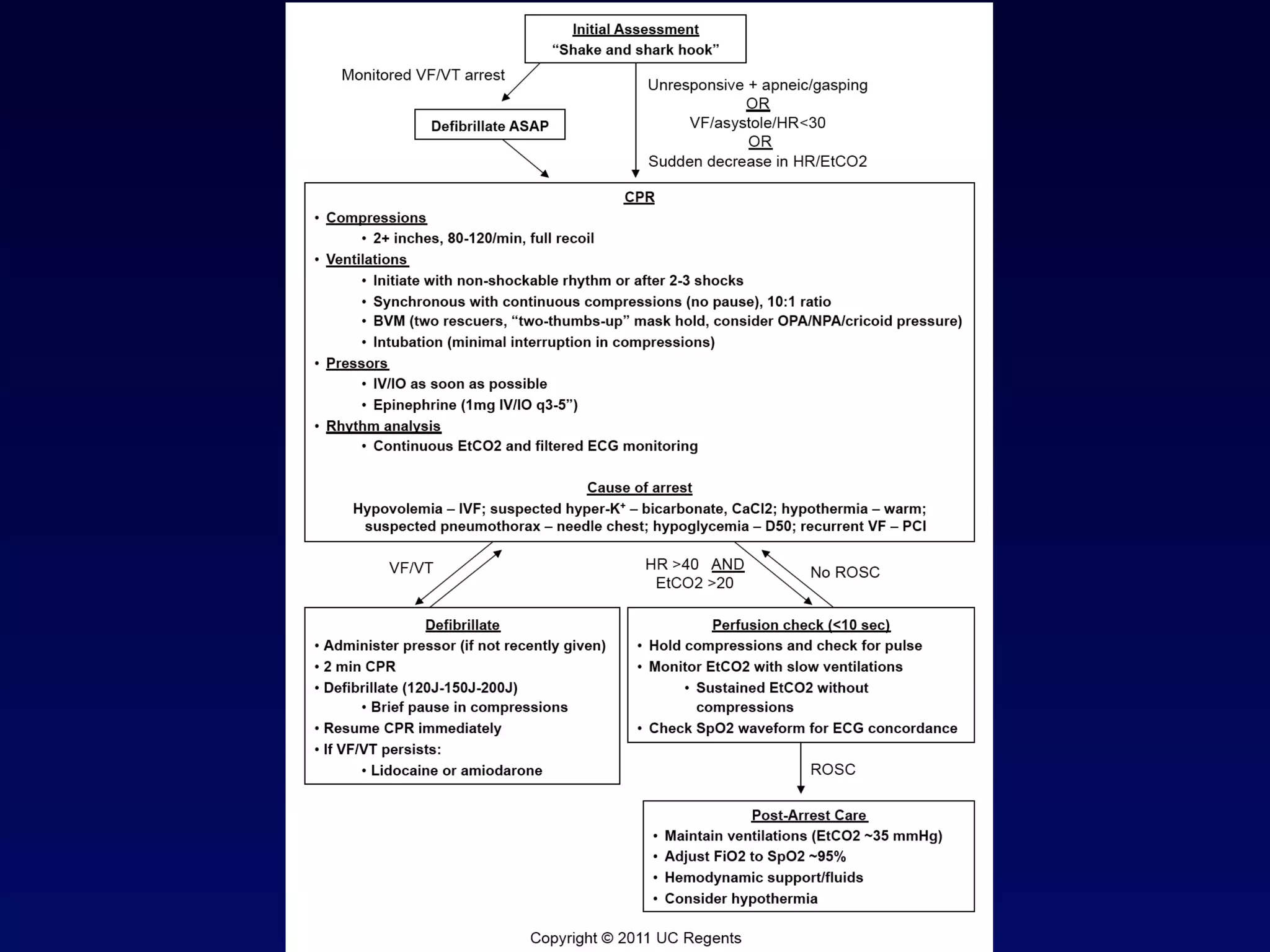
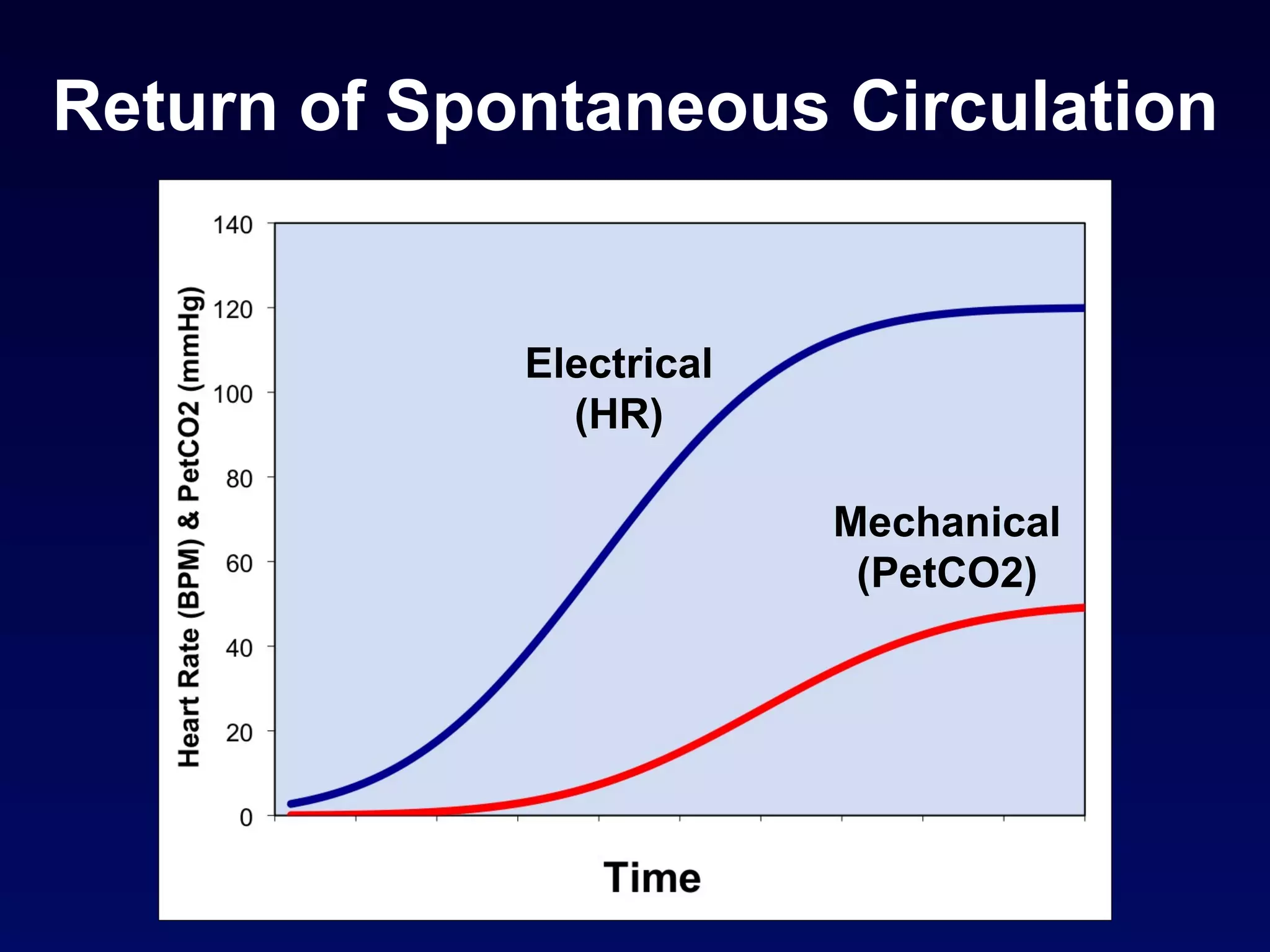
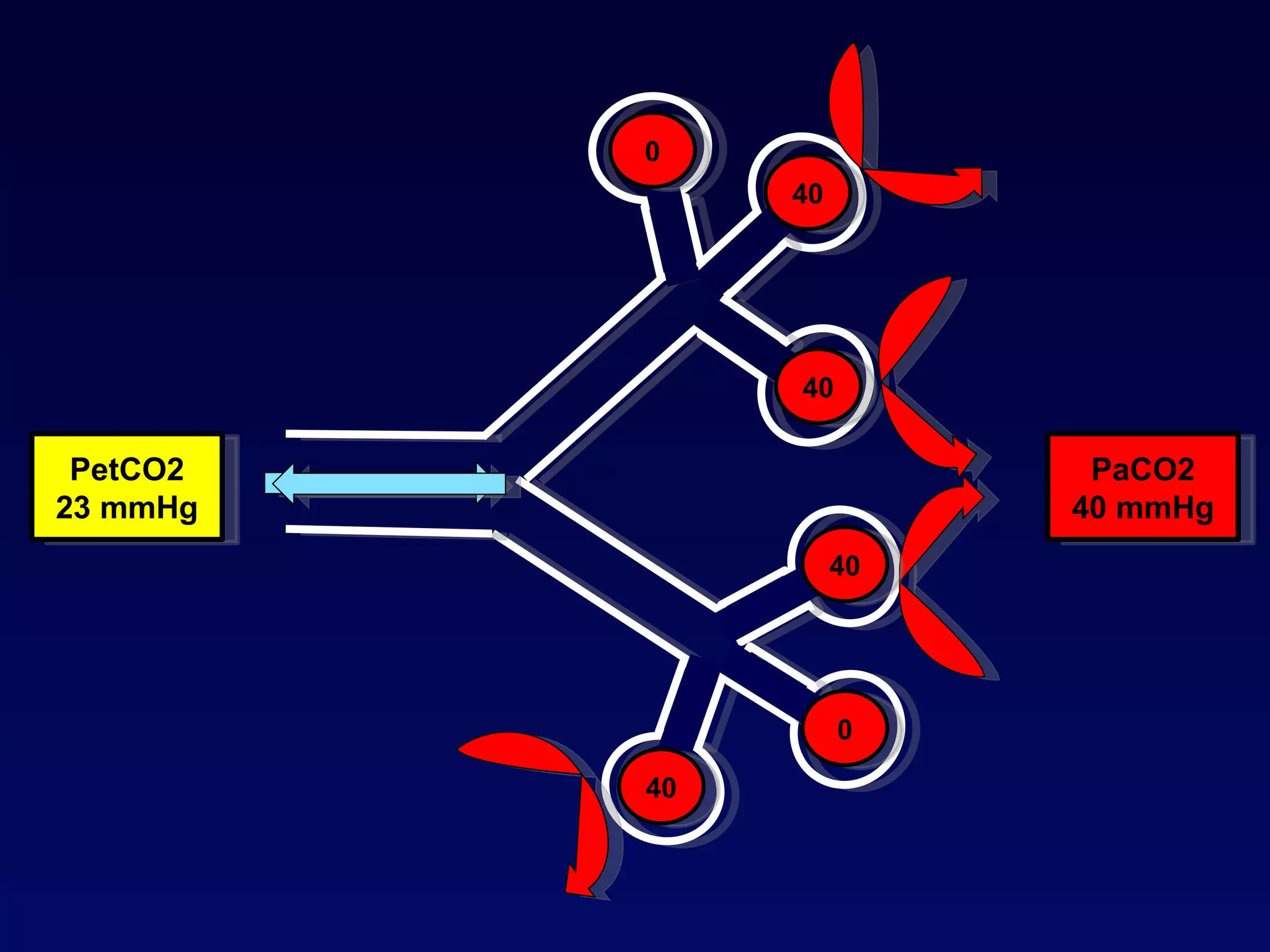
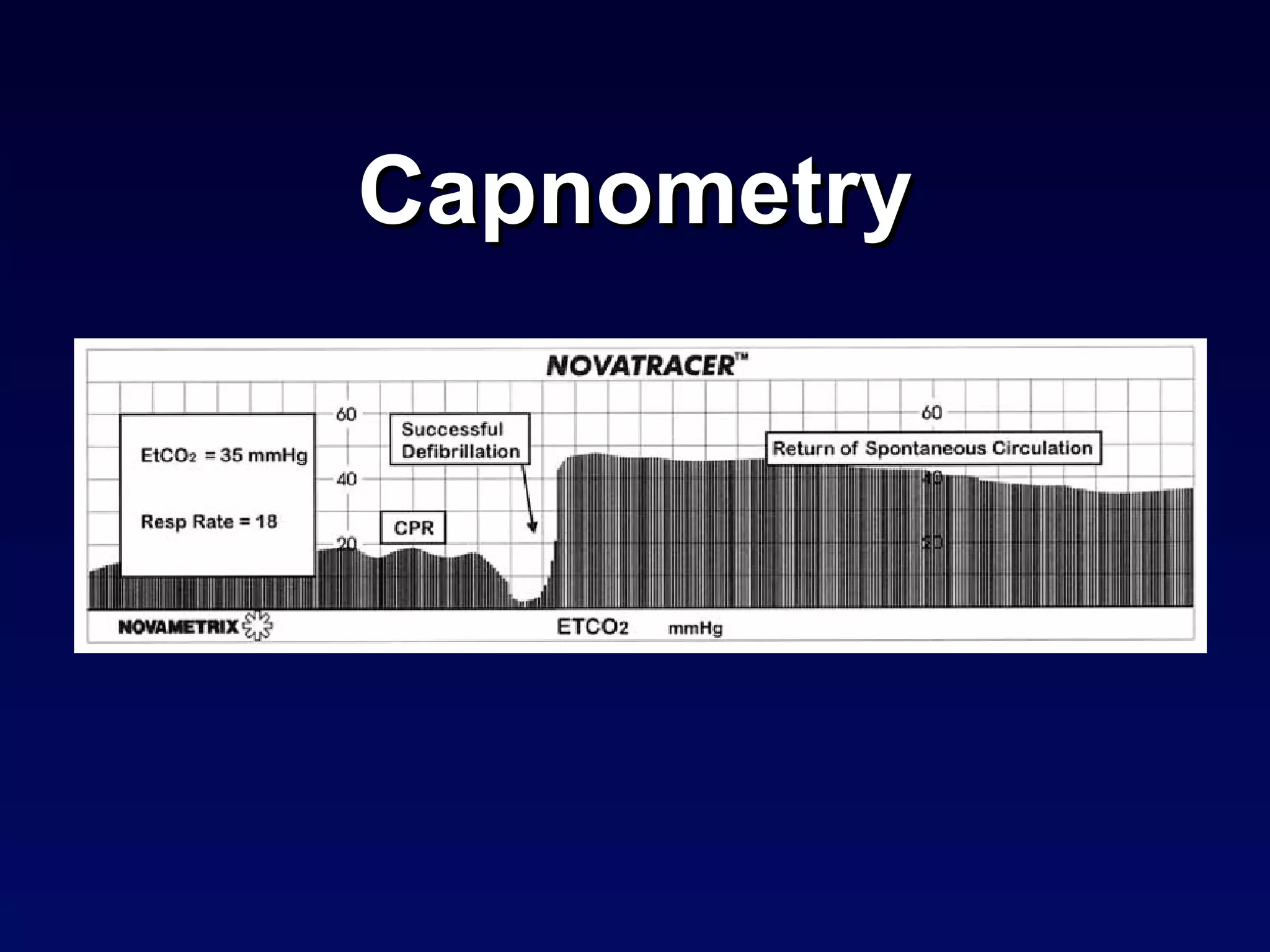
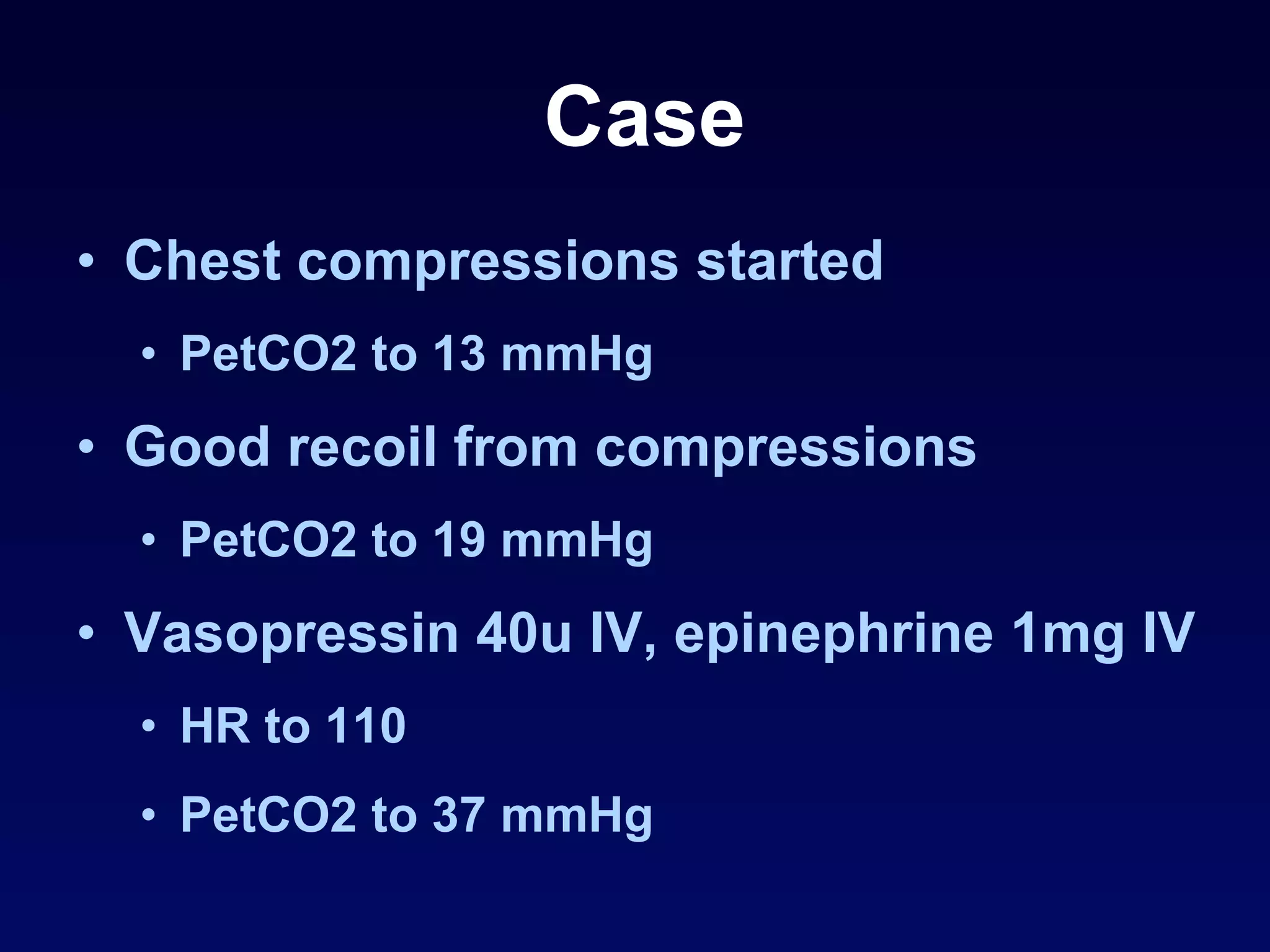
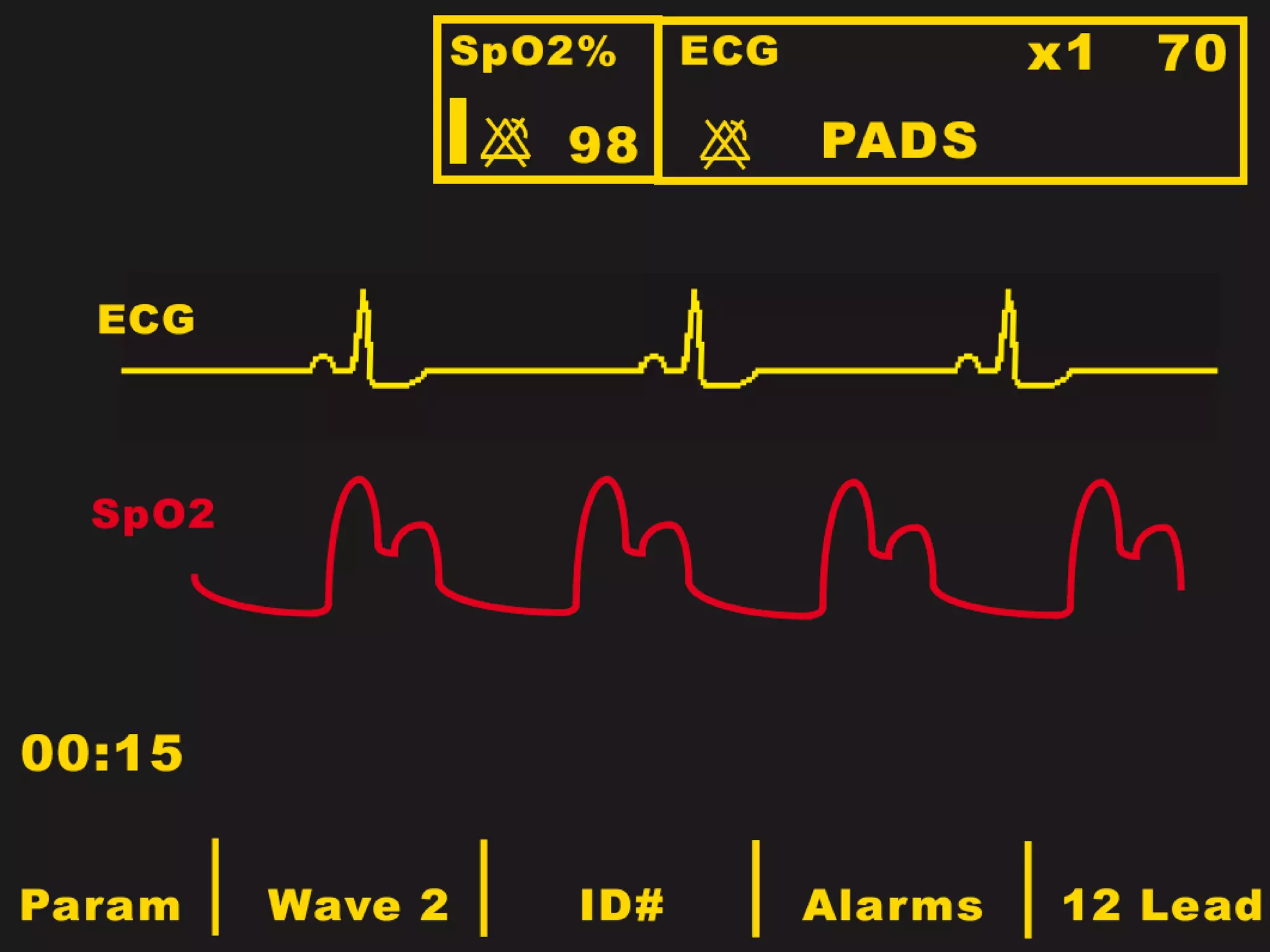
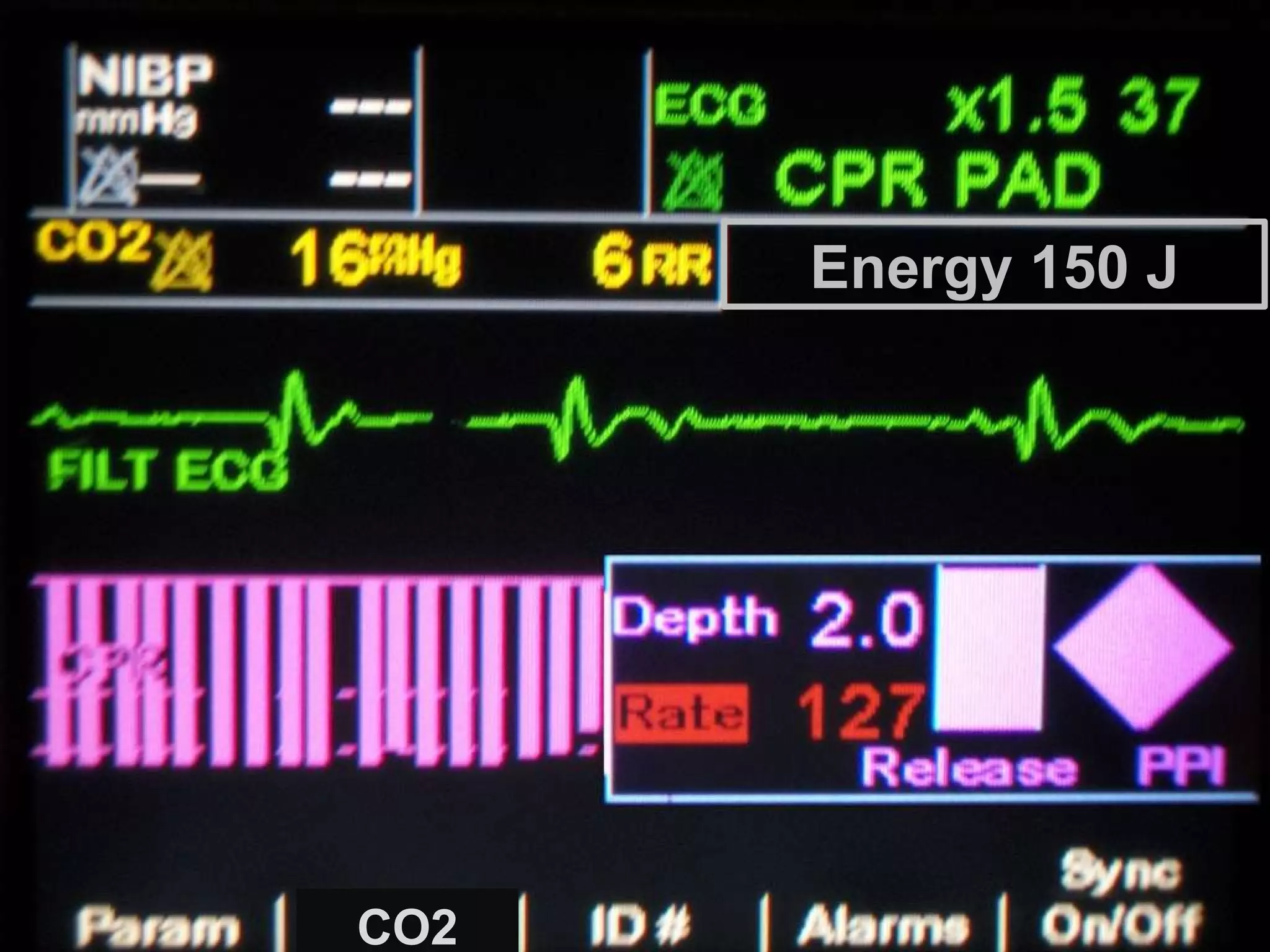
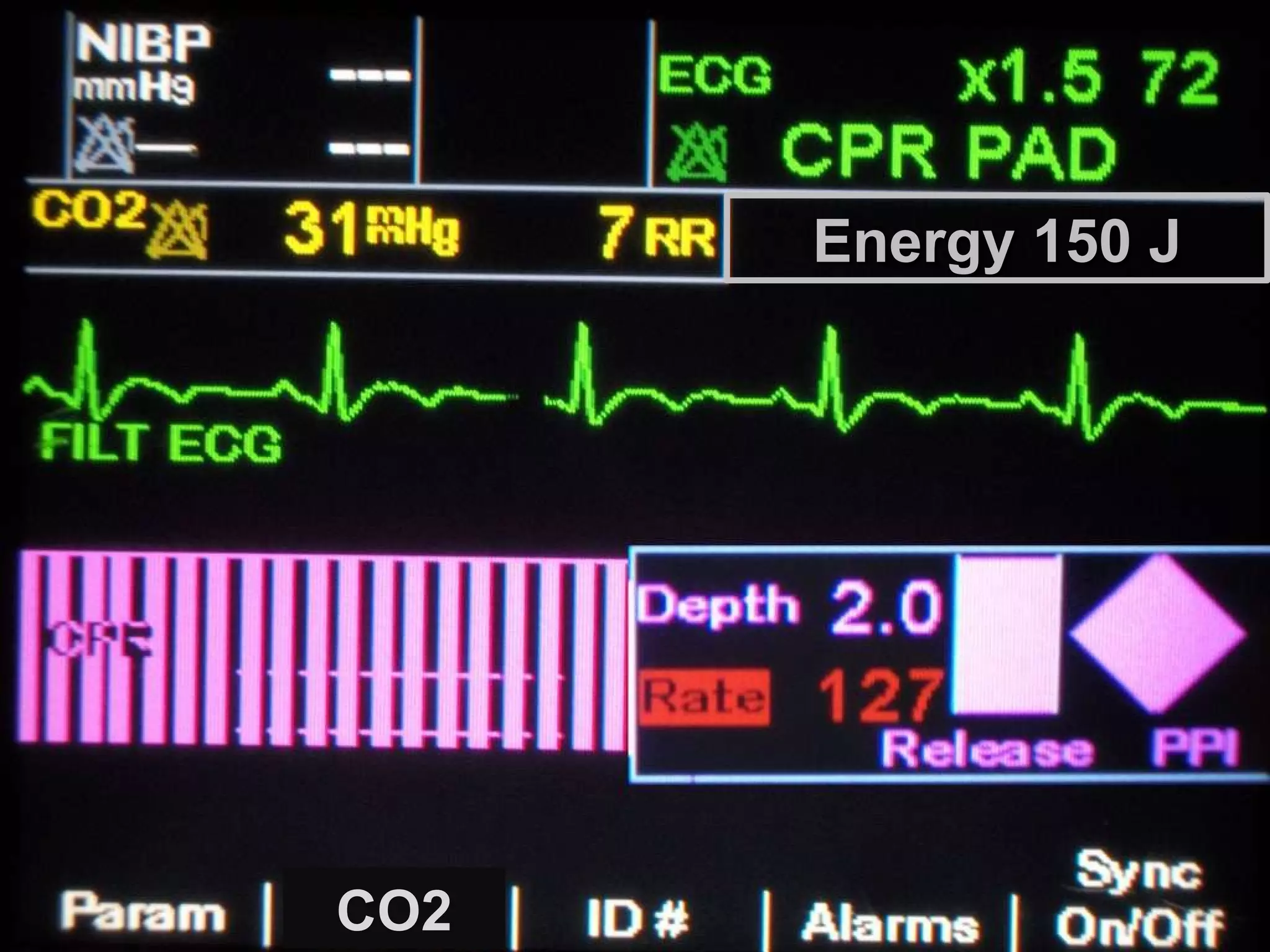
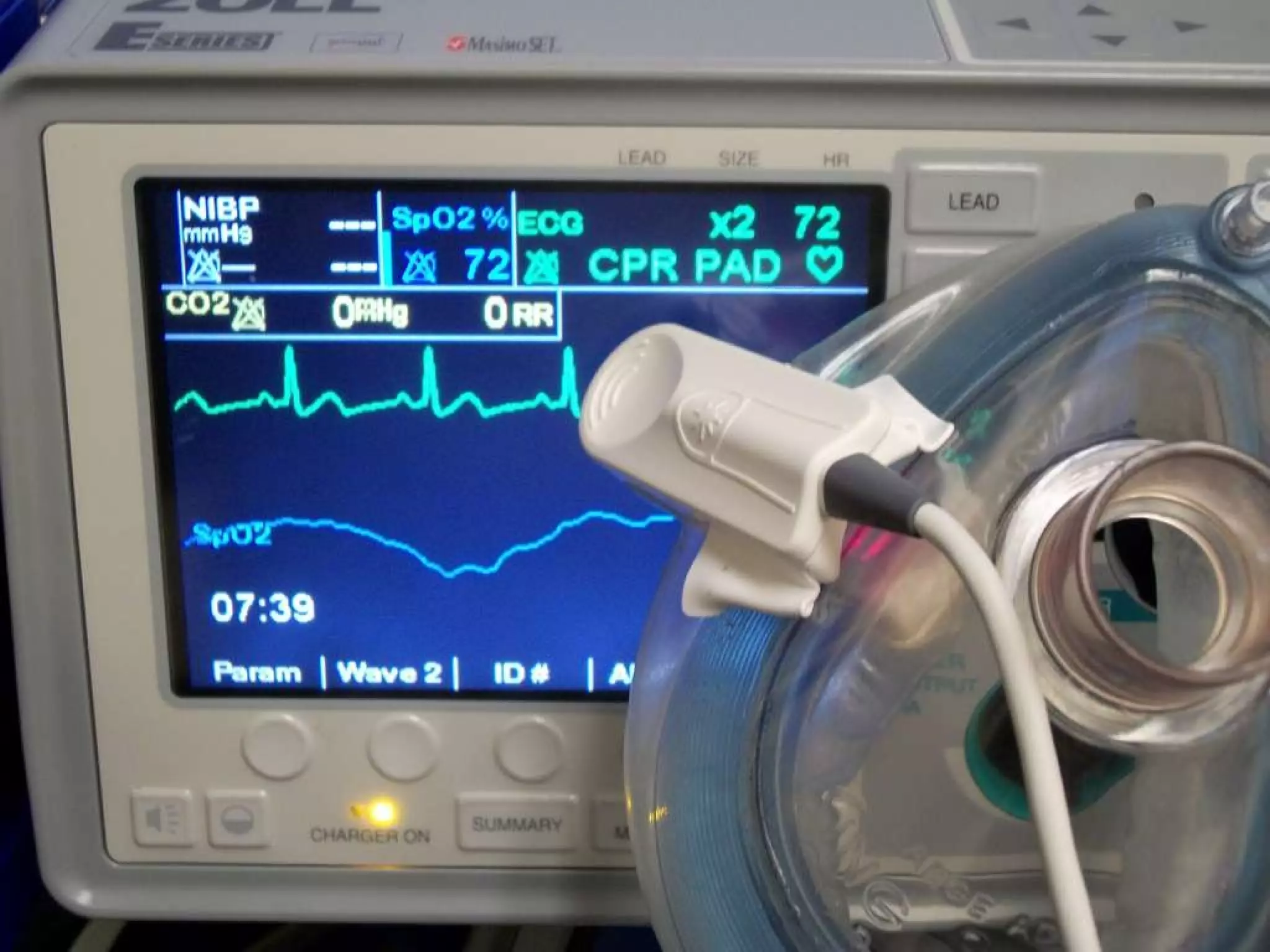
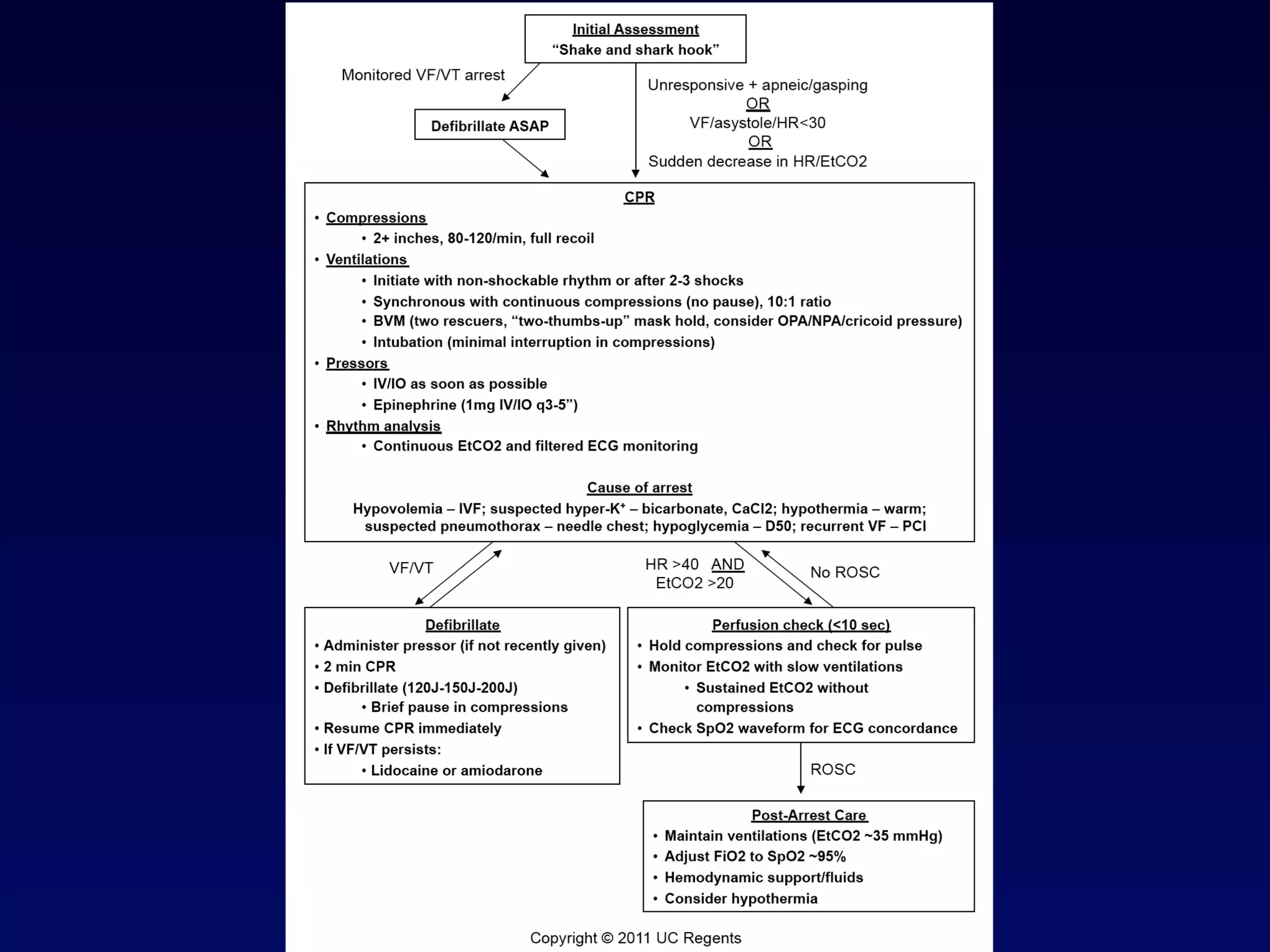
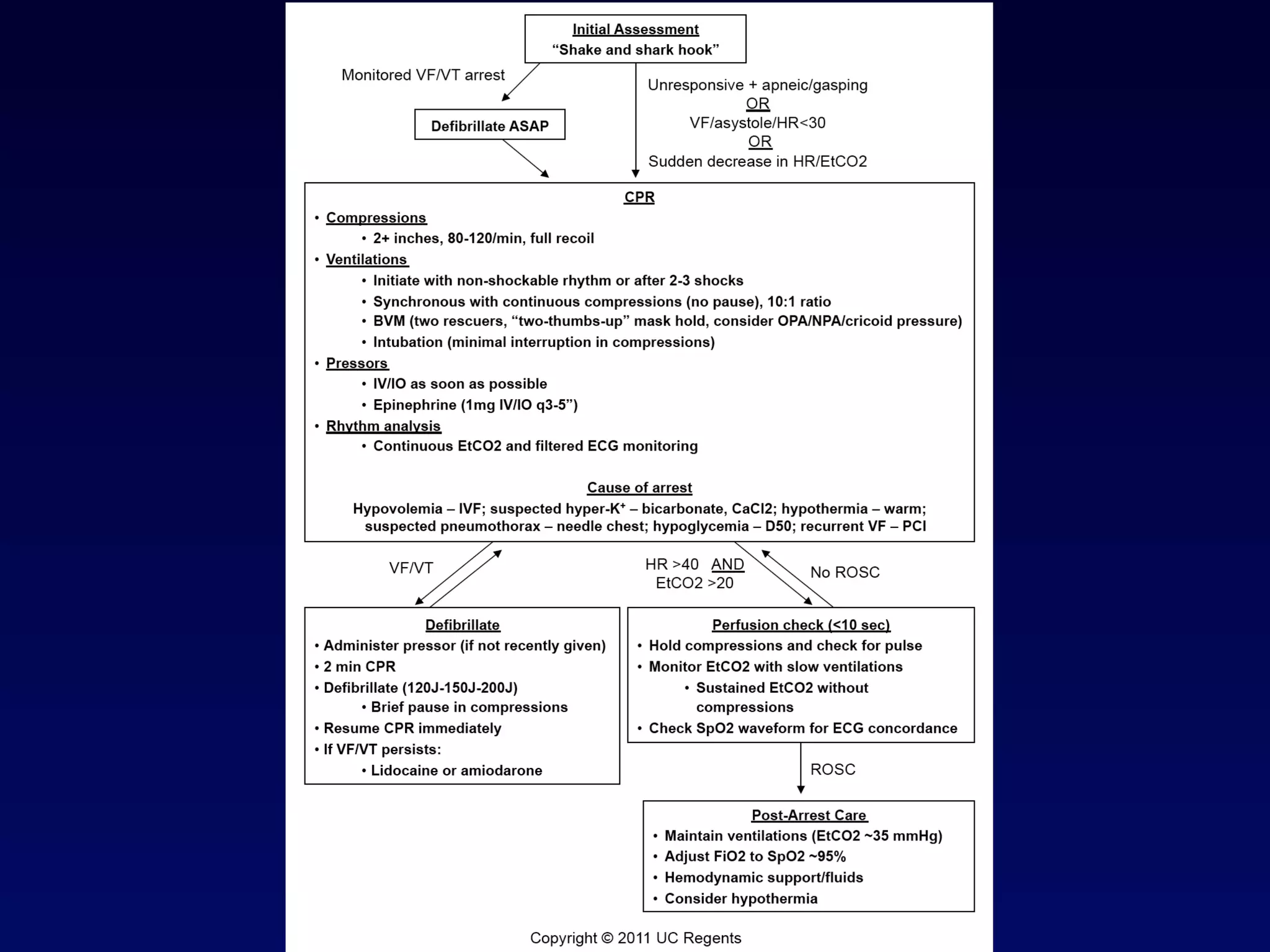
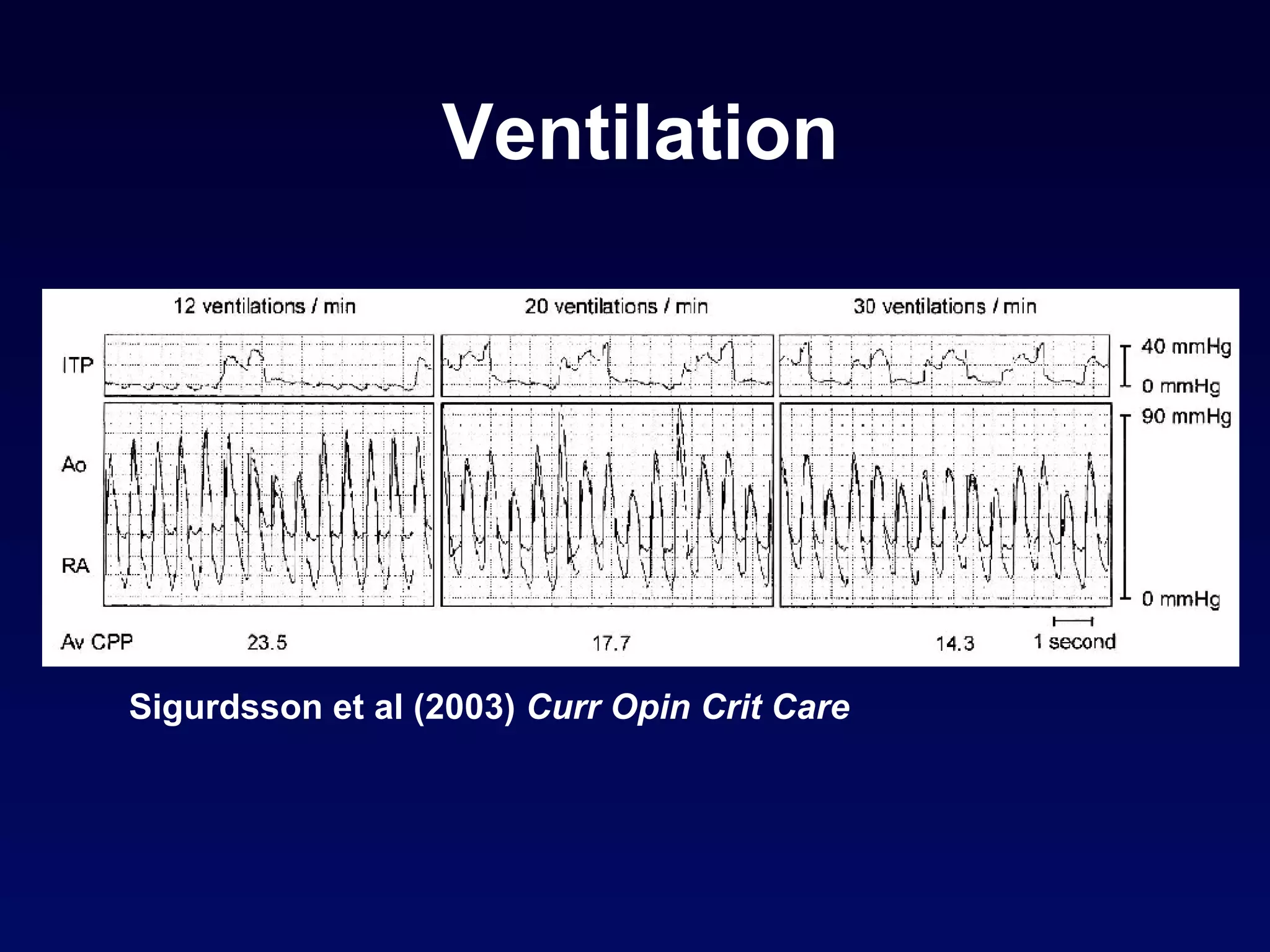
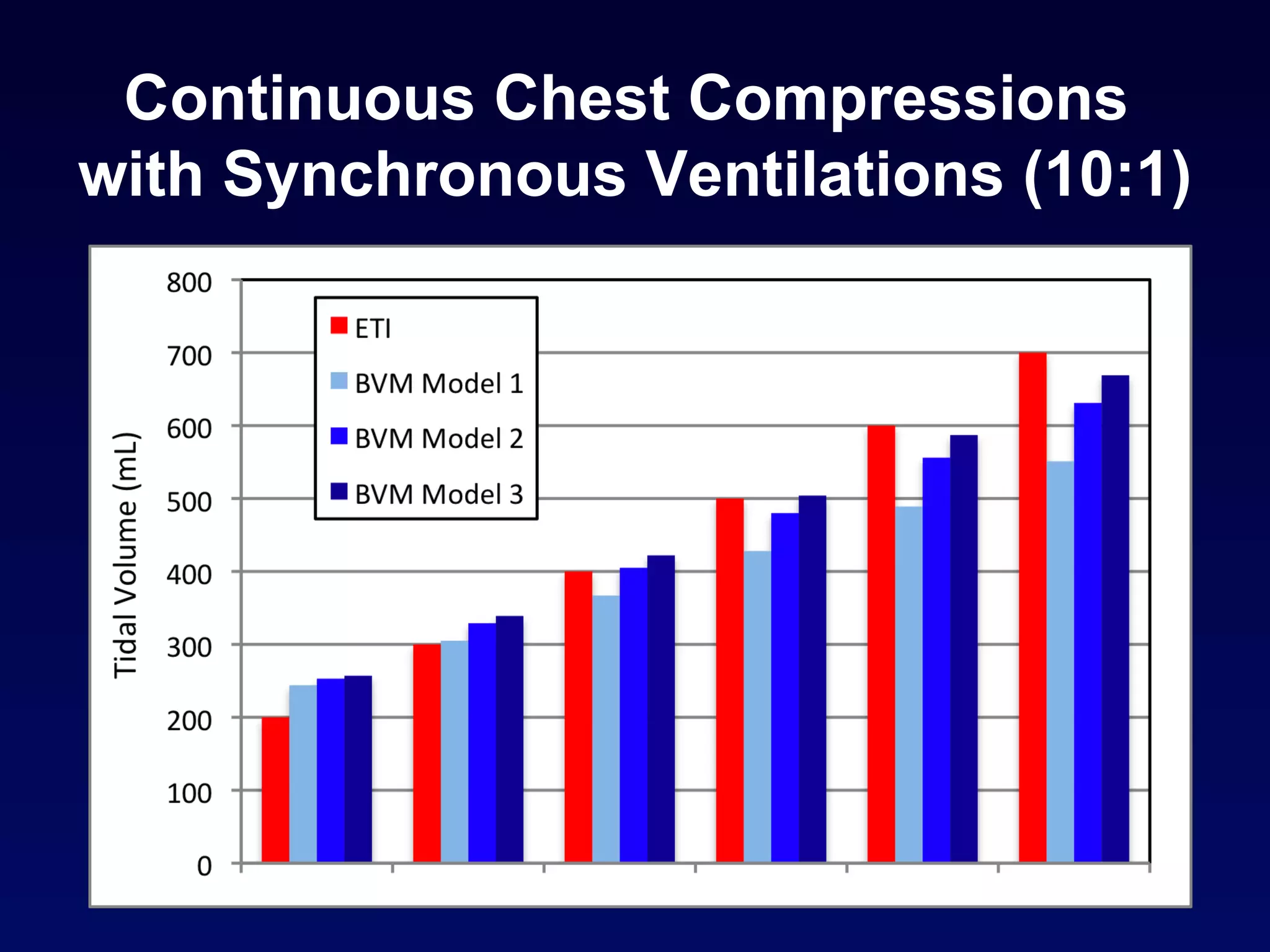
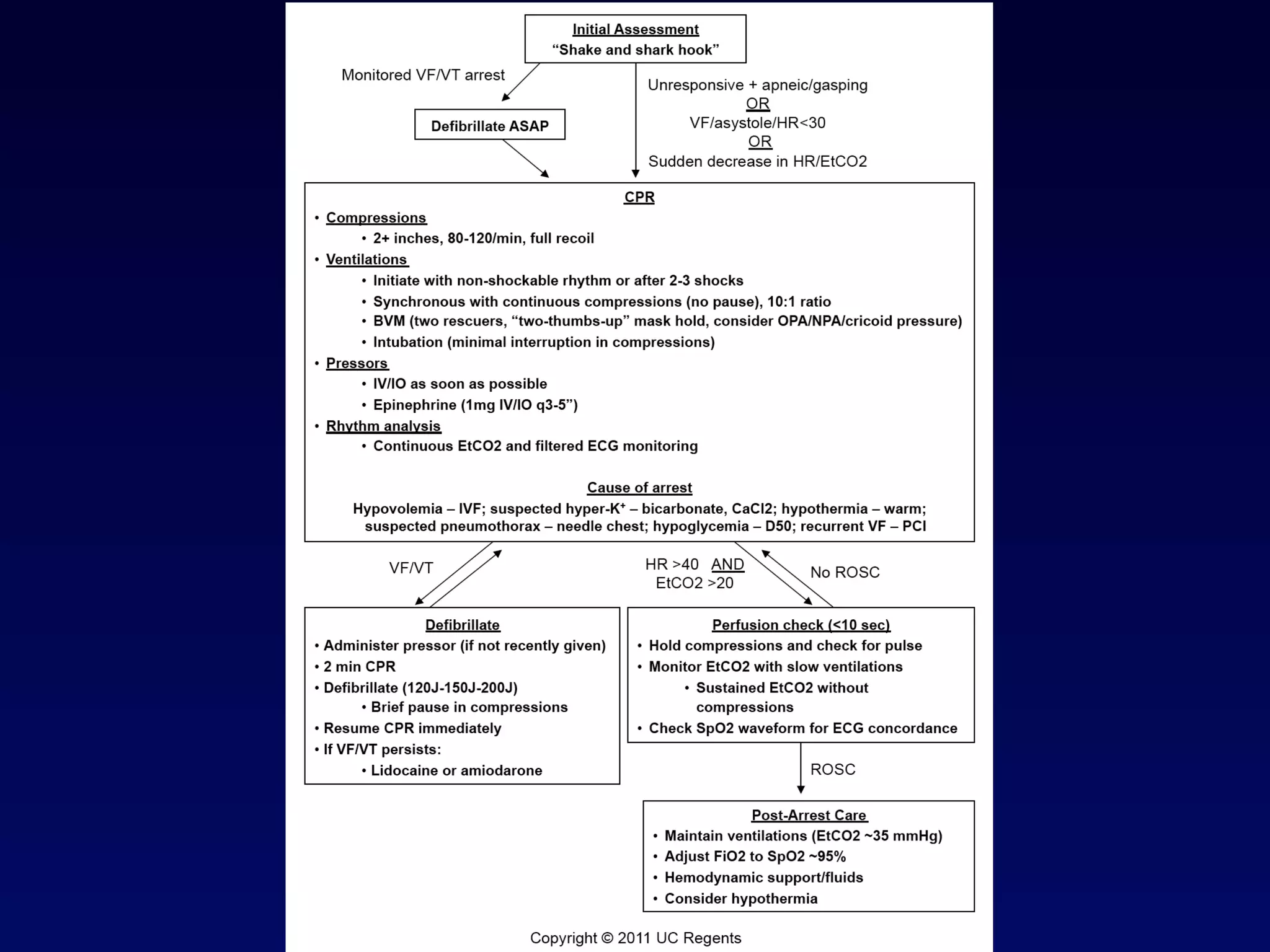
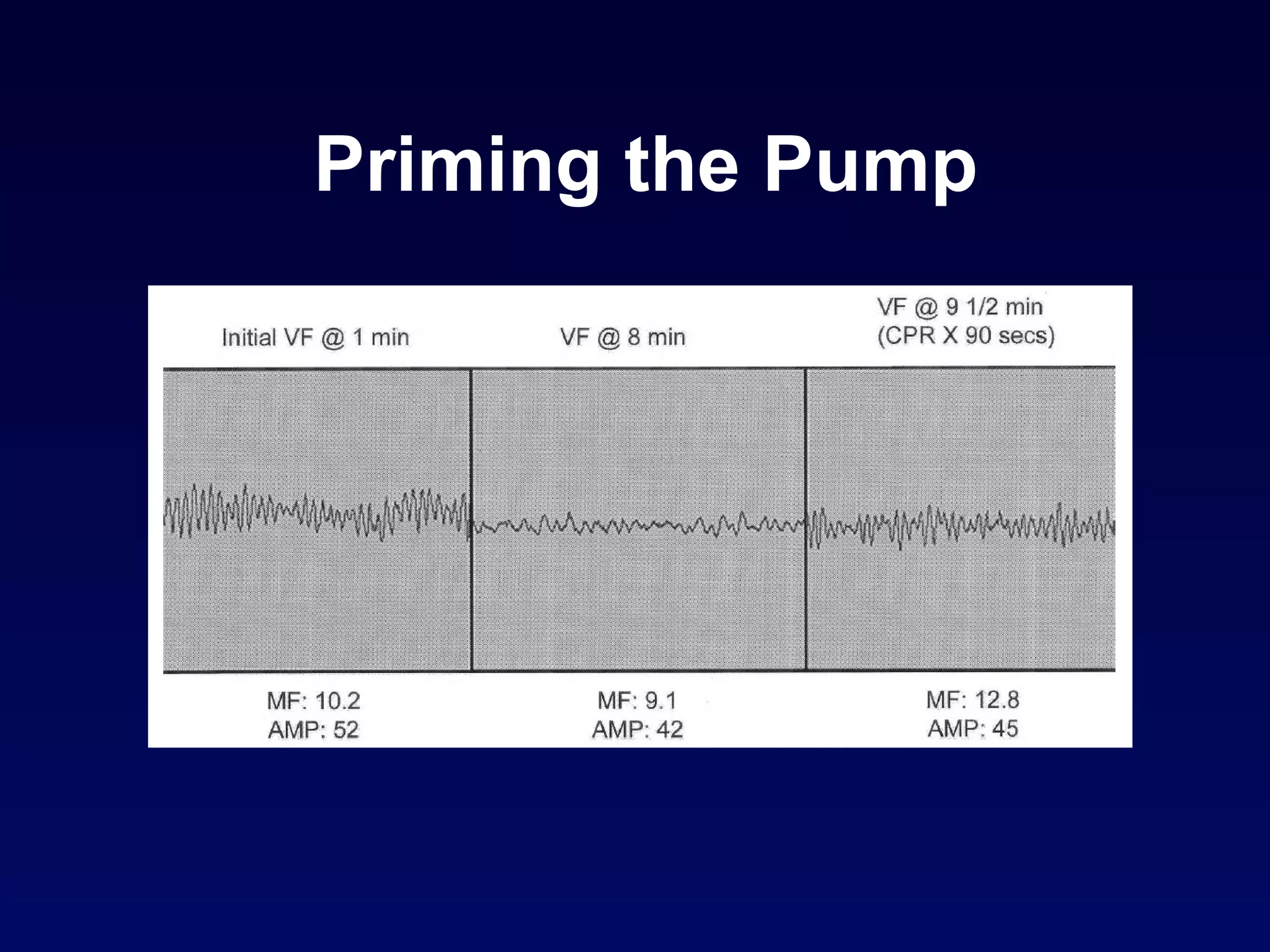
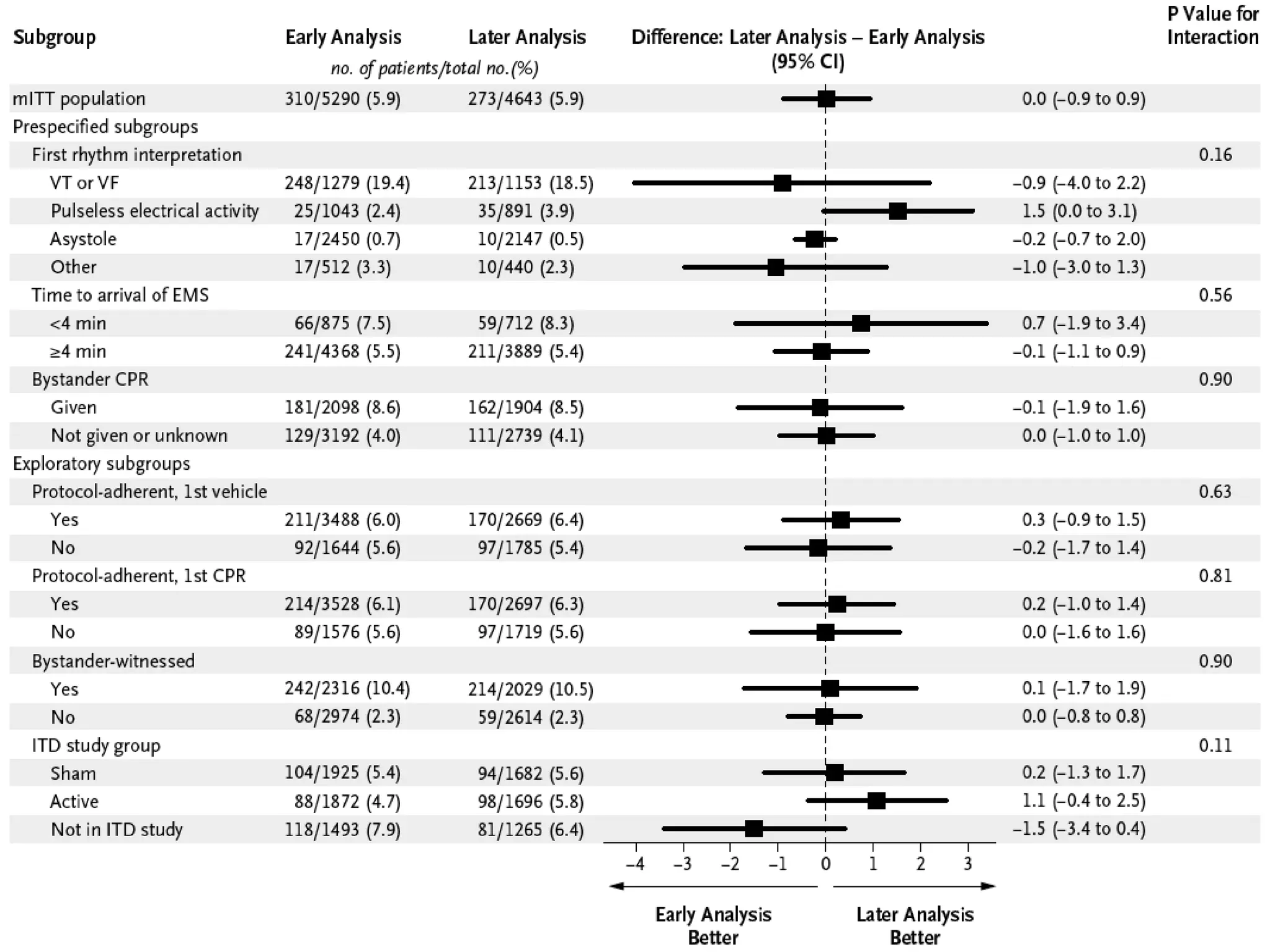
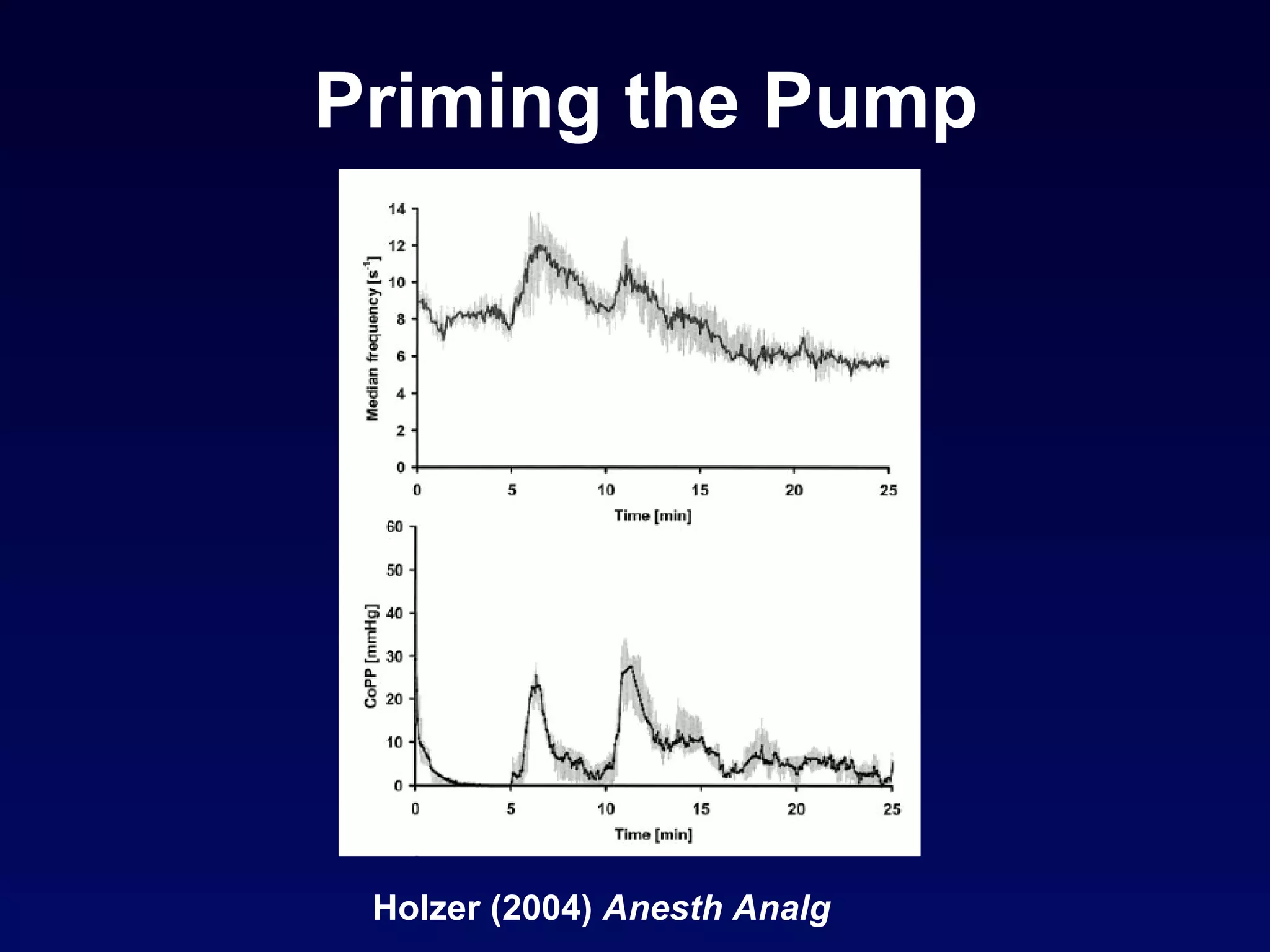
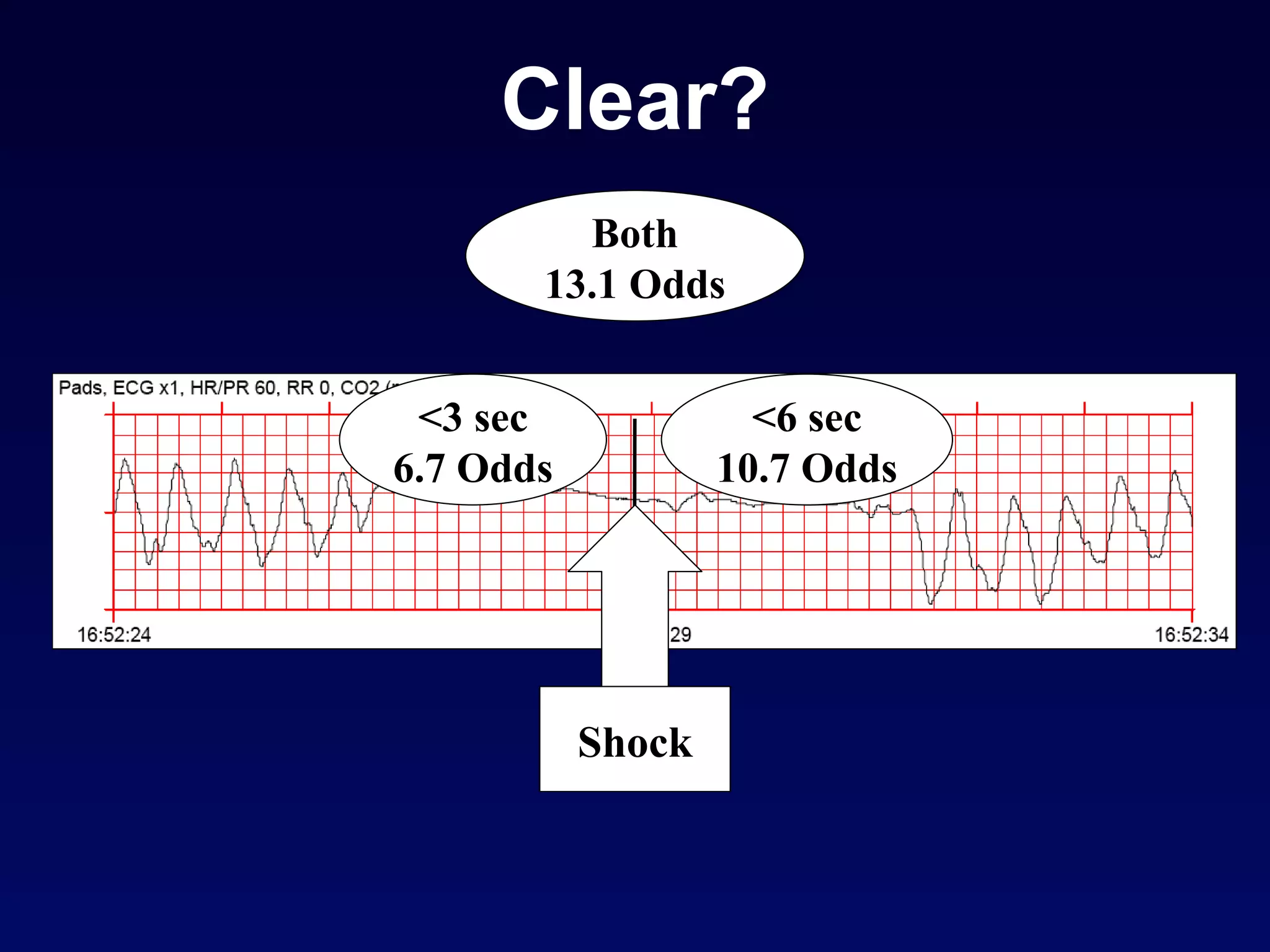
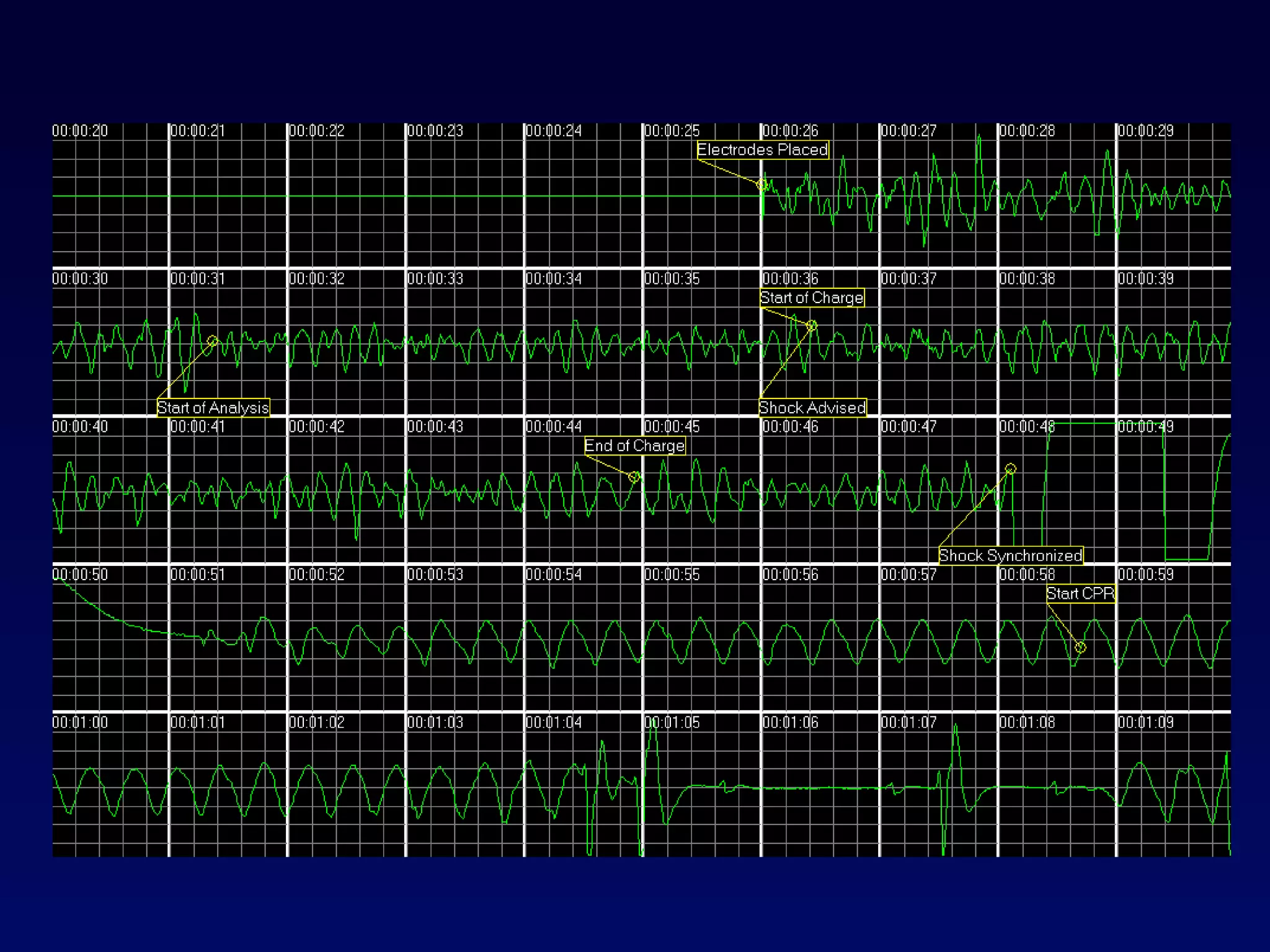
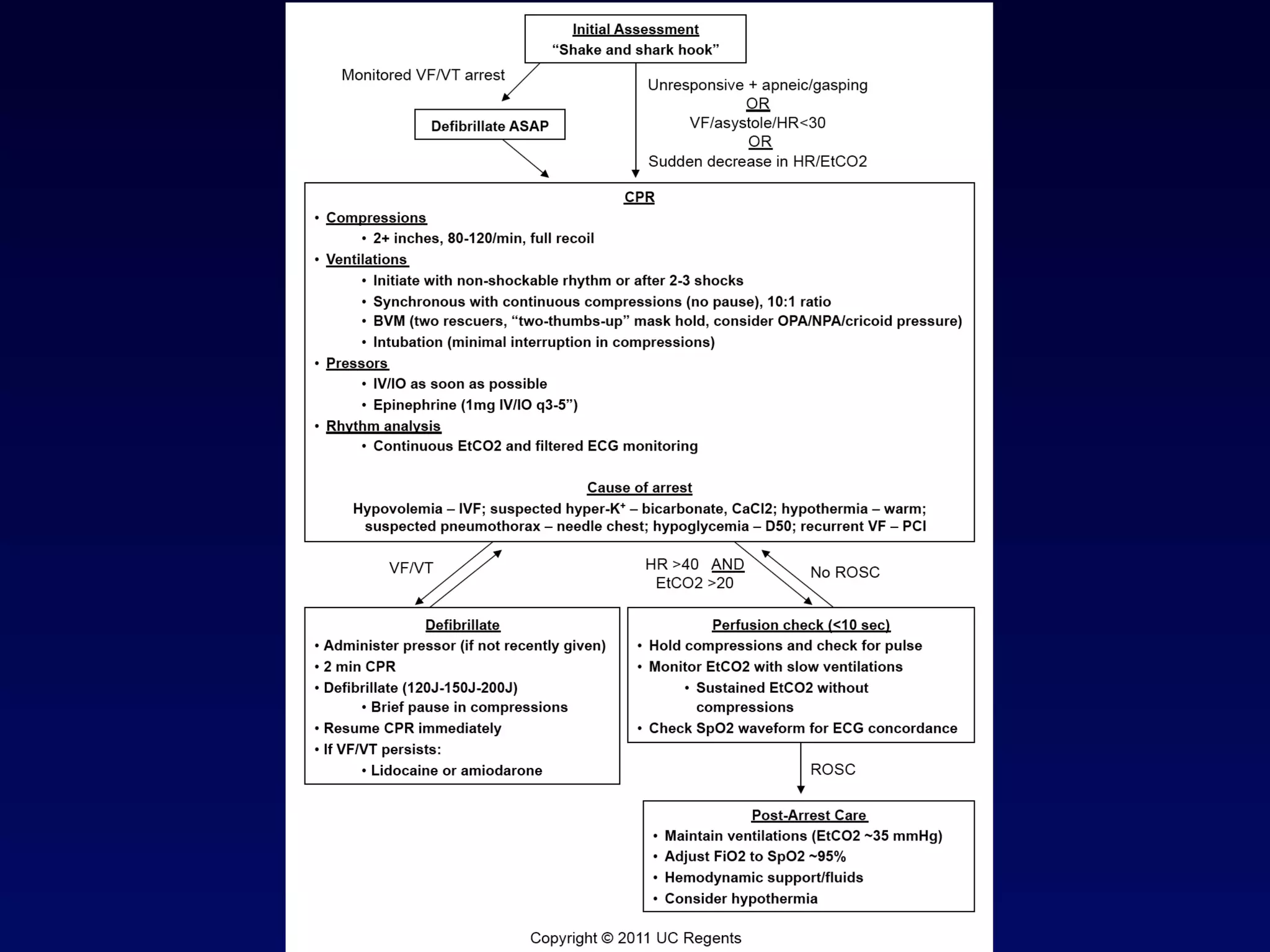
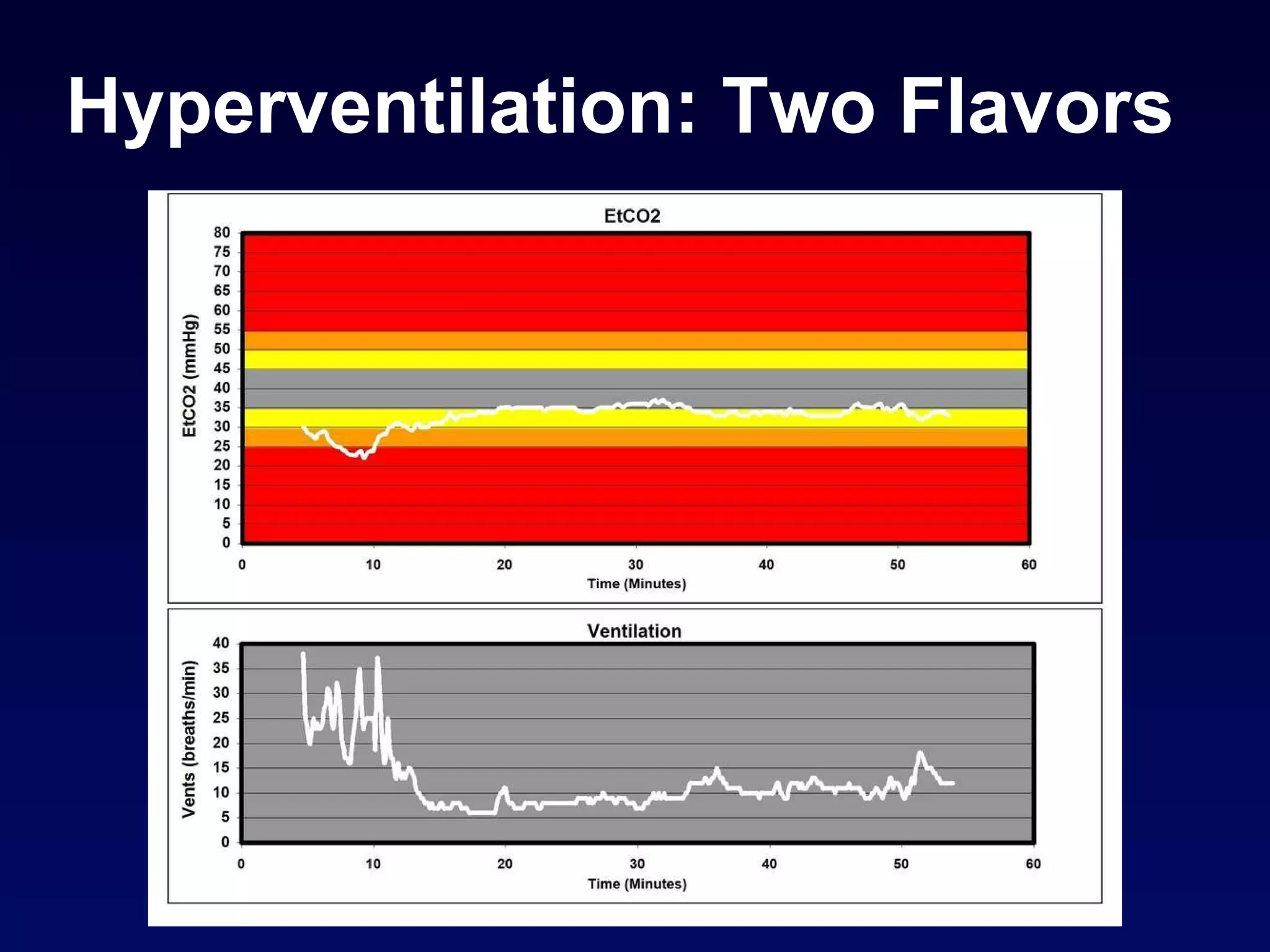
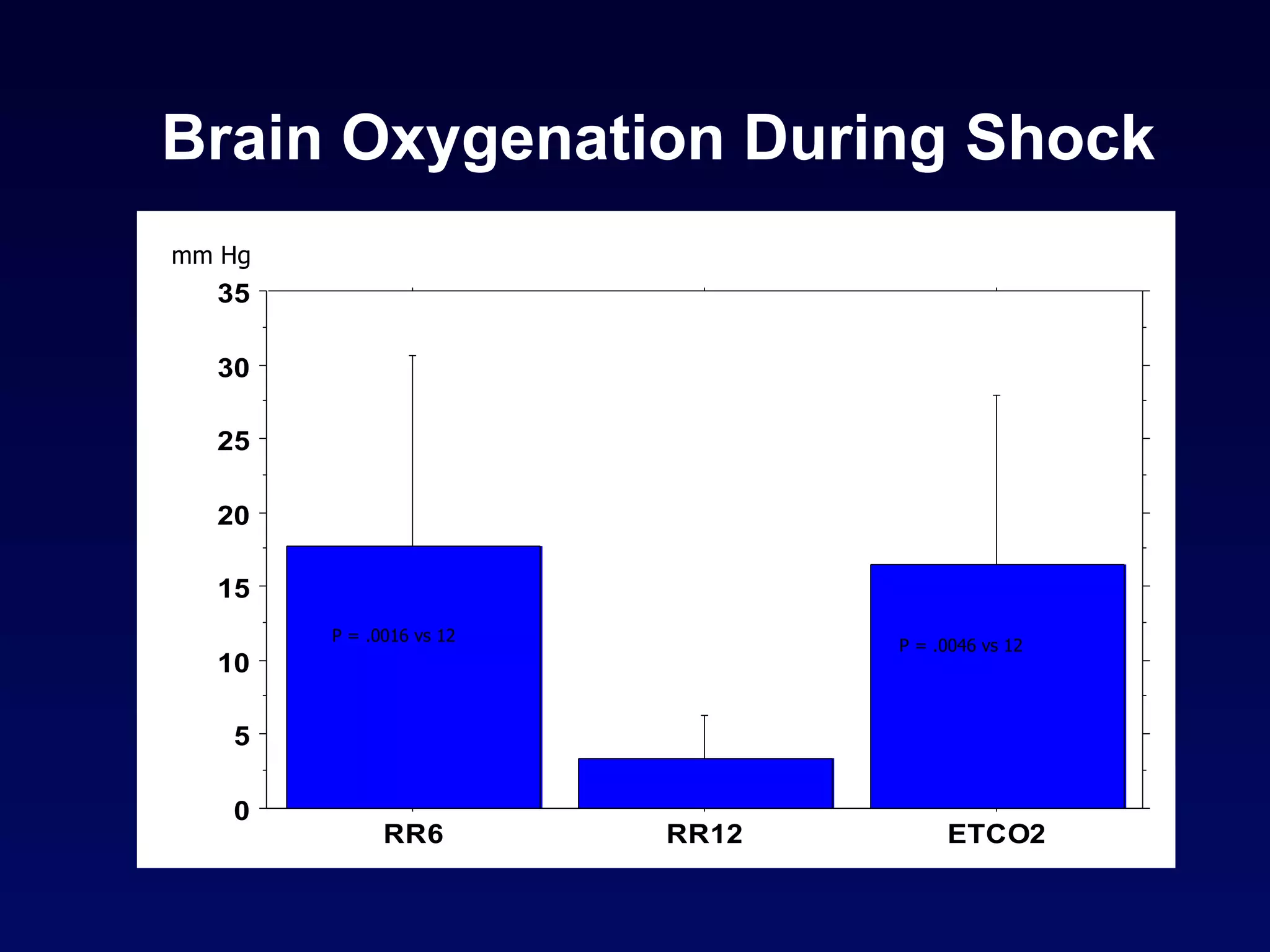
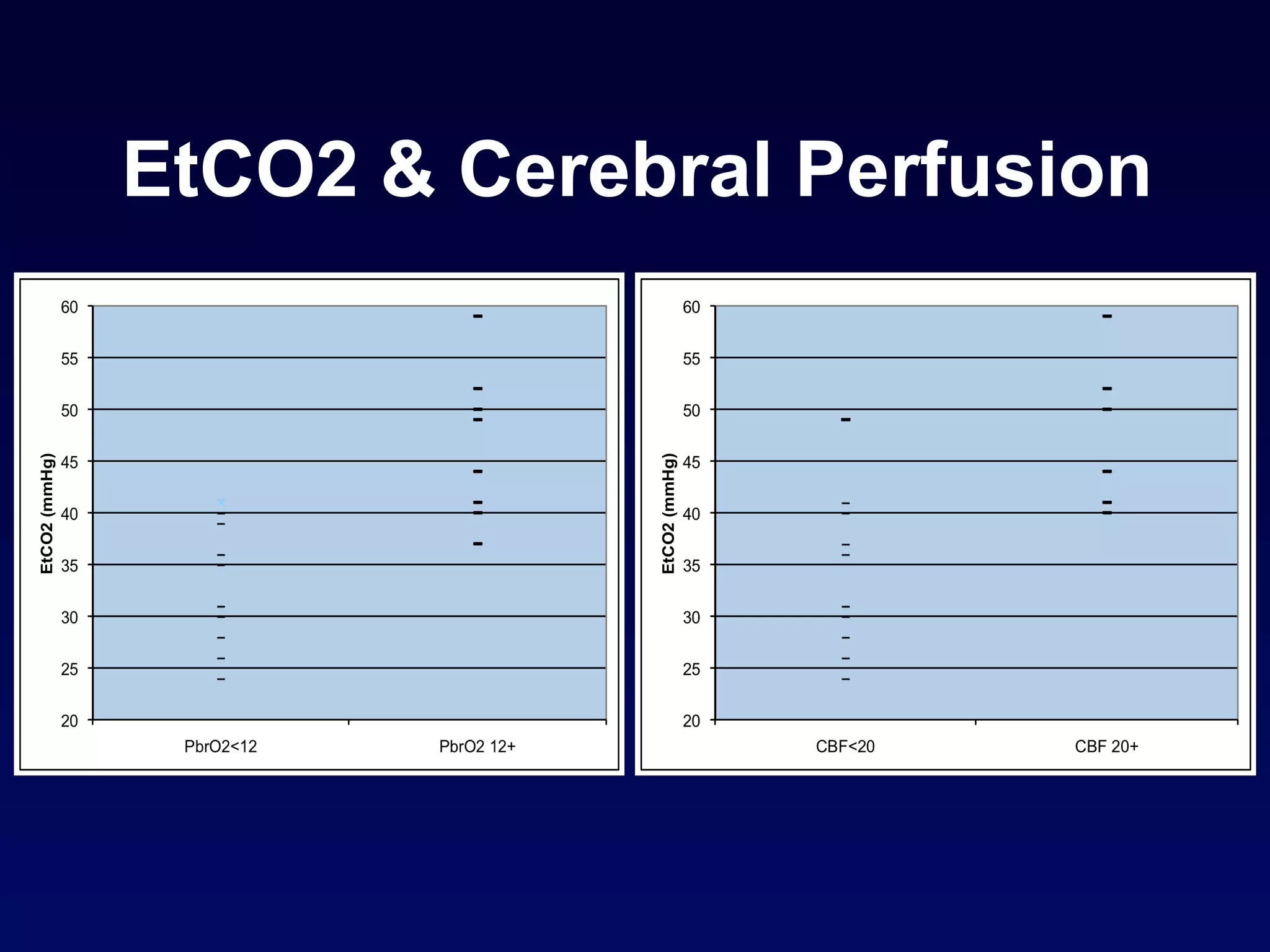
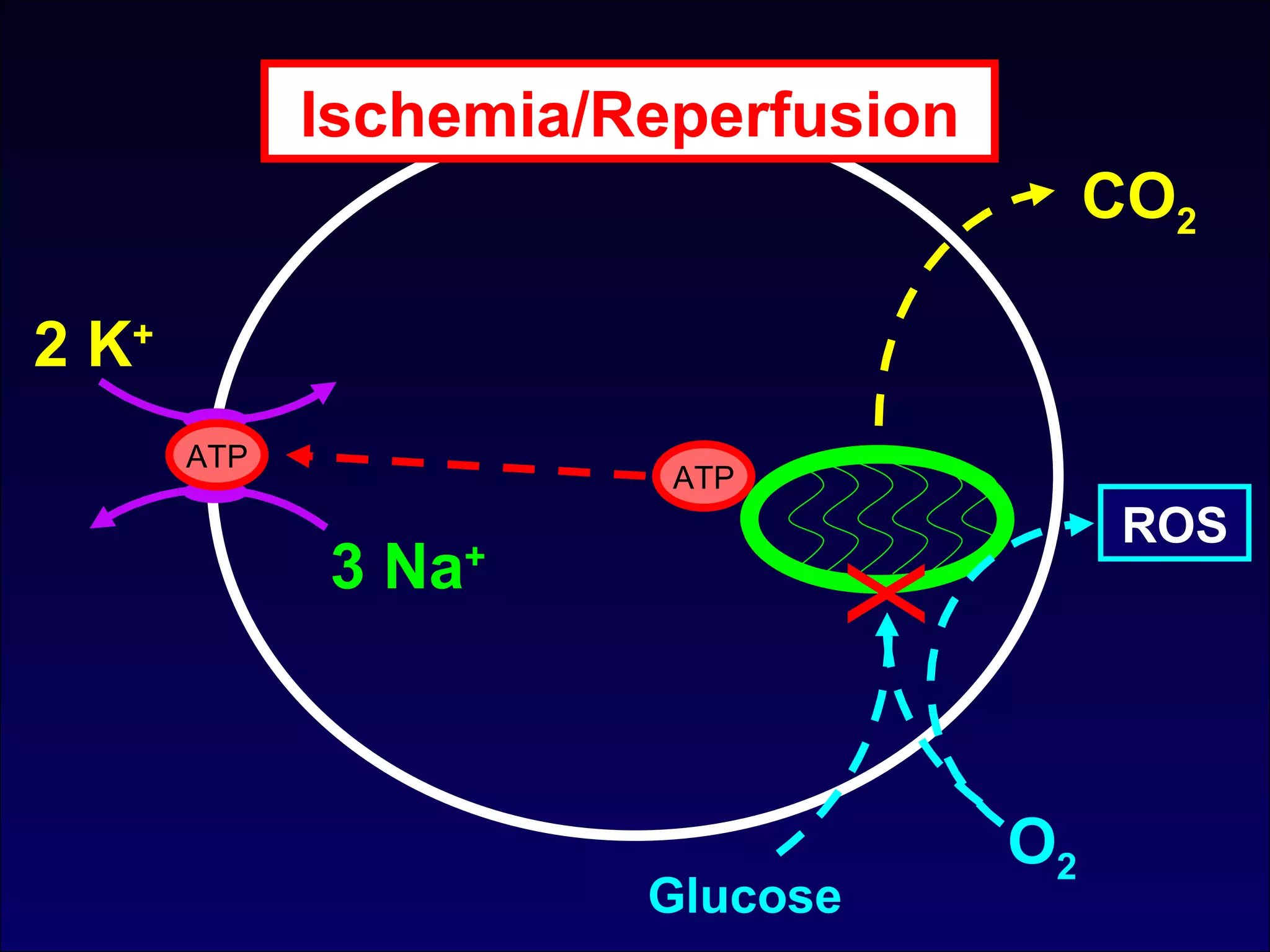
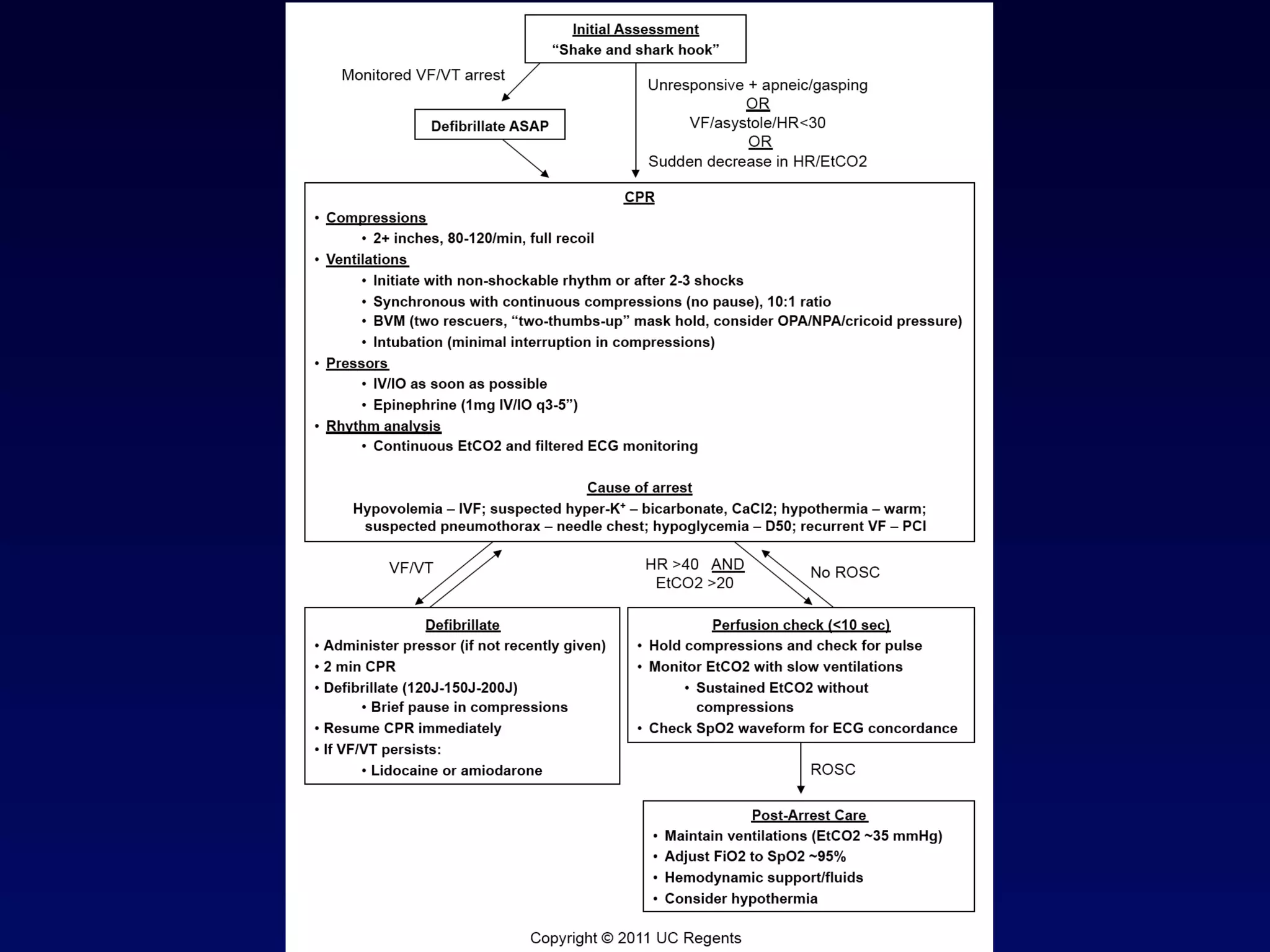
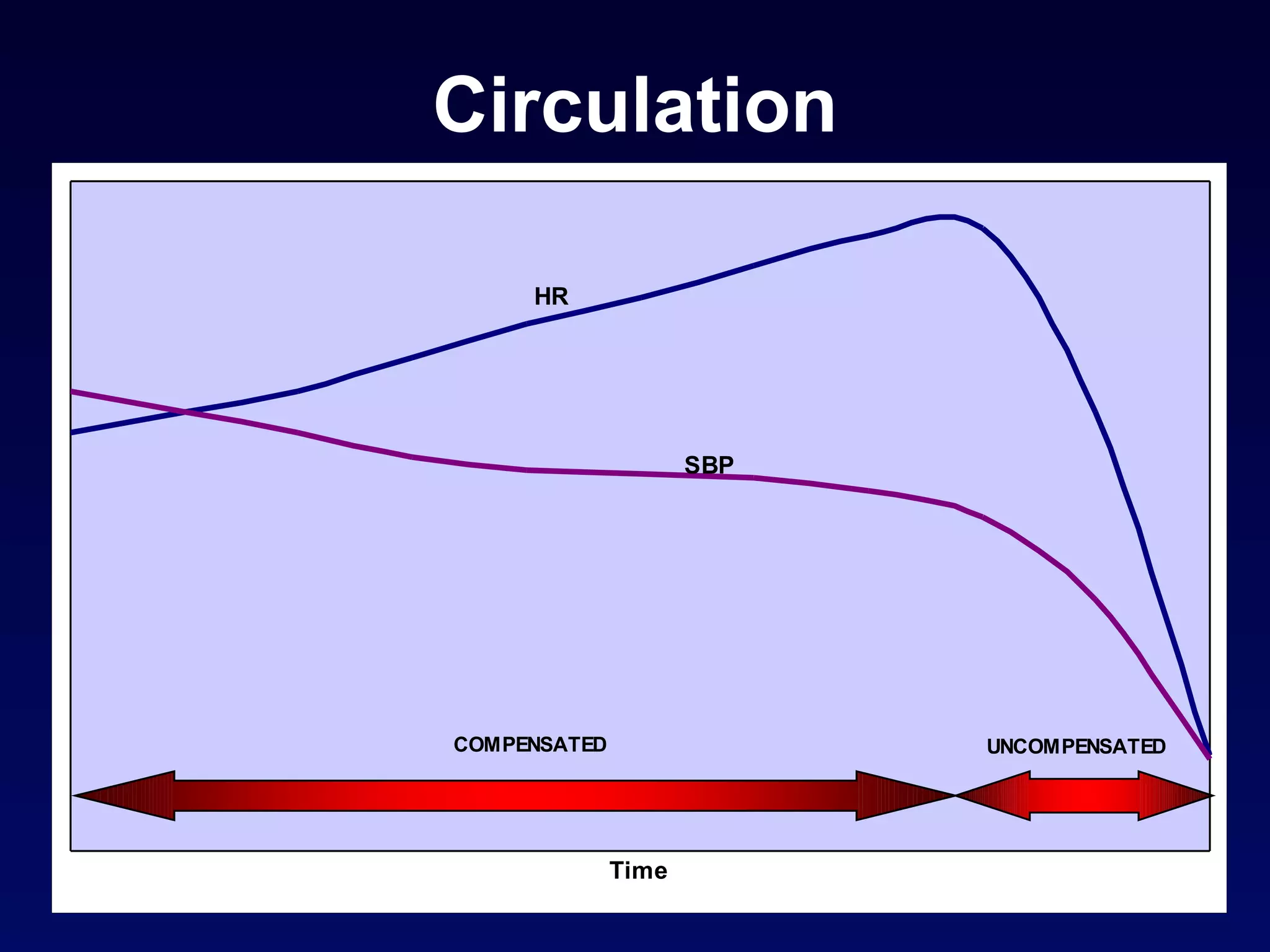
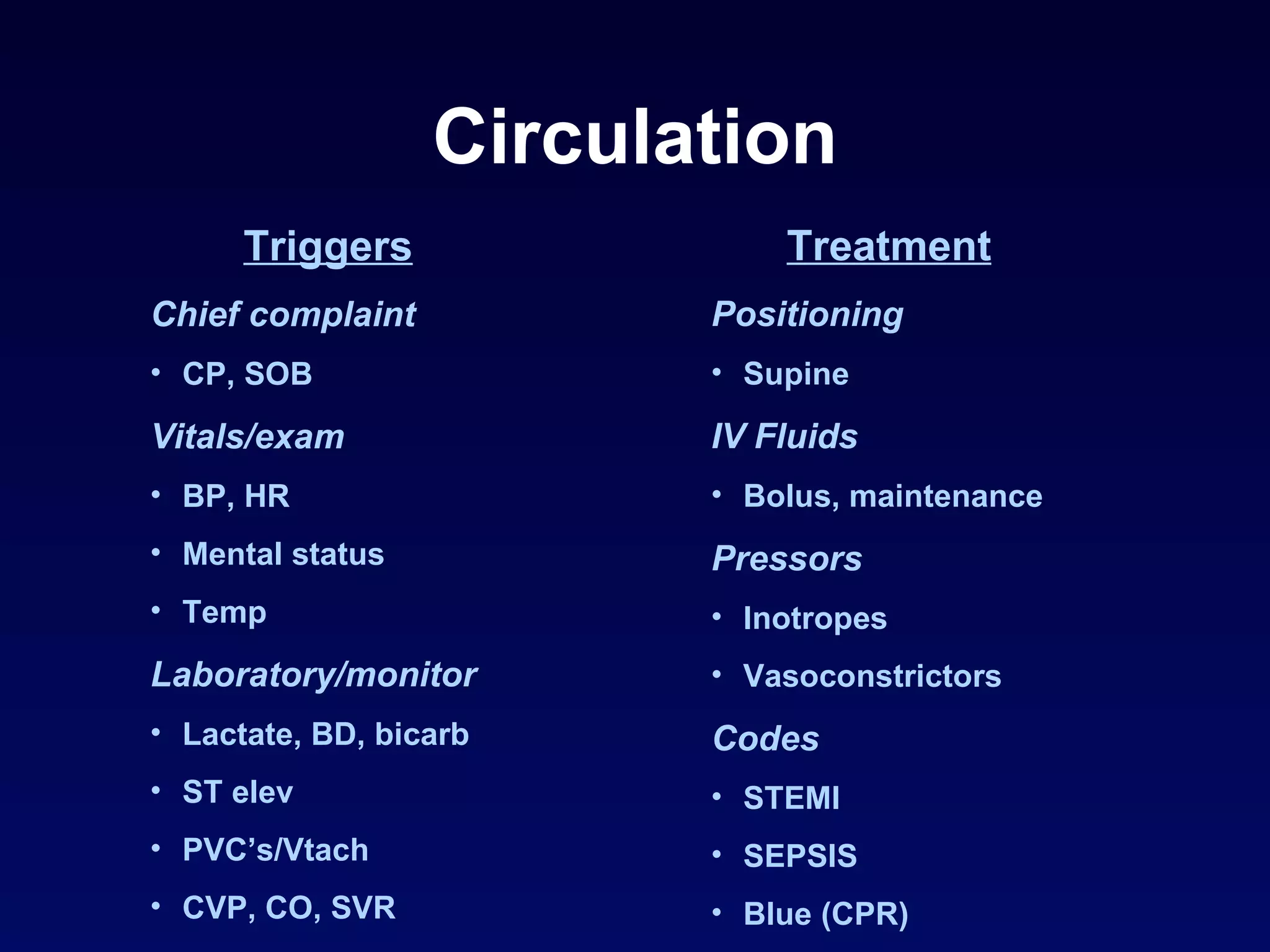
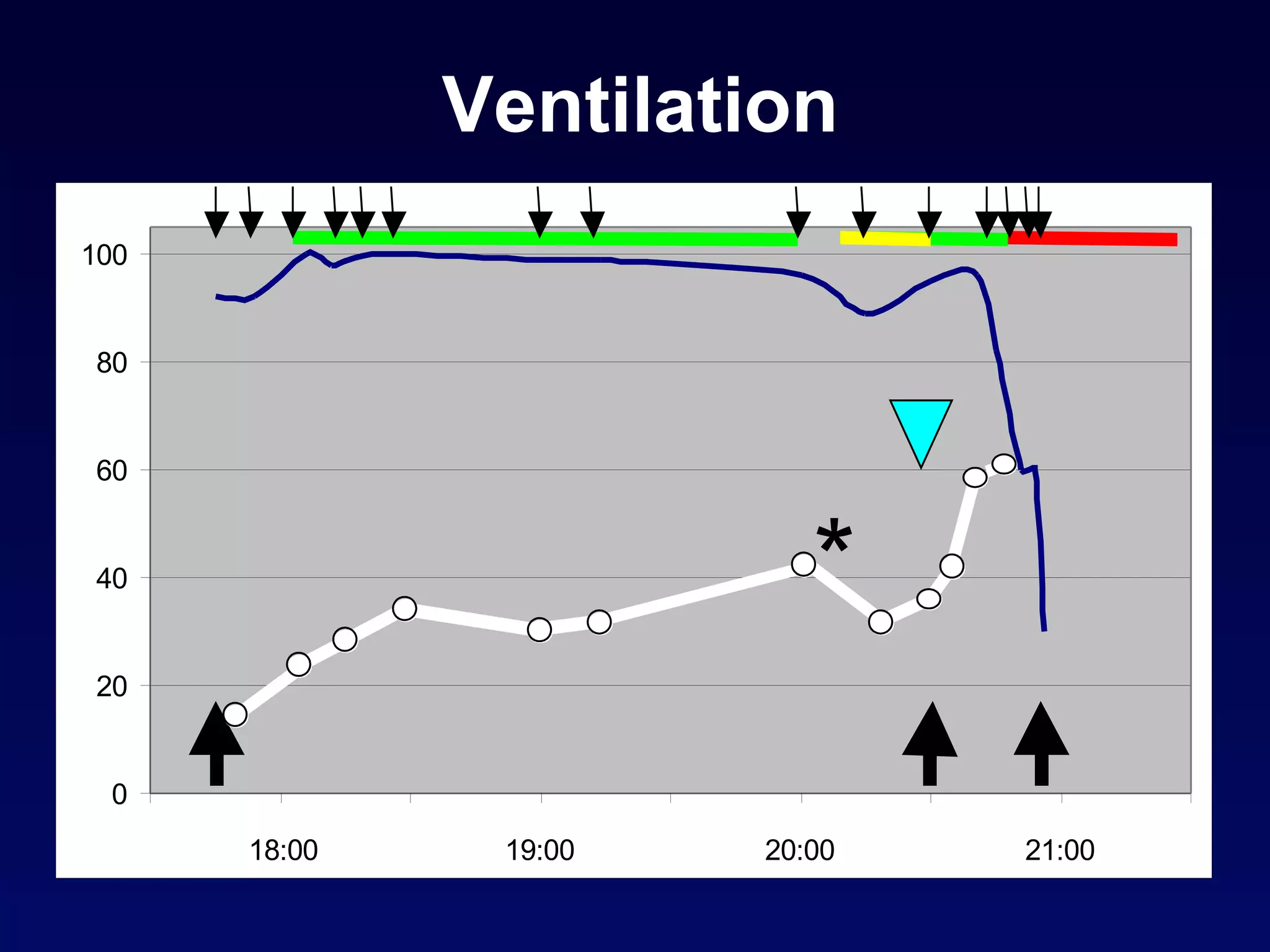
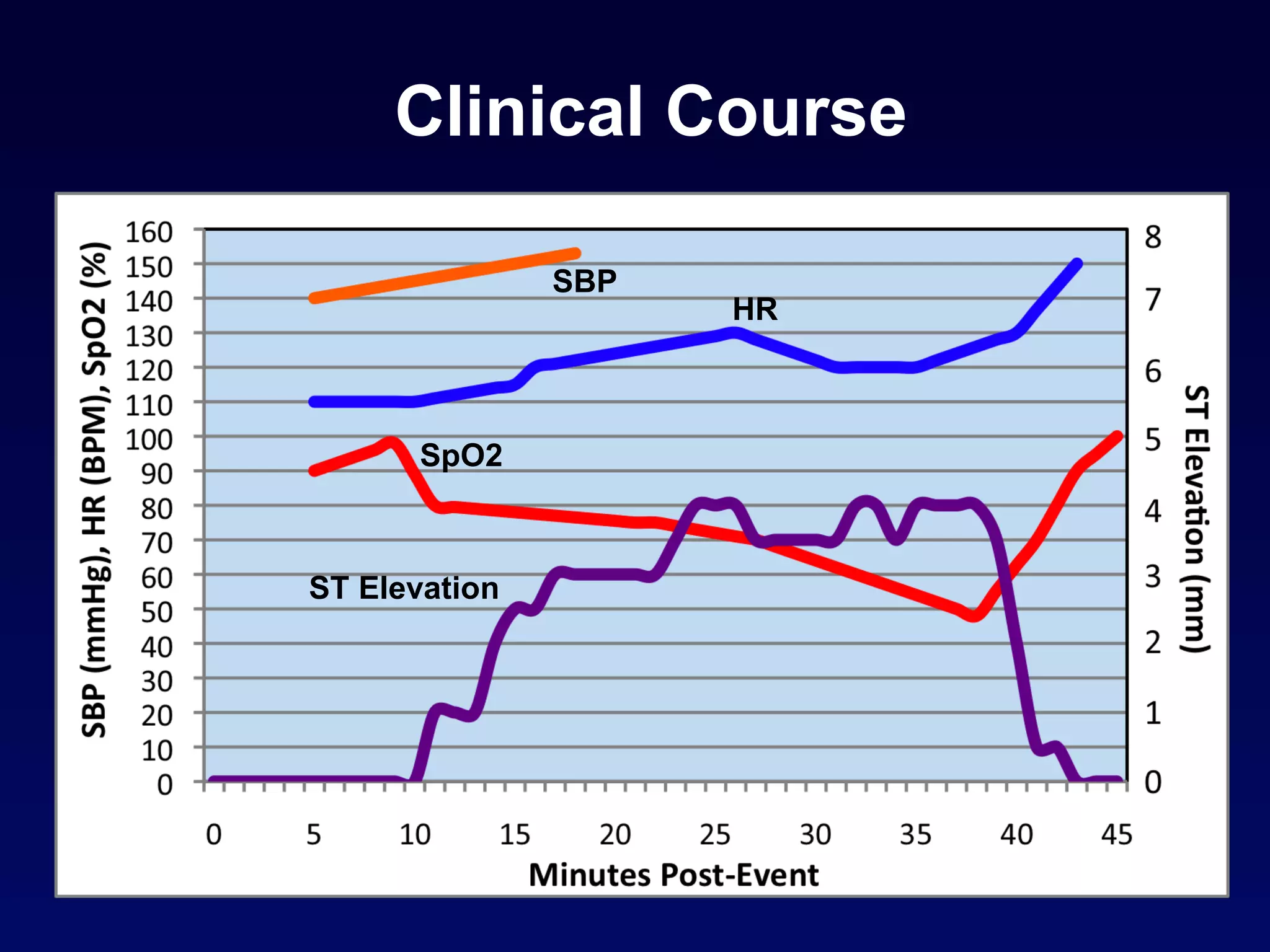
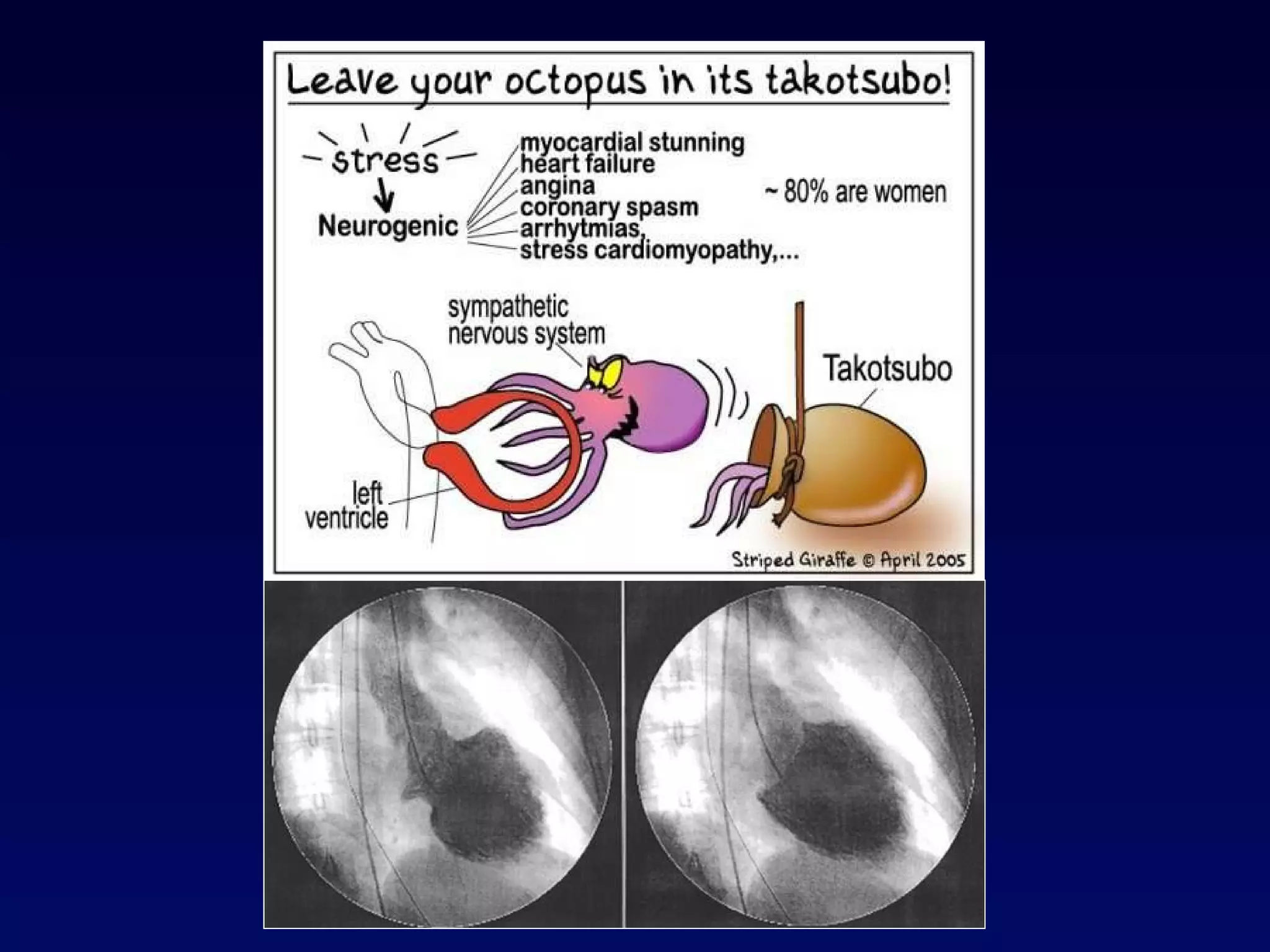
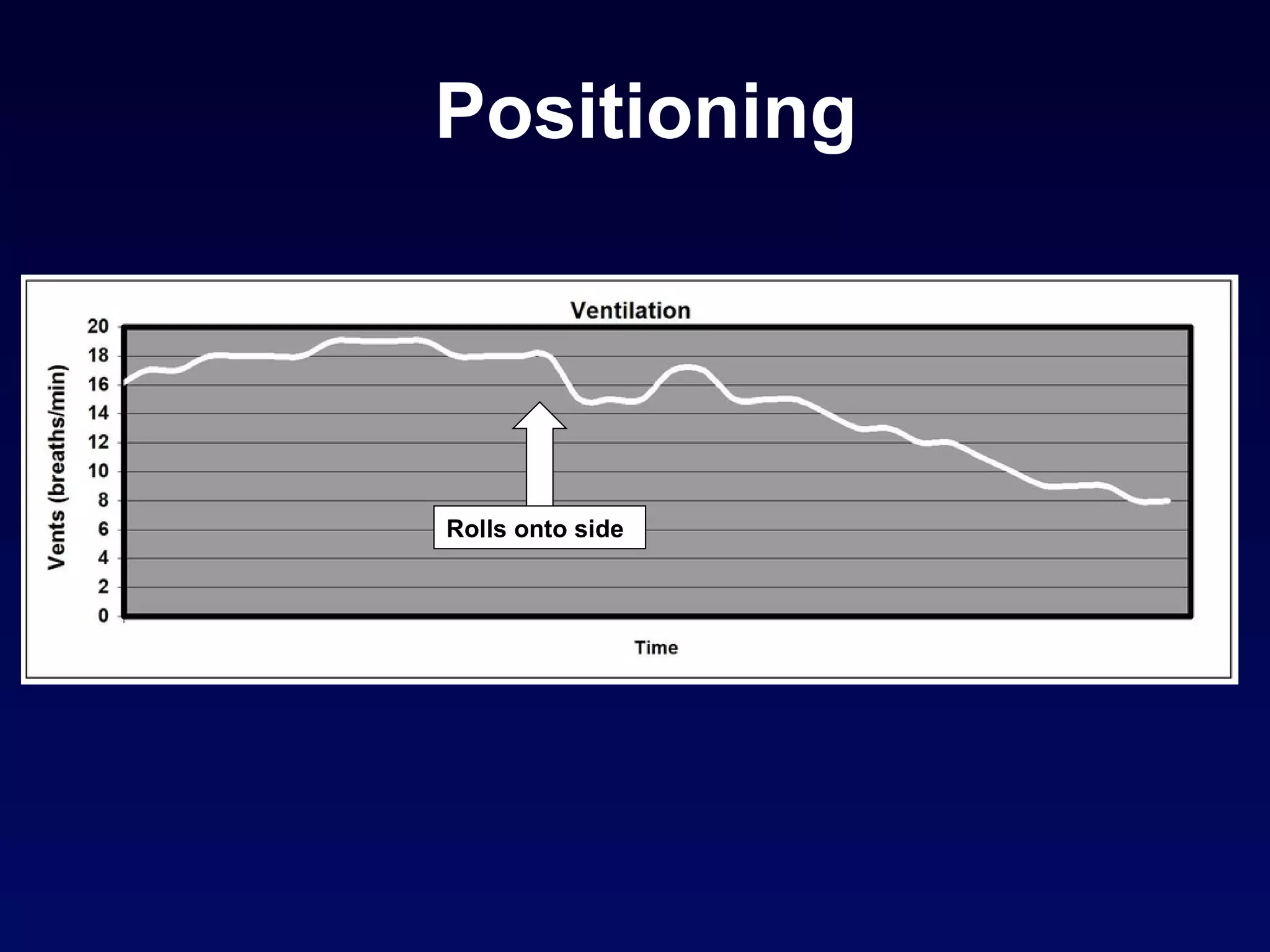
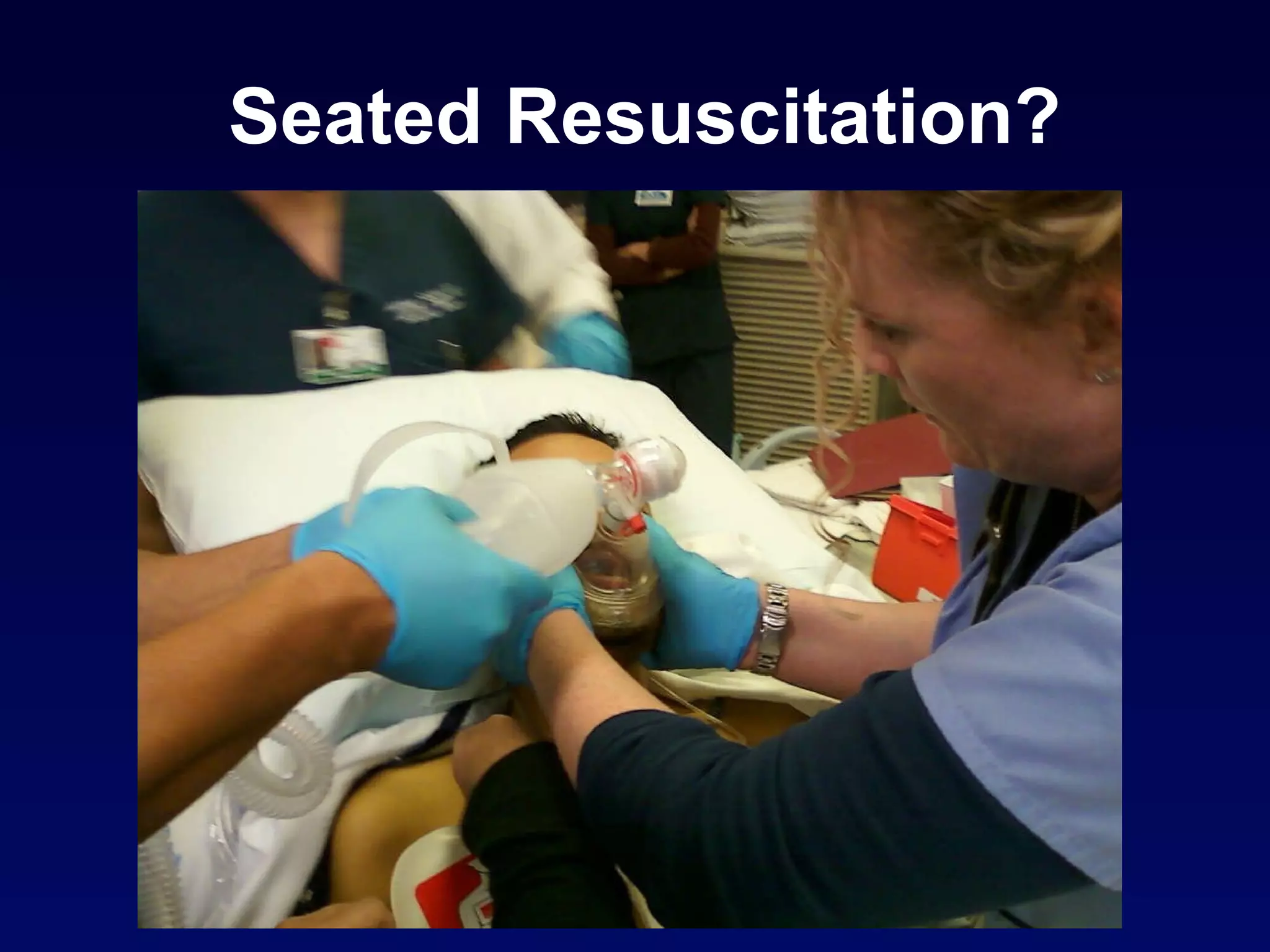
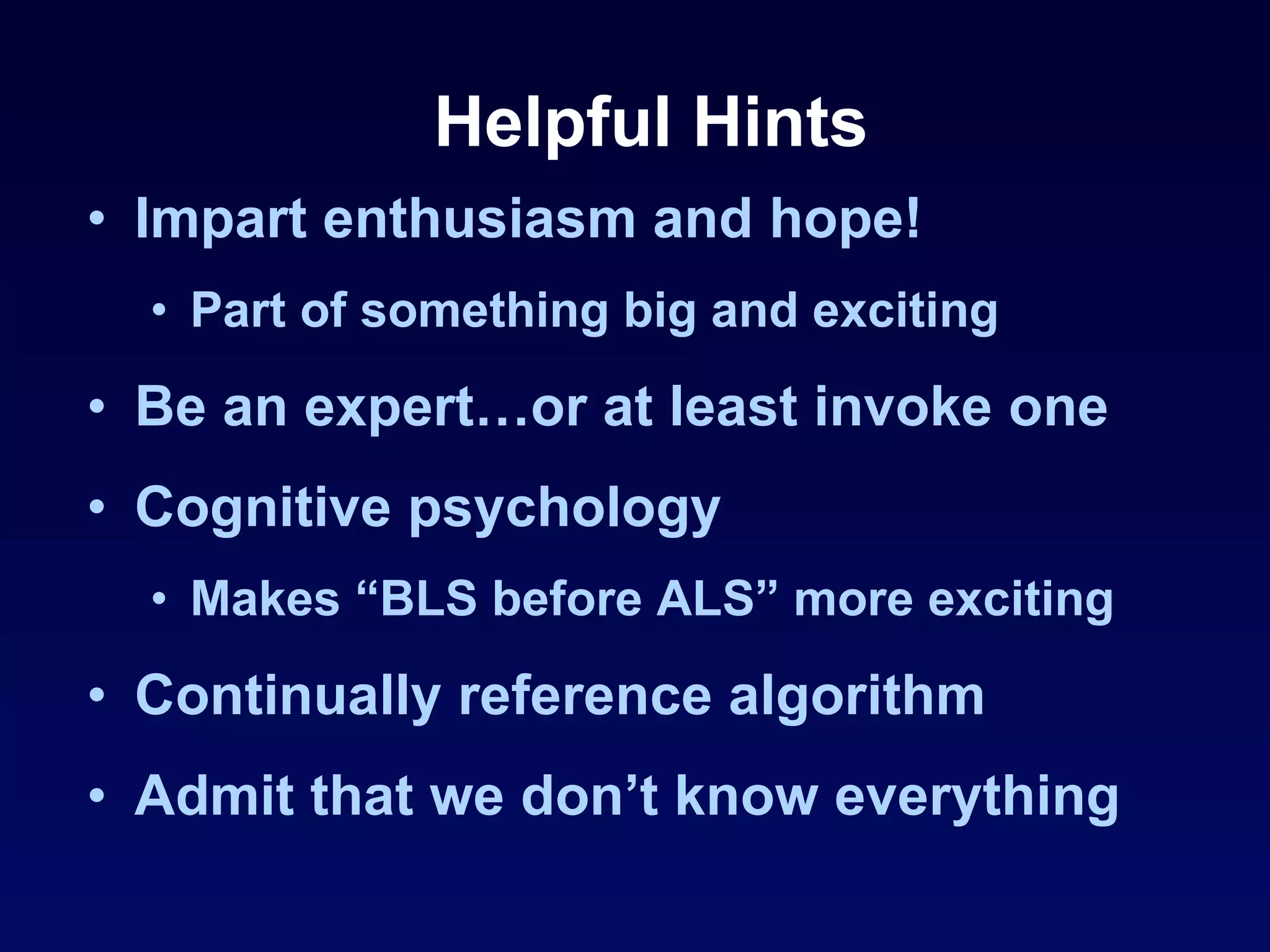
The document outlines the Advanced Resuscitation Techniques (ART) model for improving resuscitation outcomes. It describes seven commandments of cardiac arrest care, including high-quality chest compressions, use of pressors, ventilation techniques, and a focus on prevention. Sample patient cases and data on outcomes with the ART model in San Diego show increased survival rates from cardiac arrest.