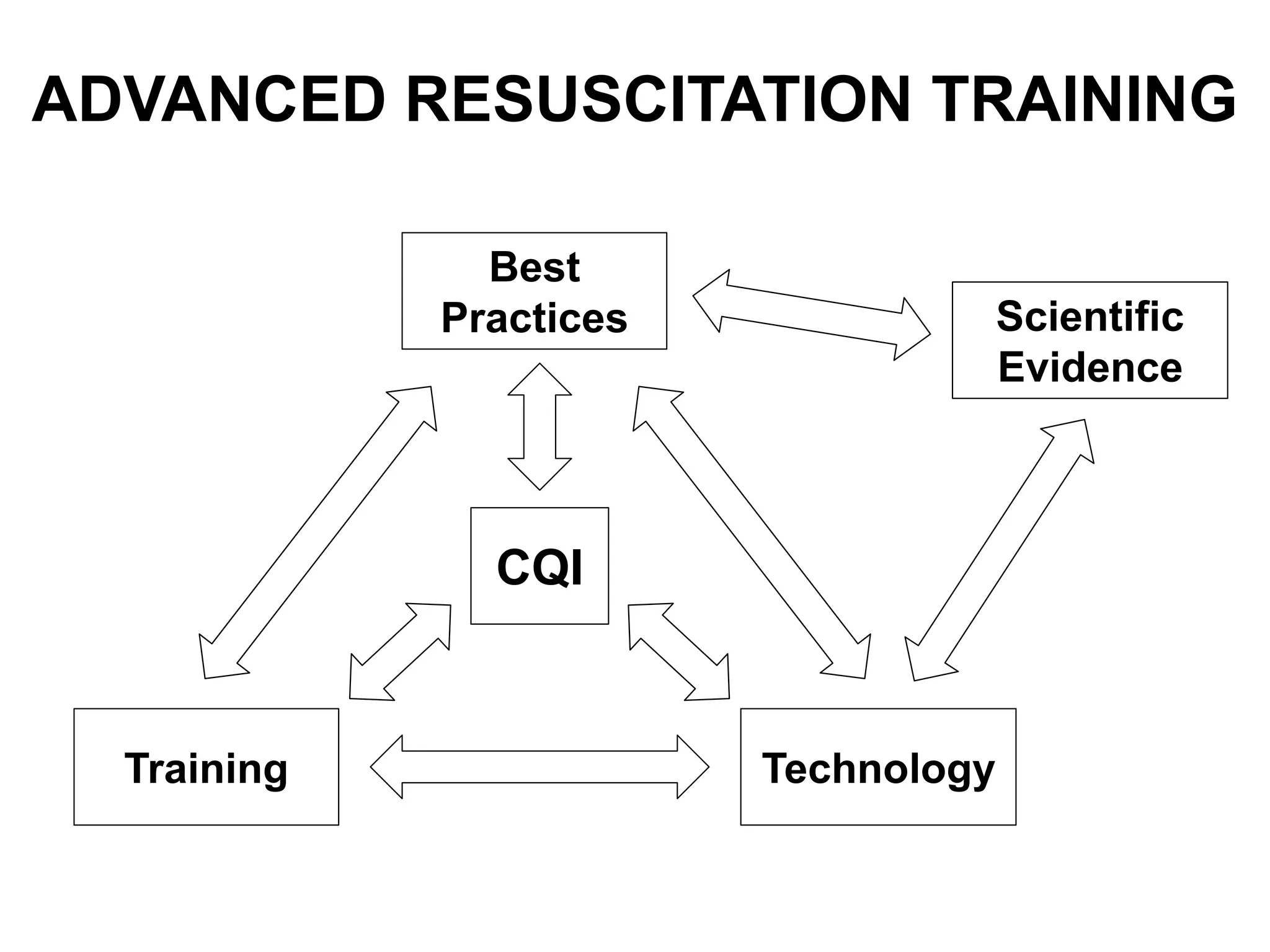
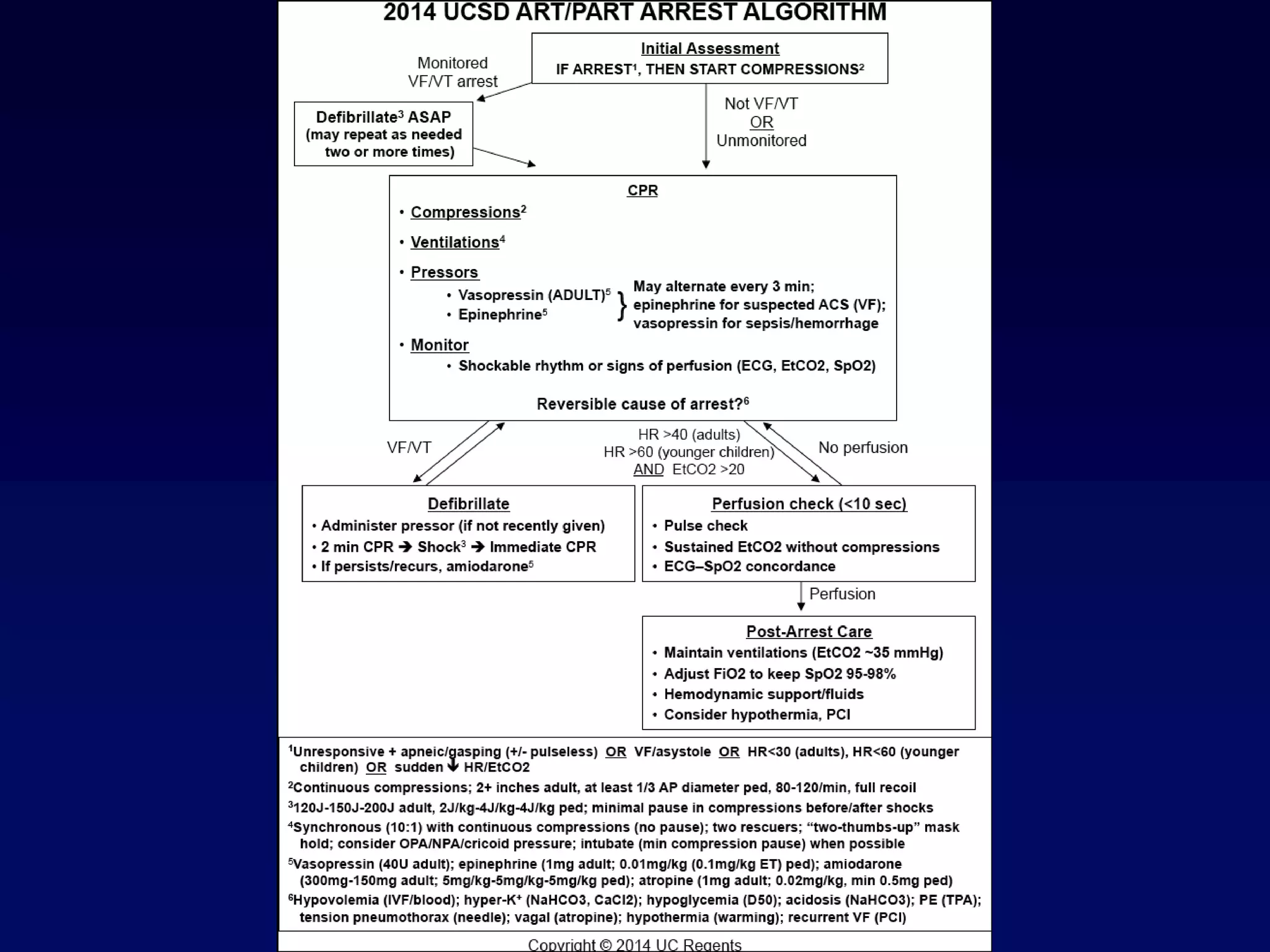
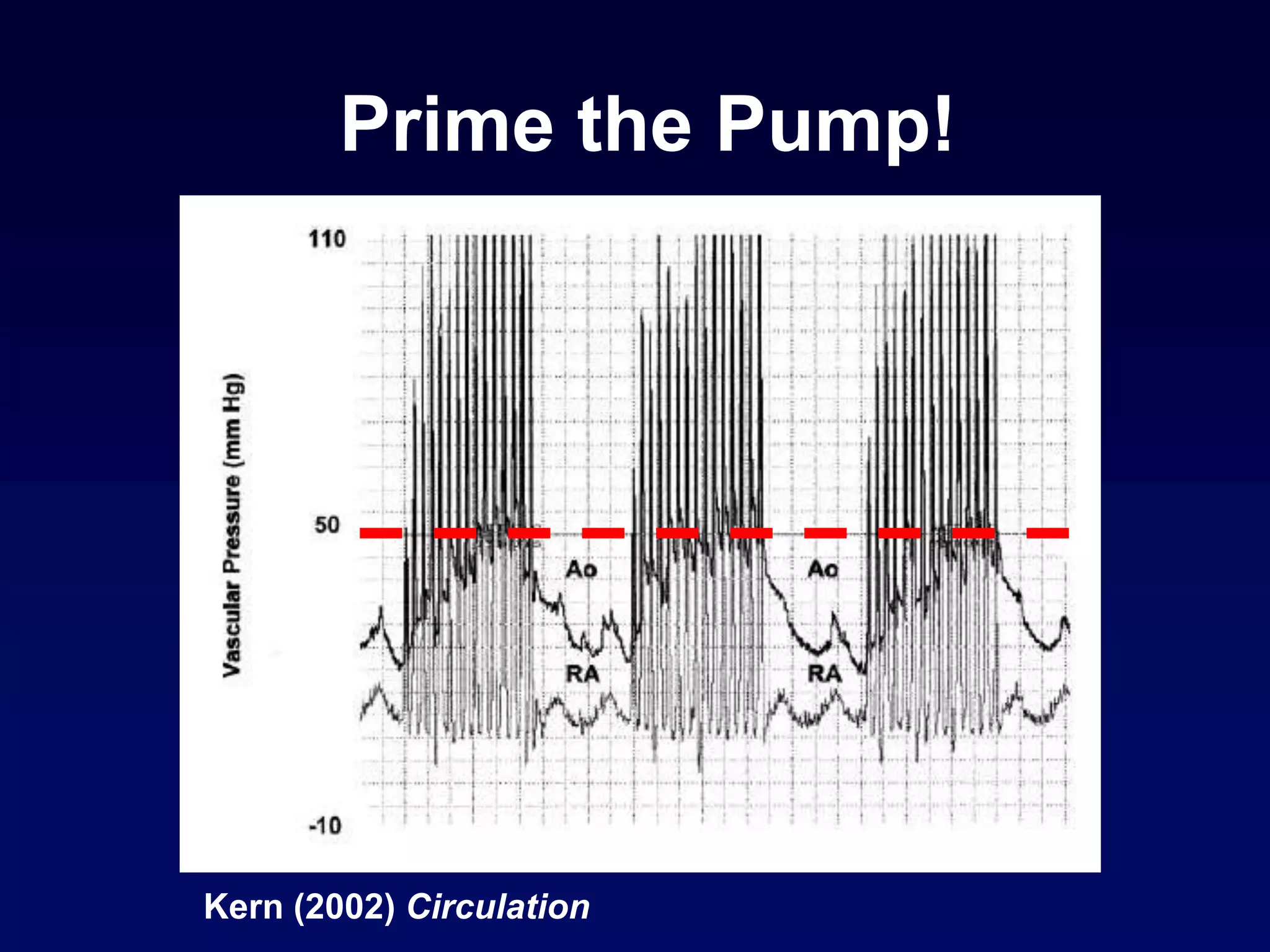
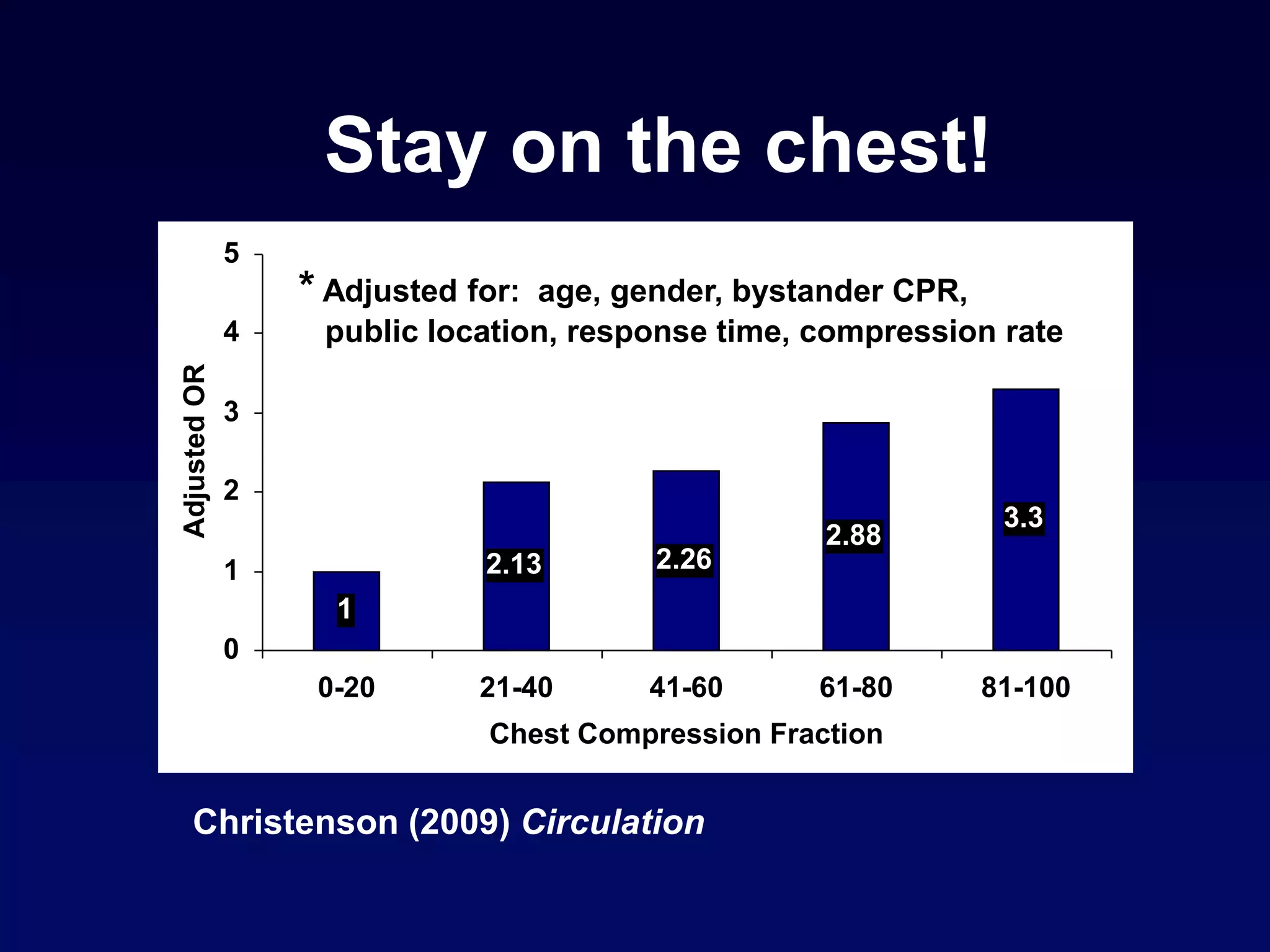
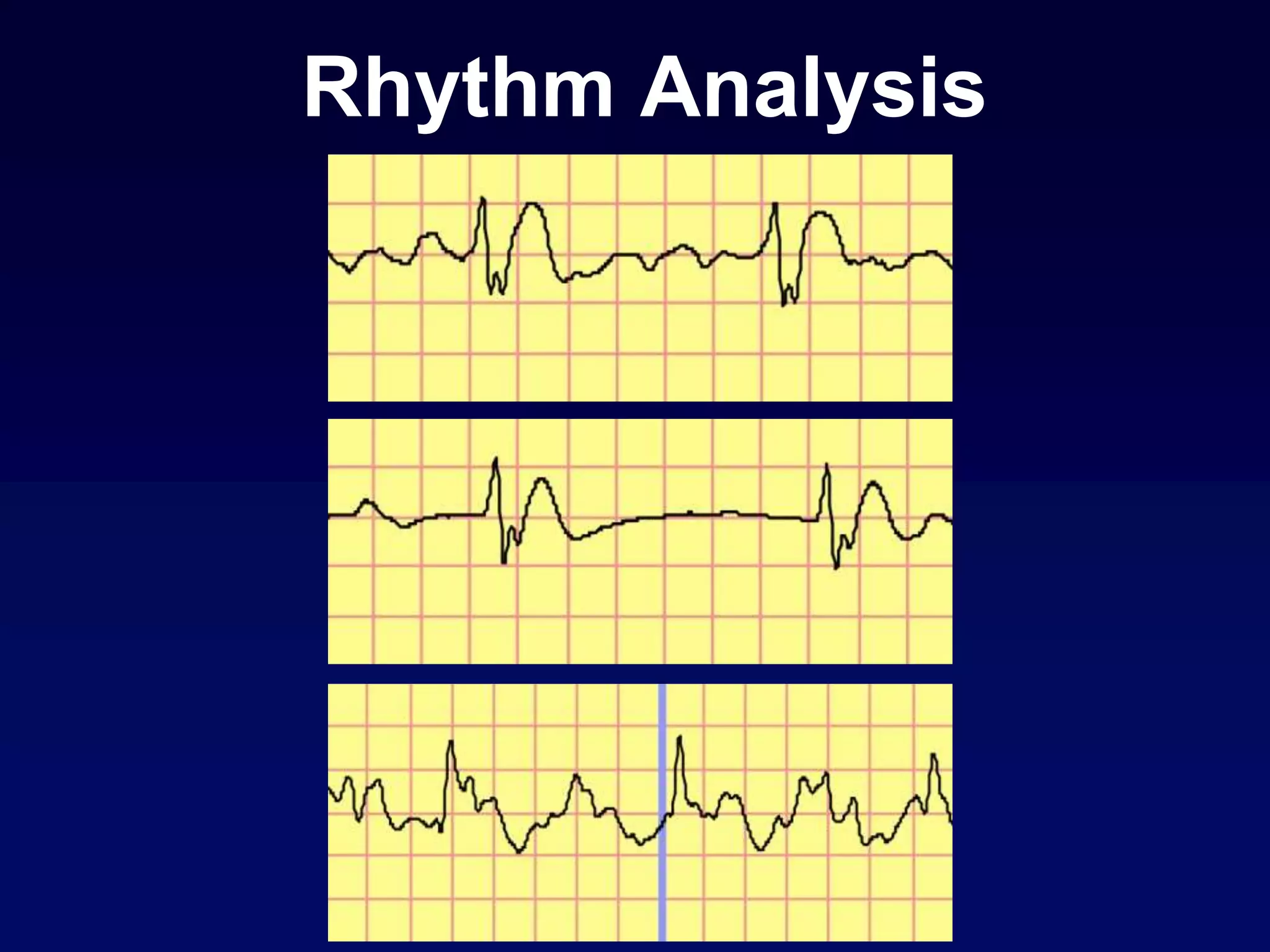
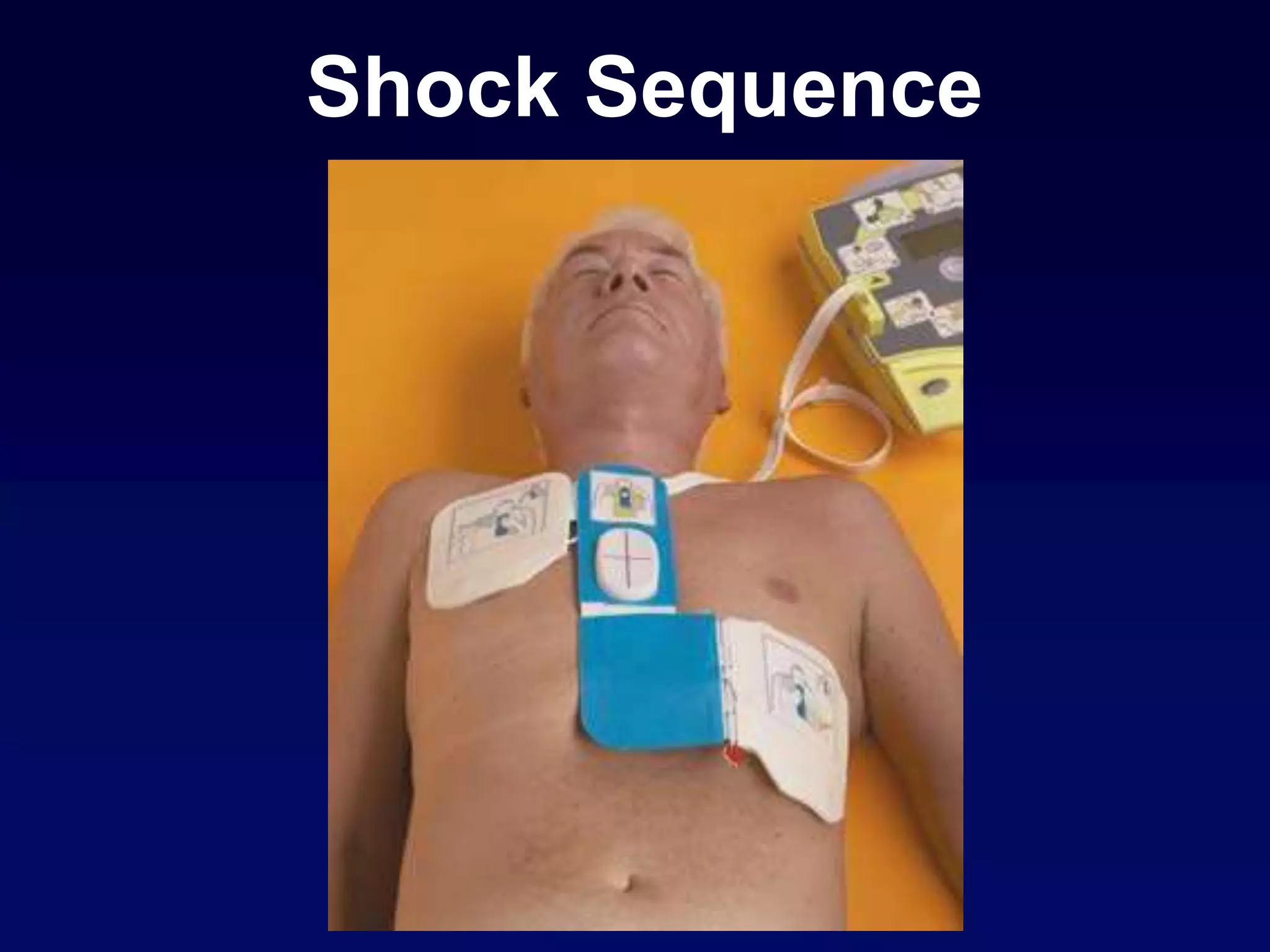
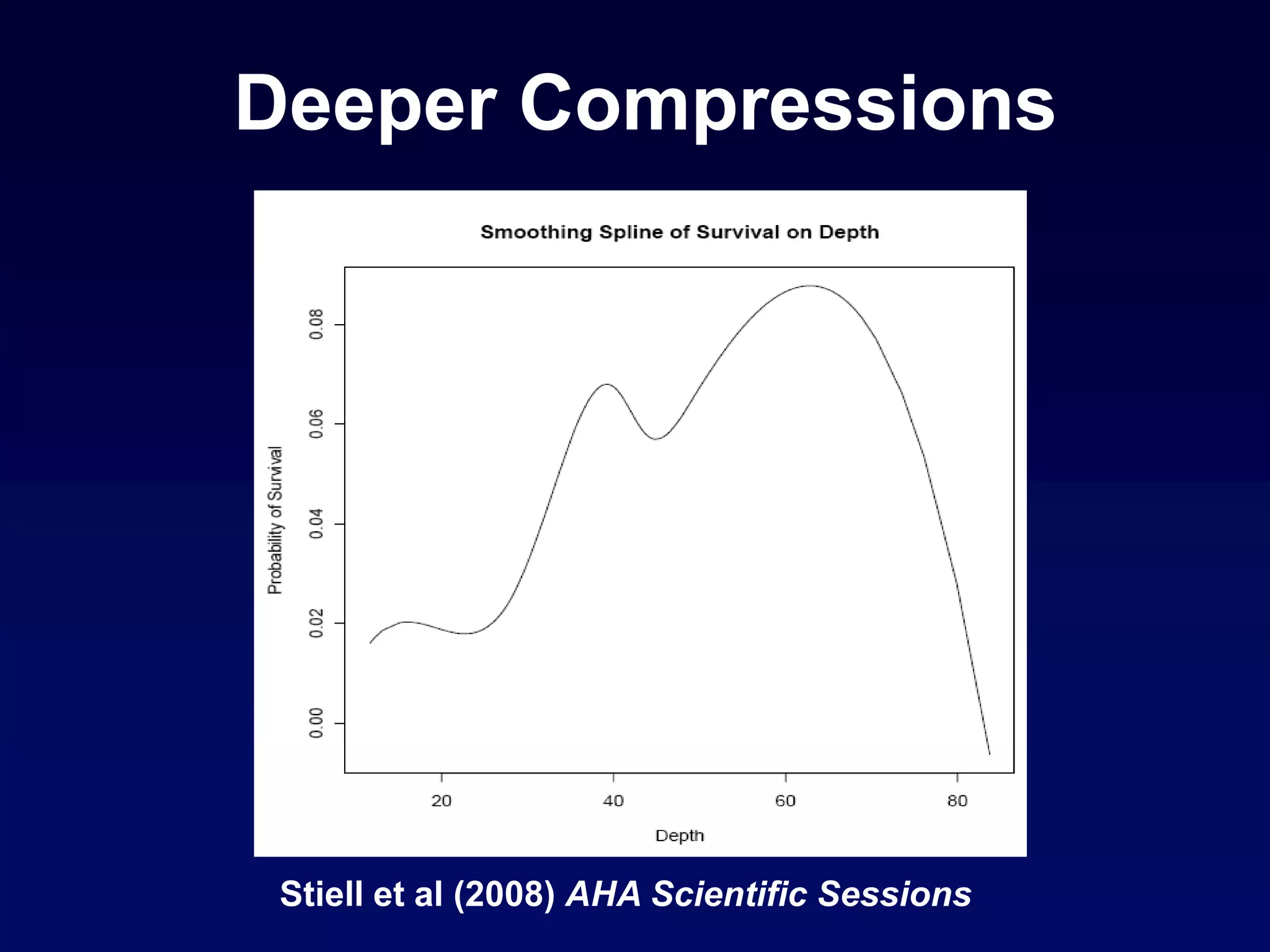
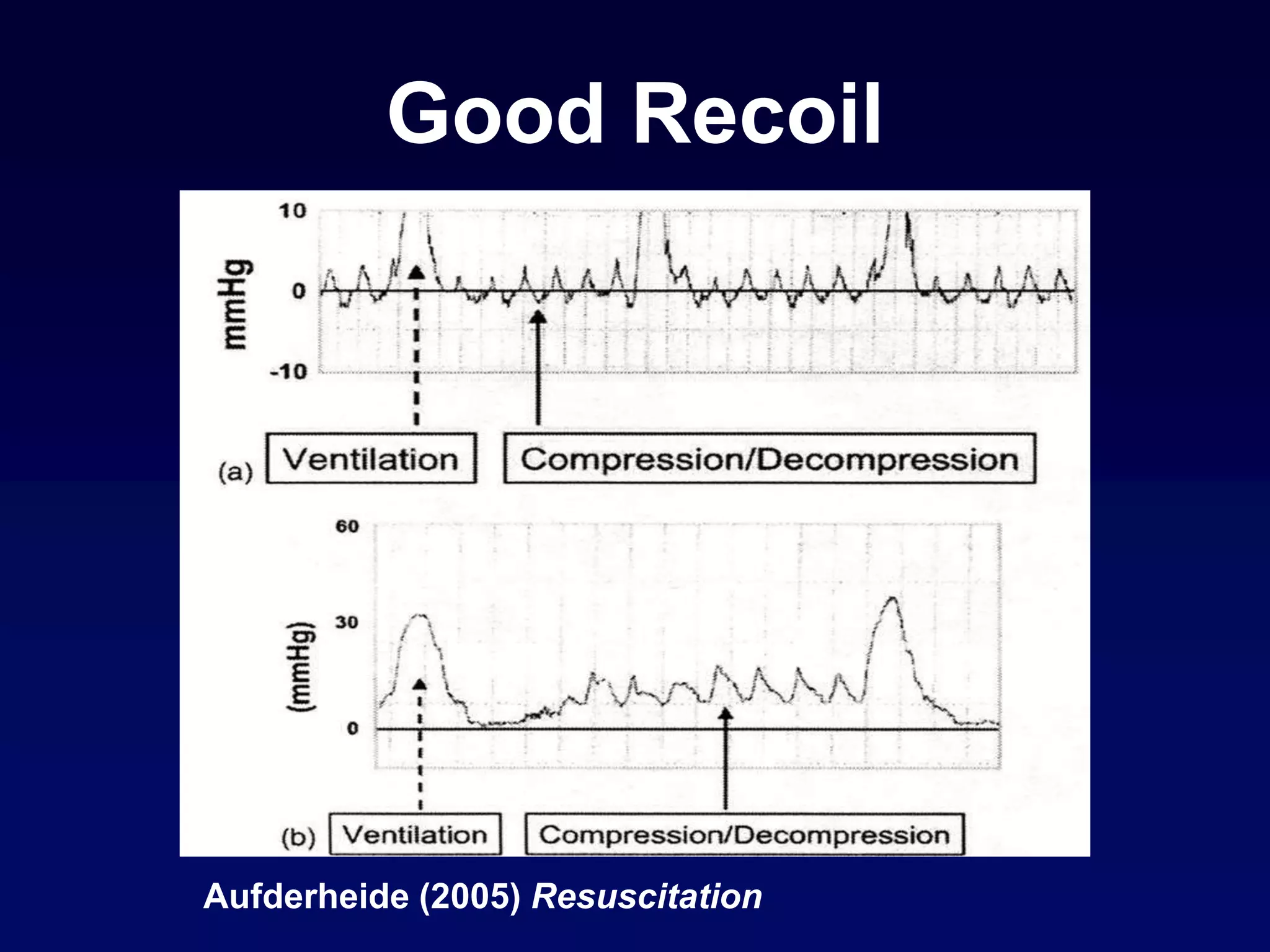
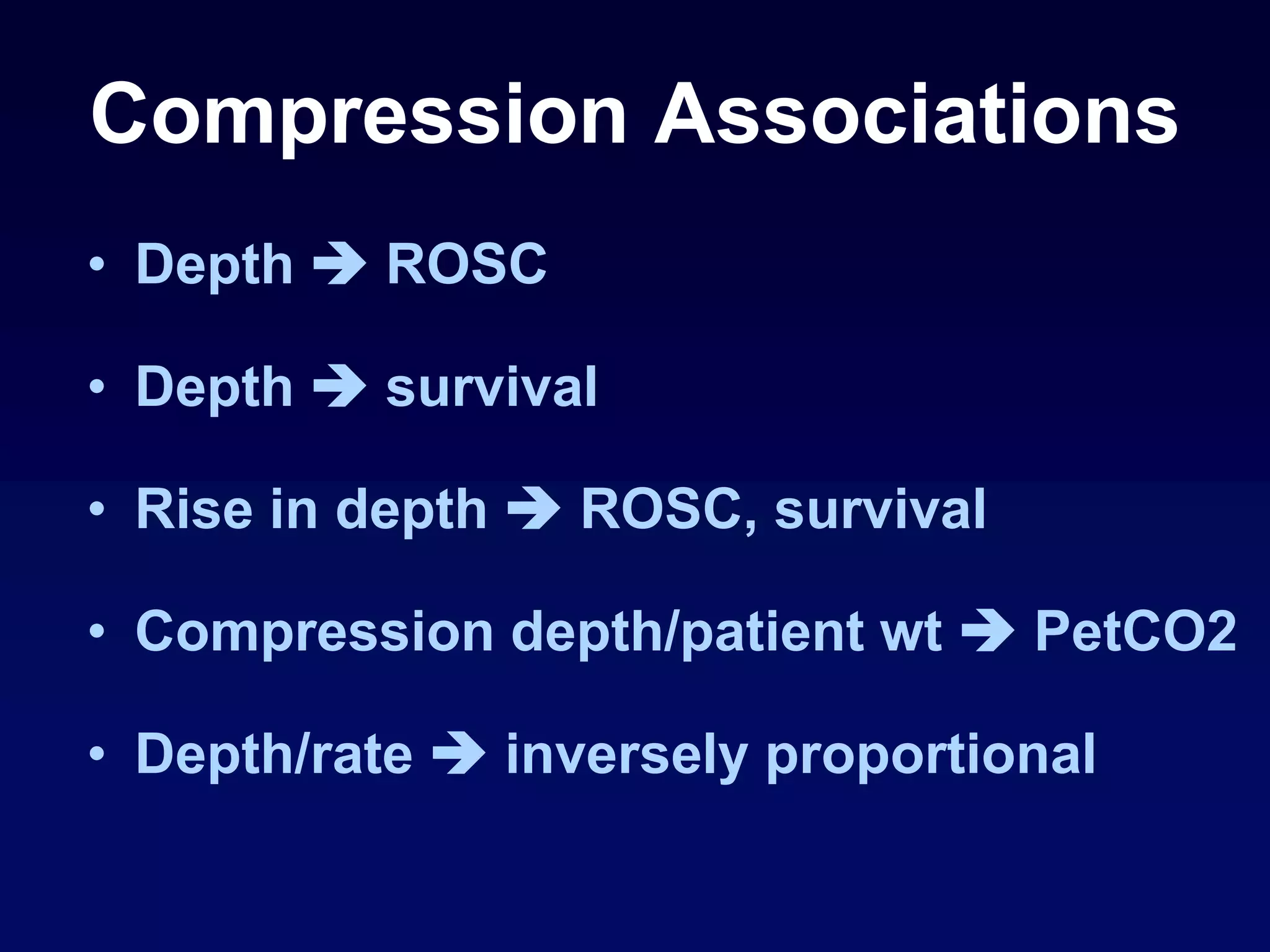
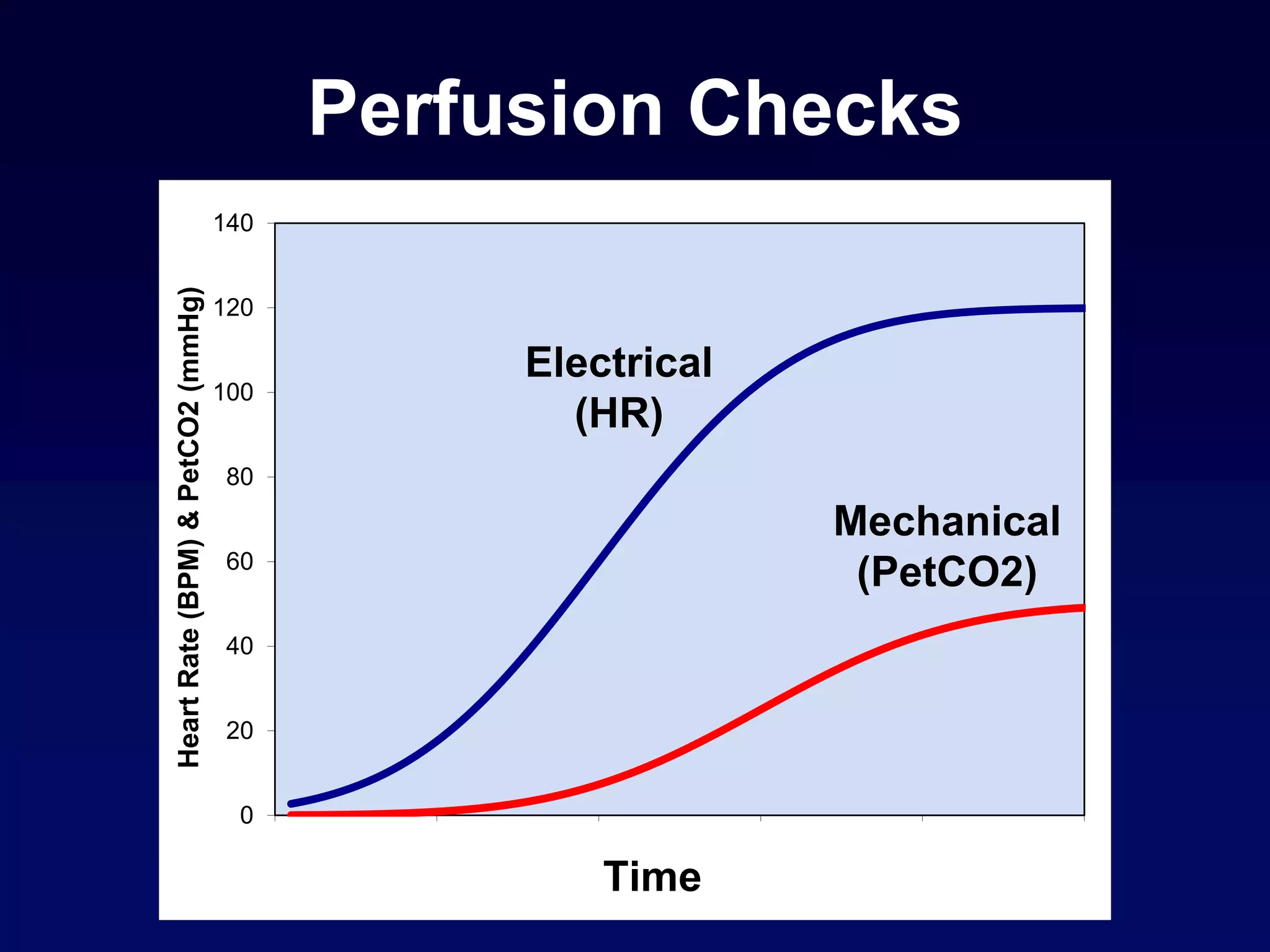
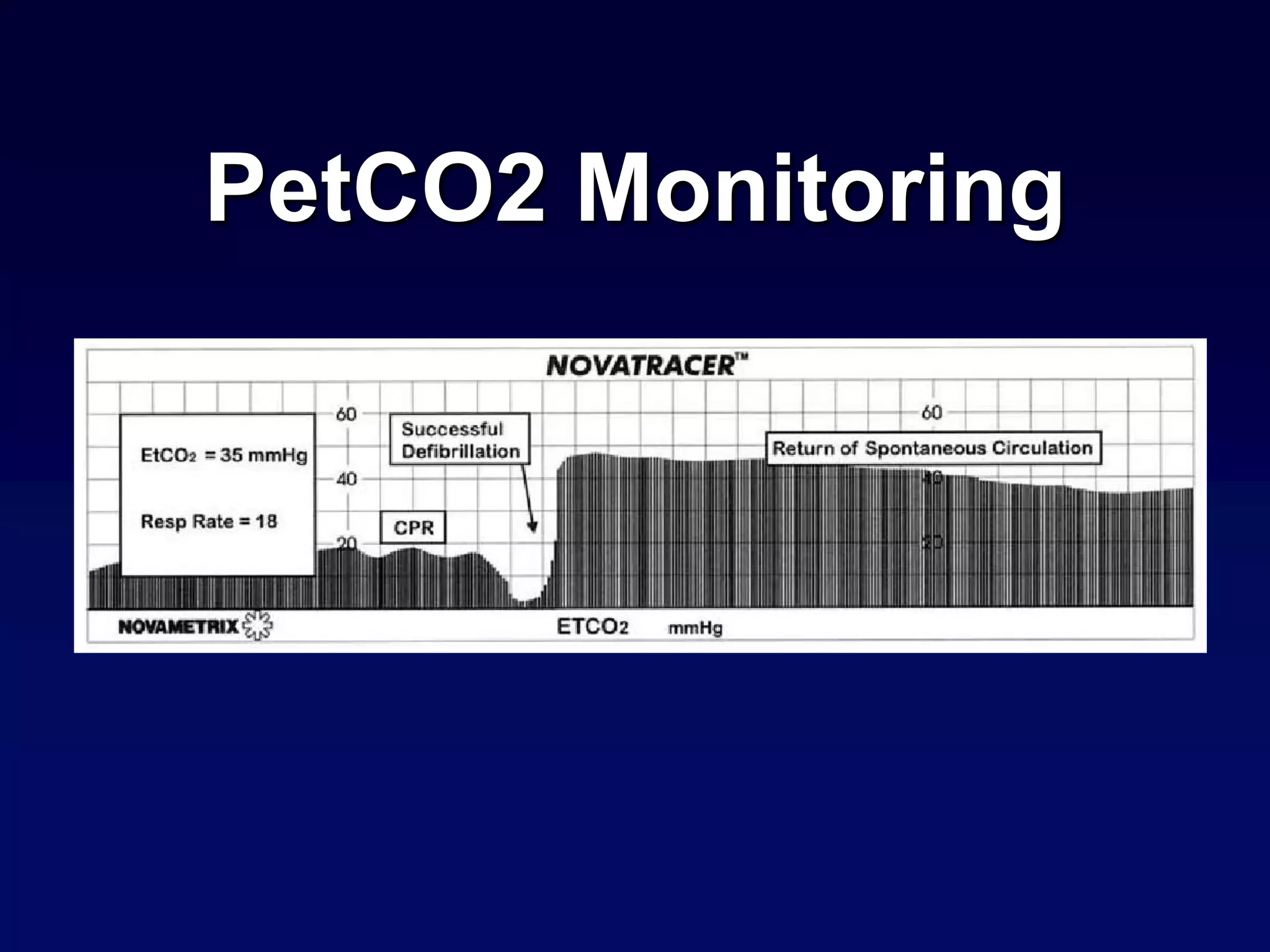
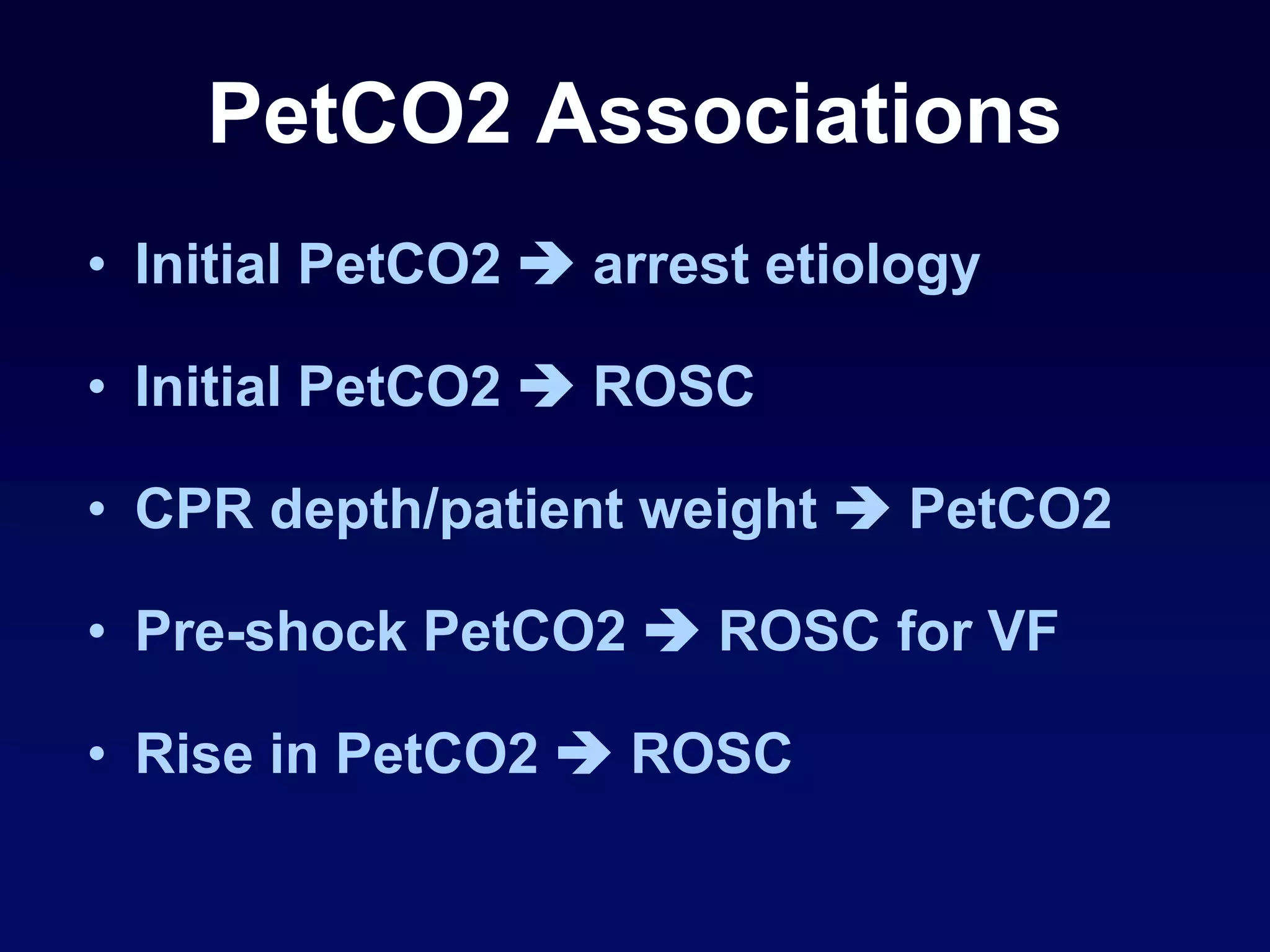
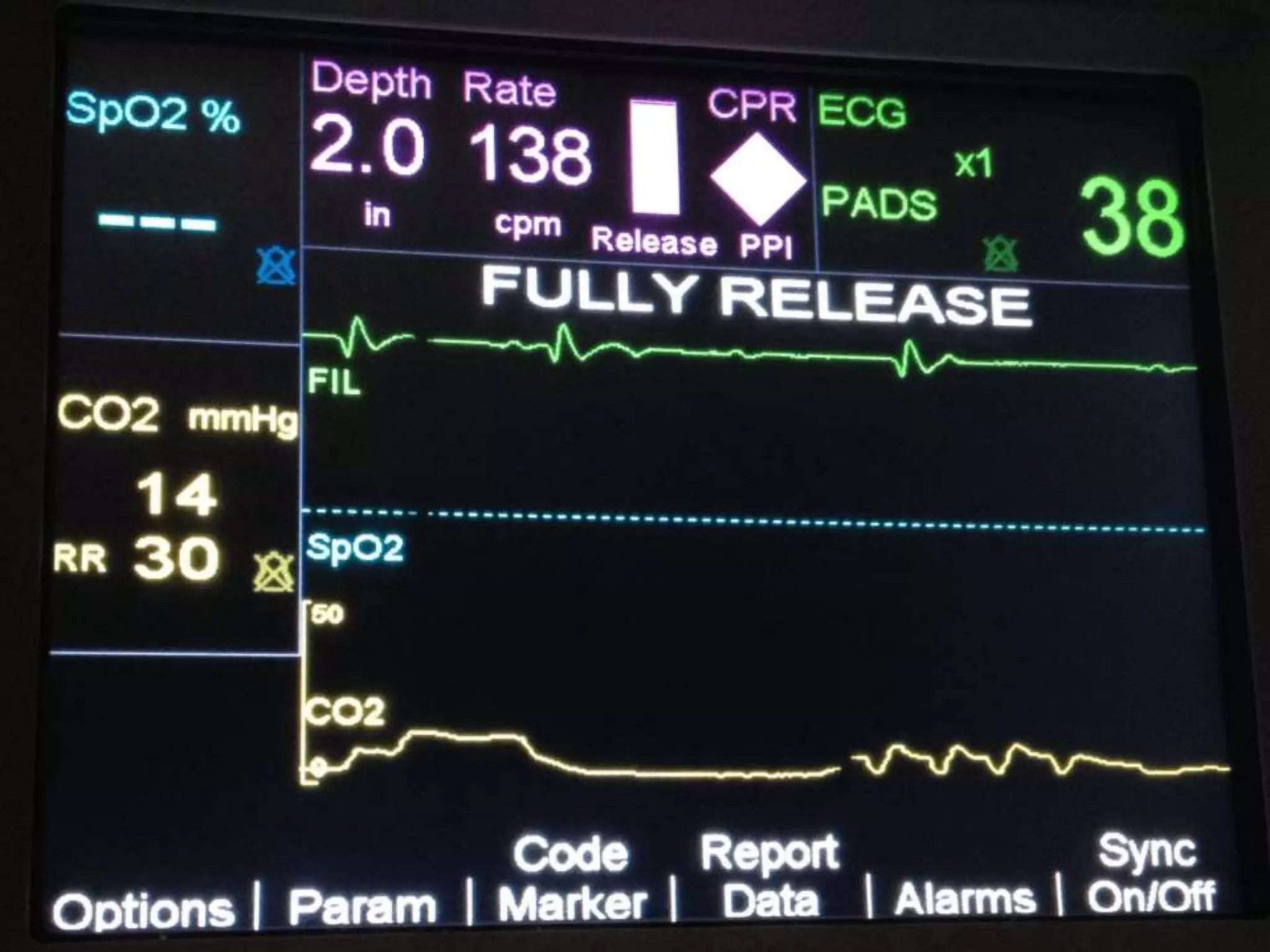
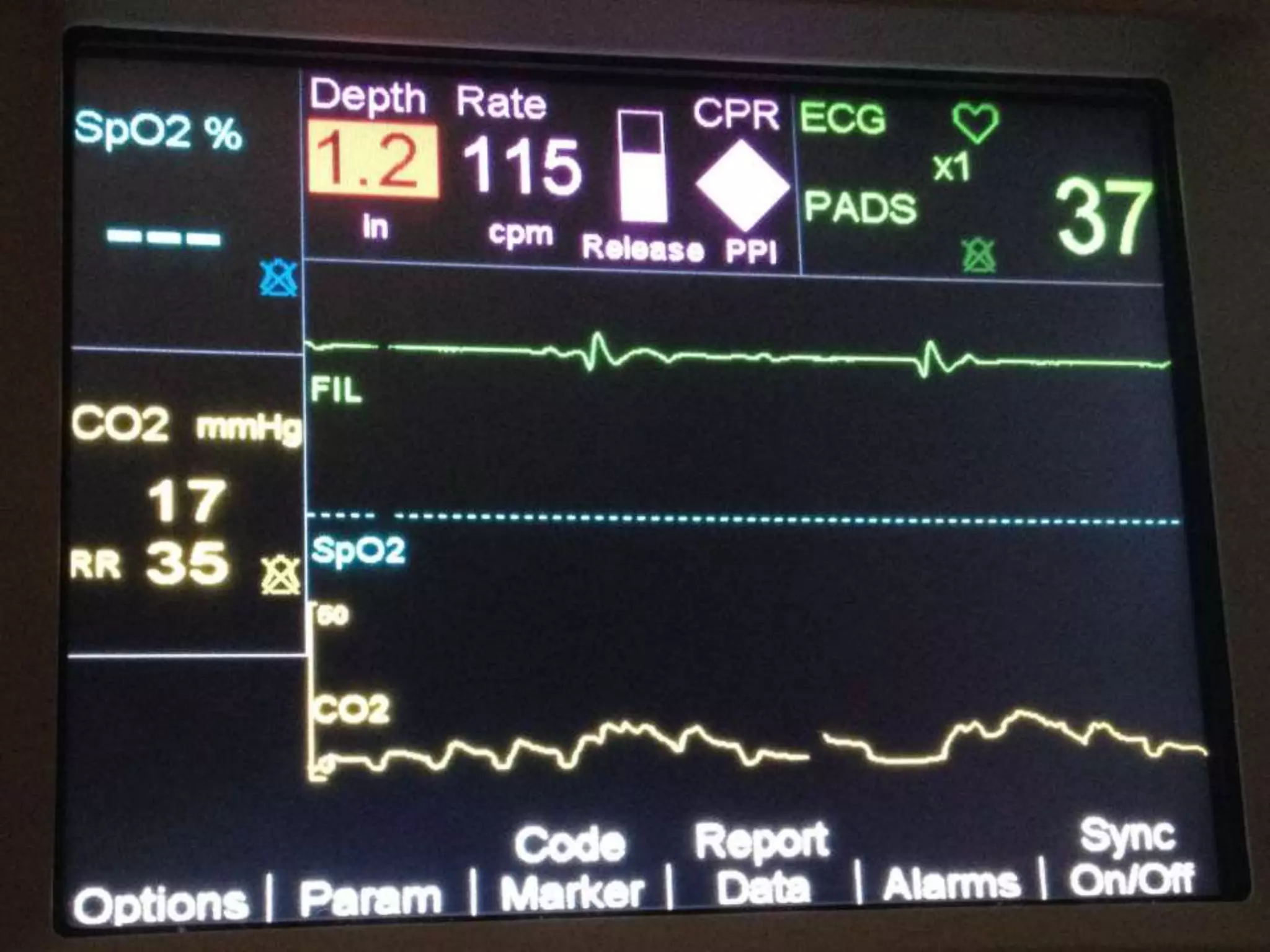
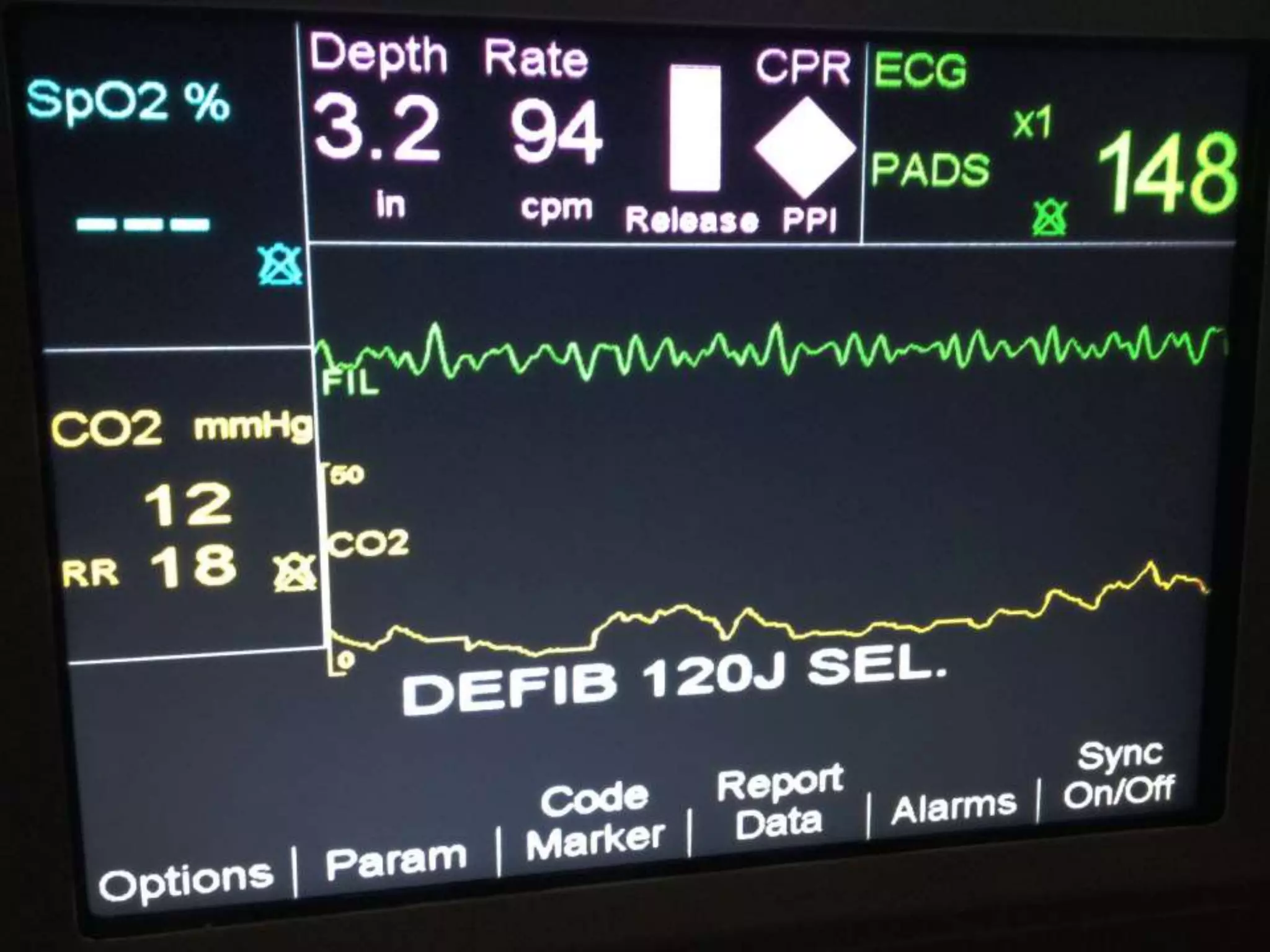
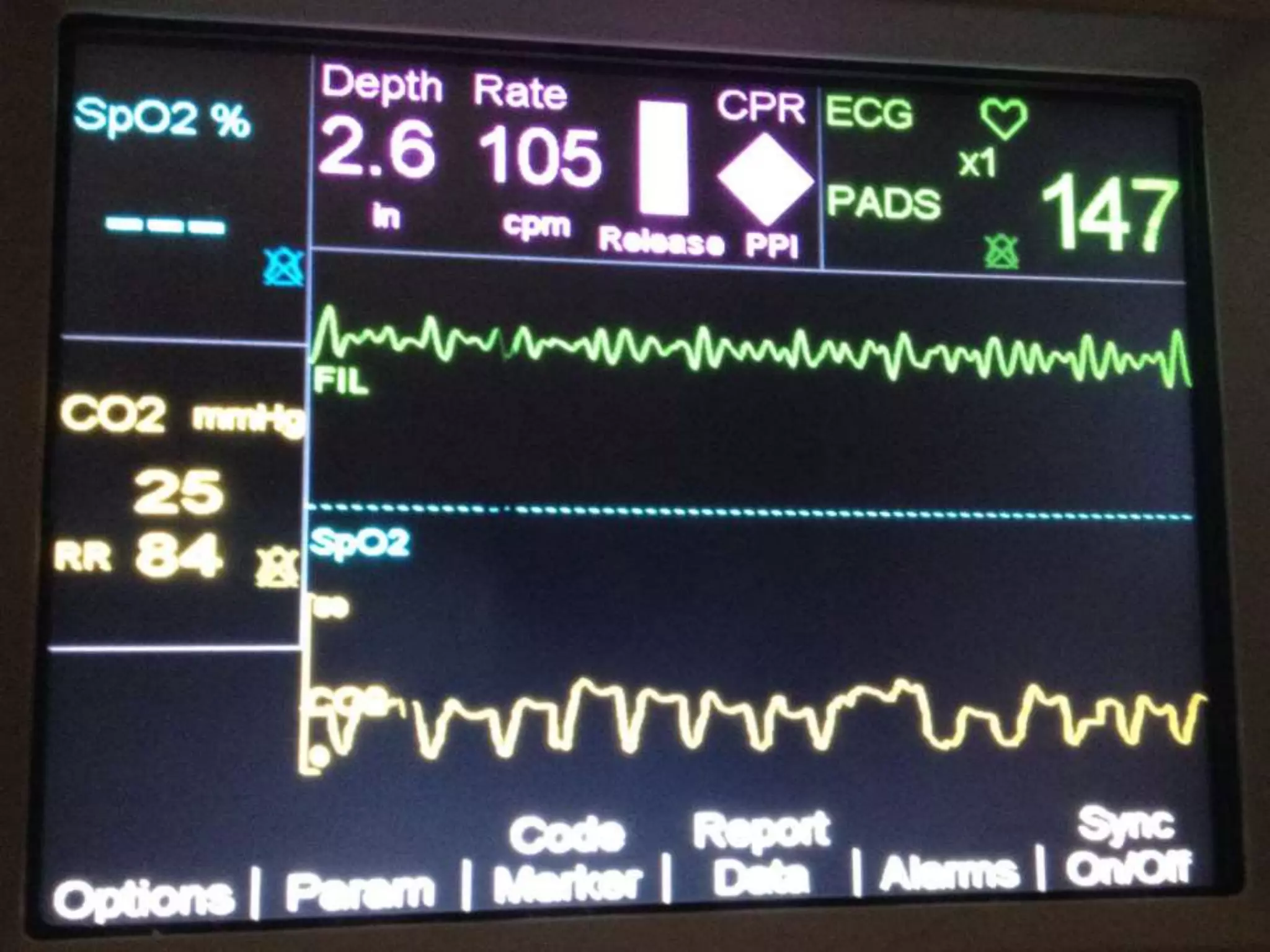
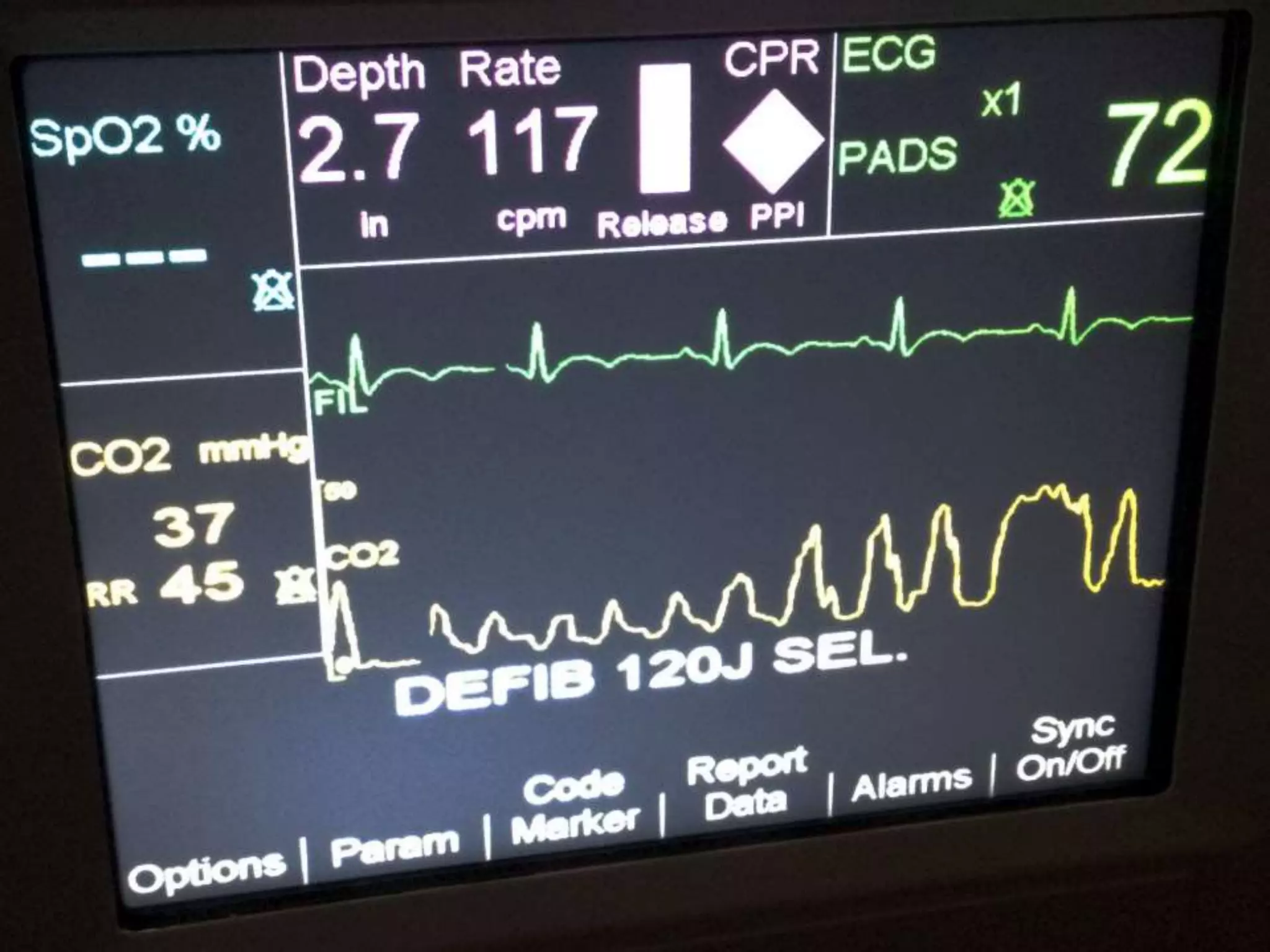
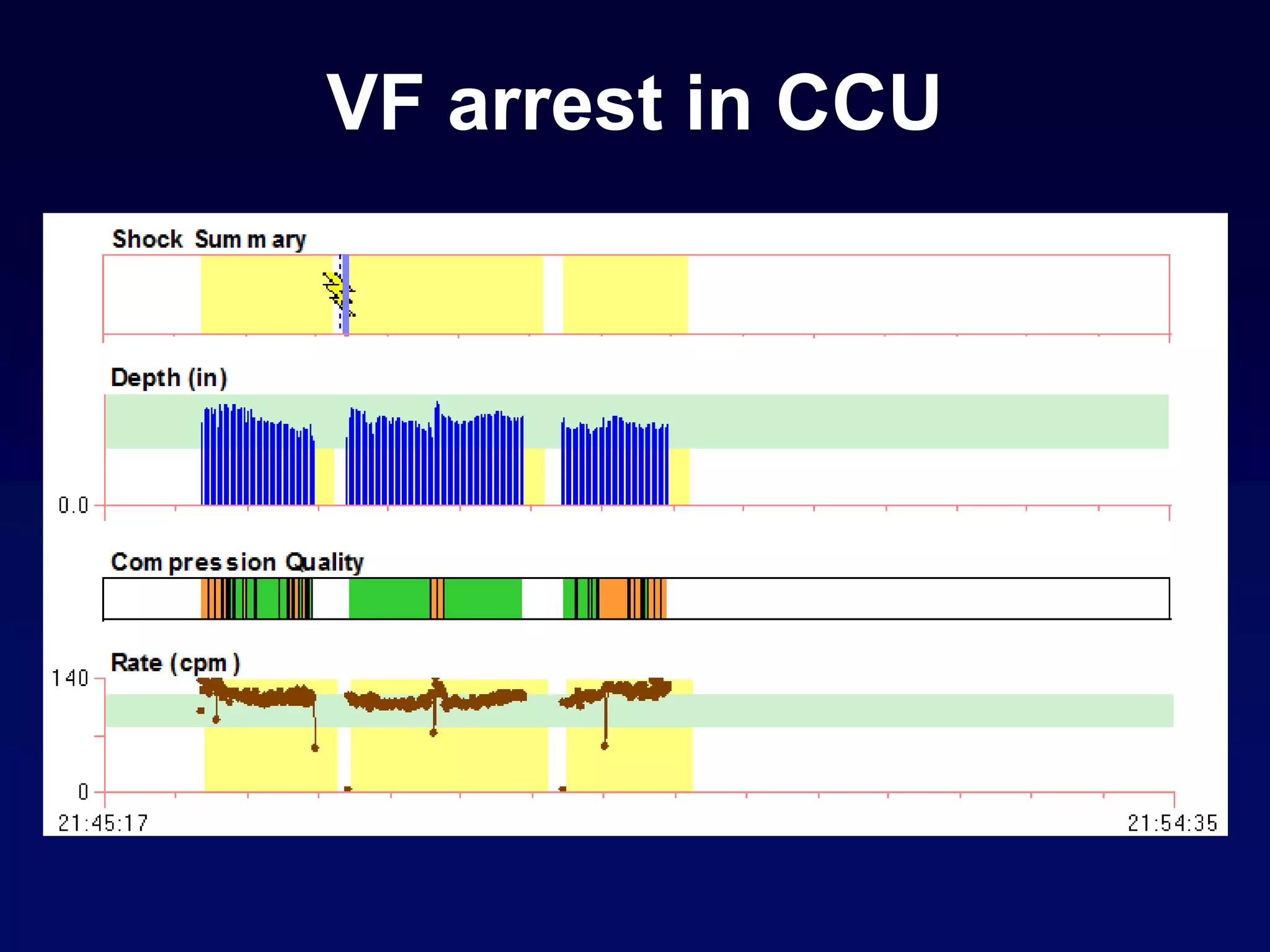
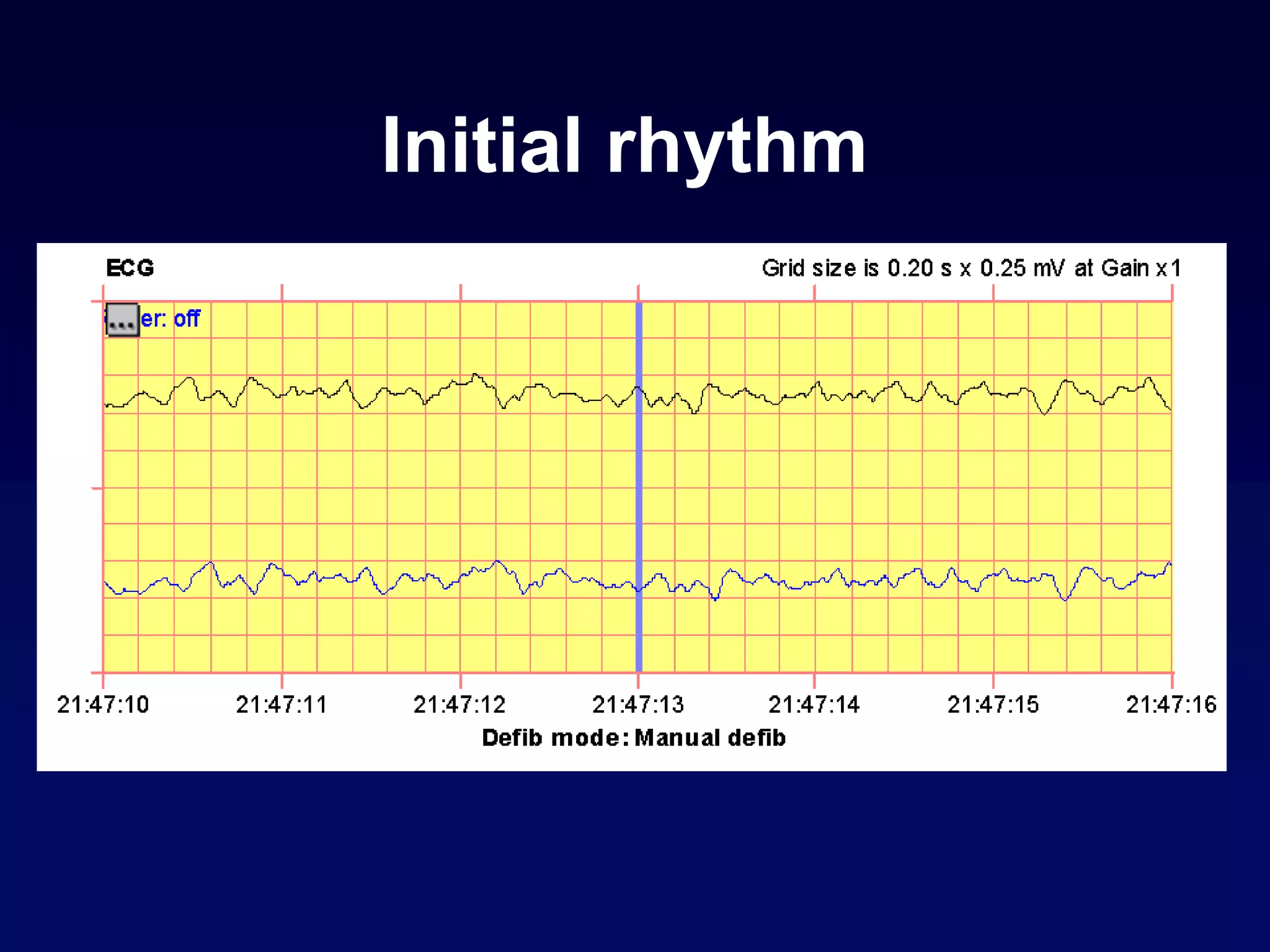
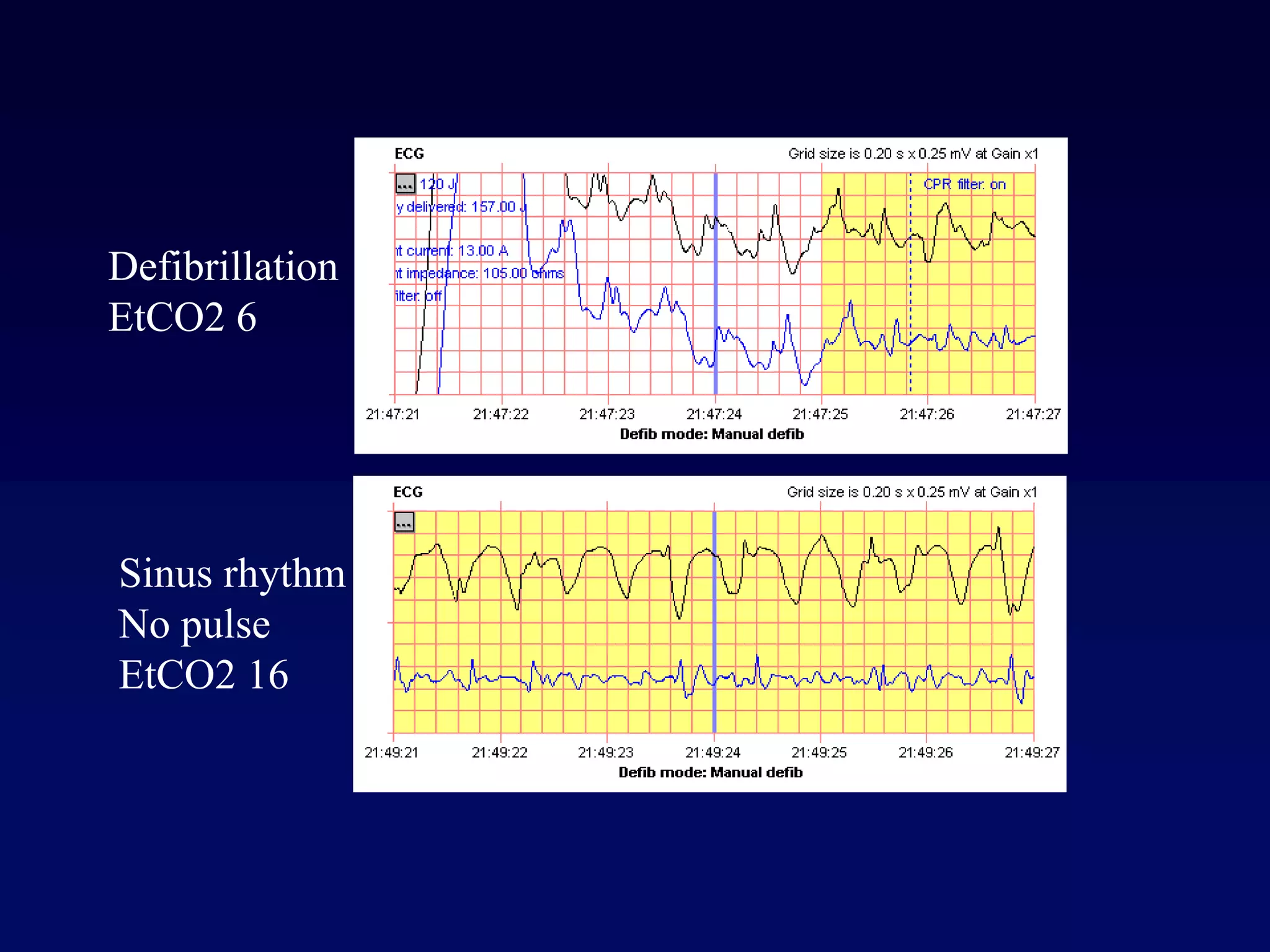
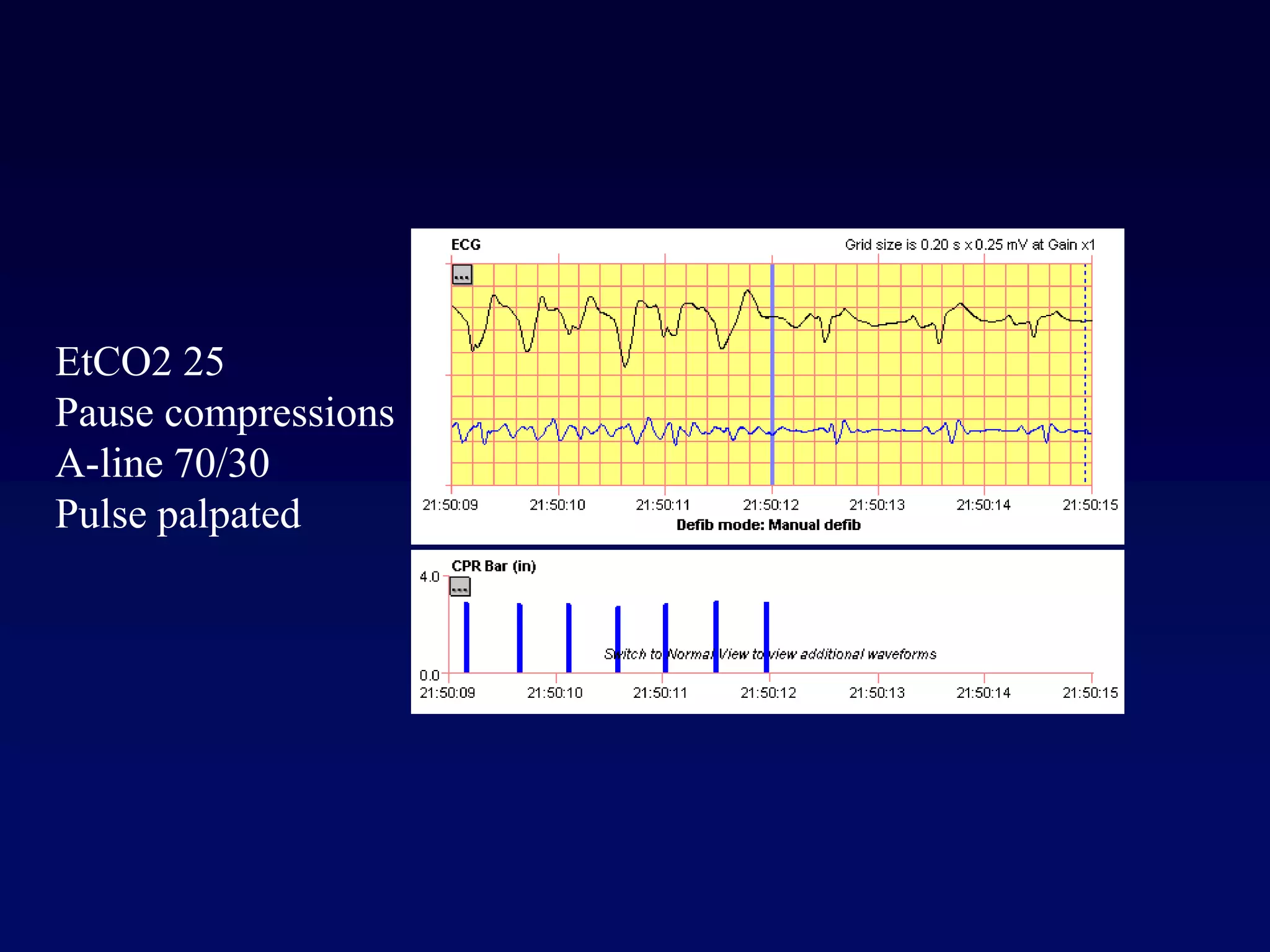
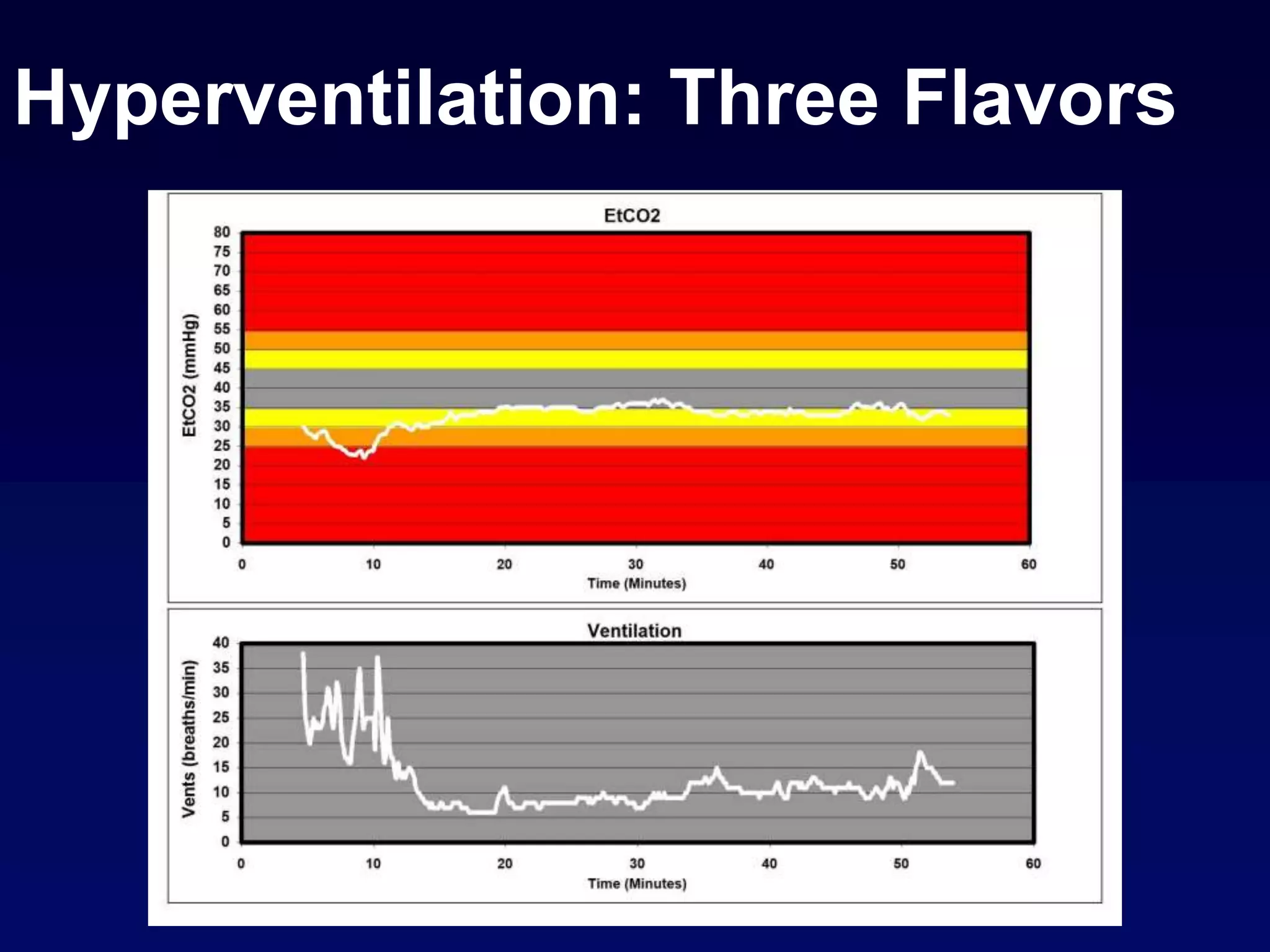
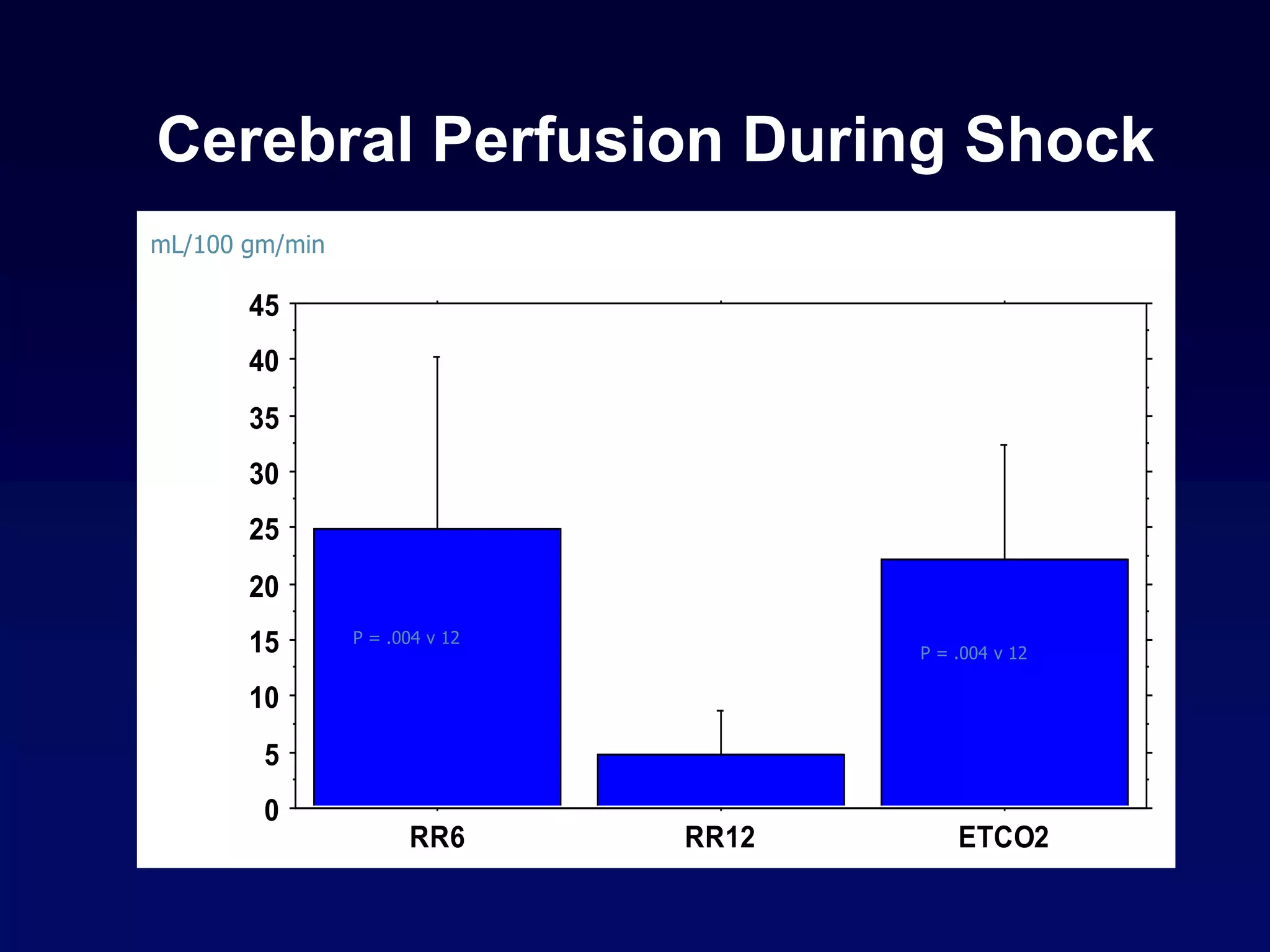
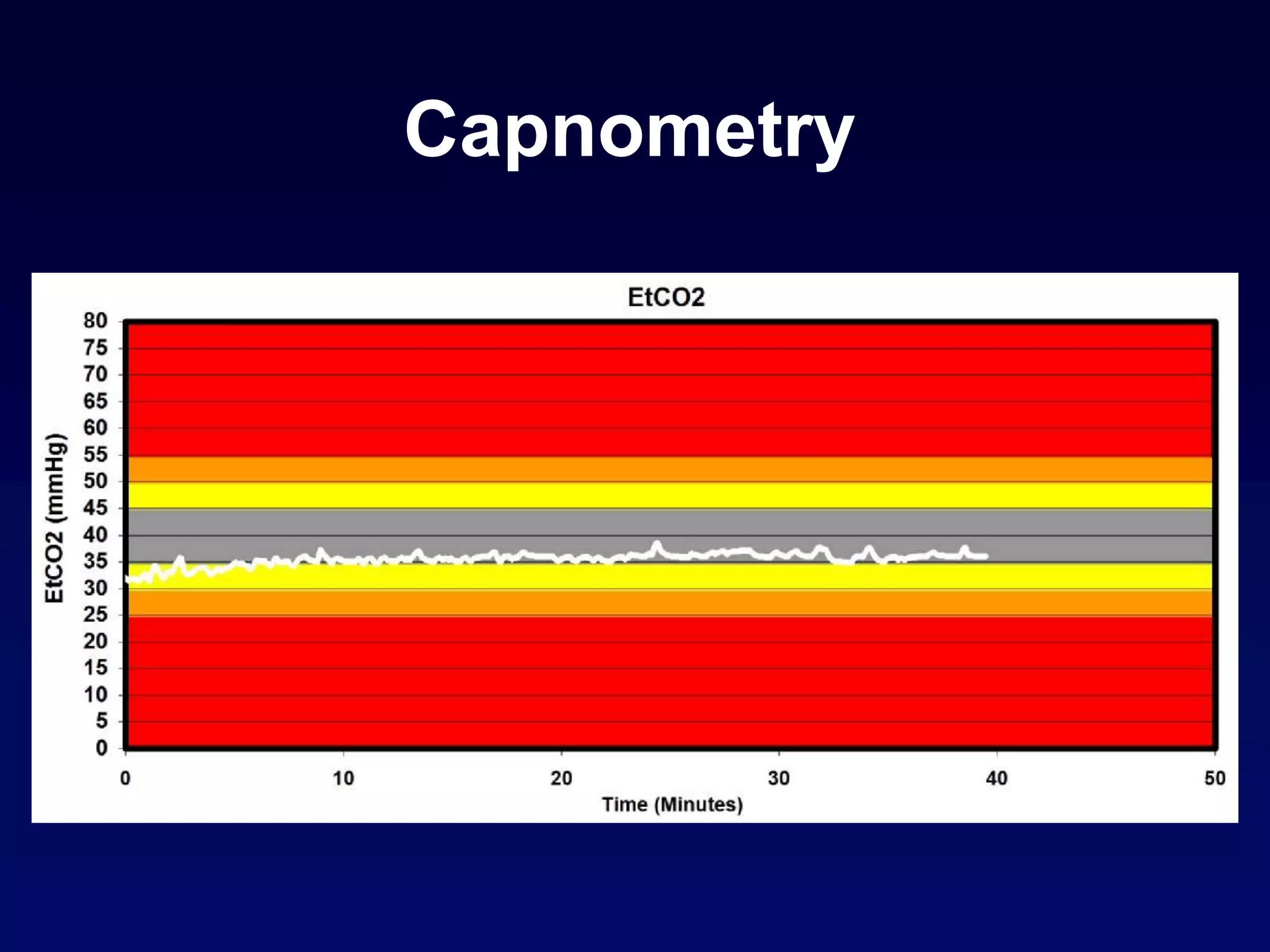
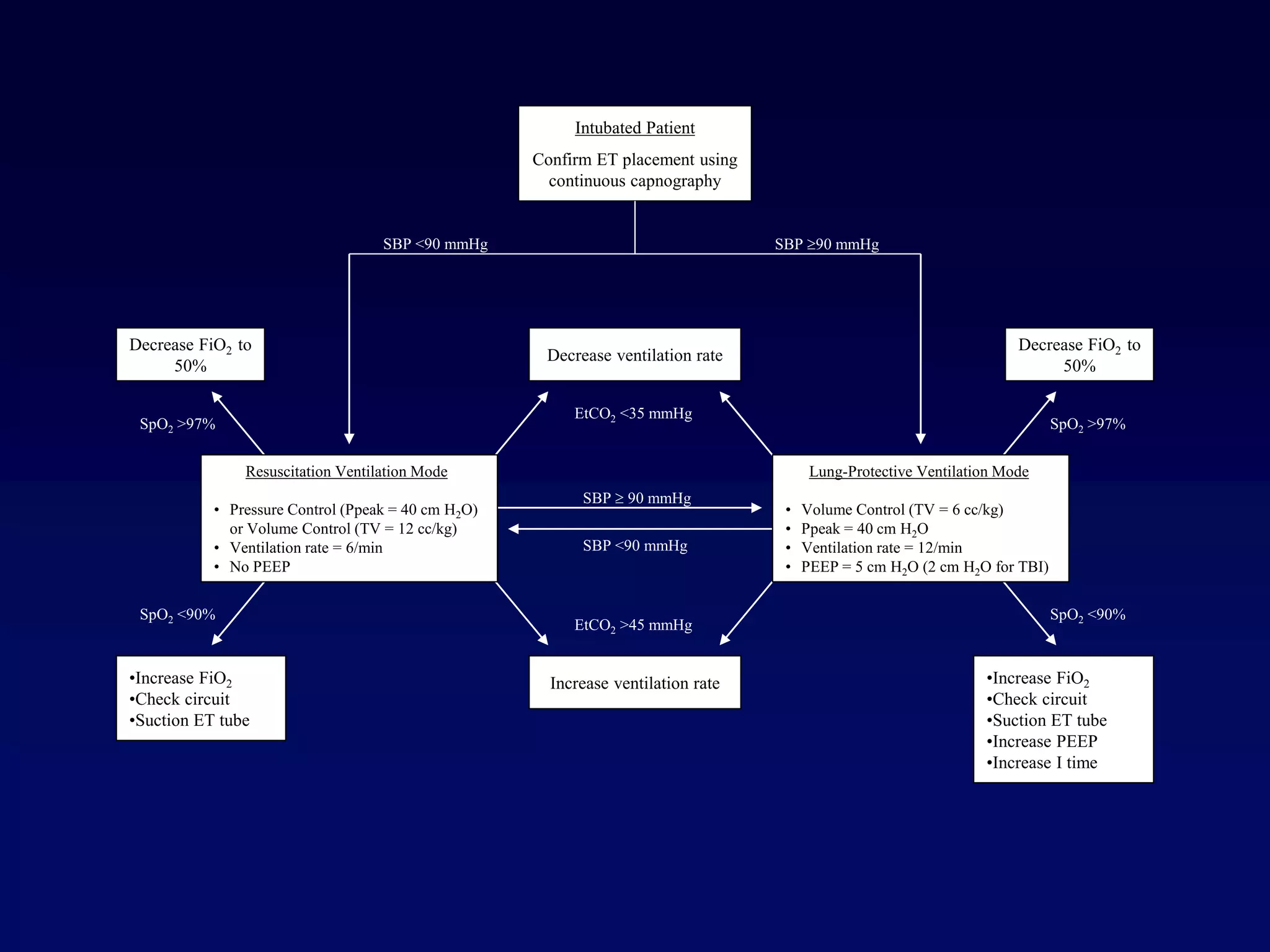
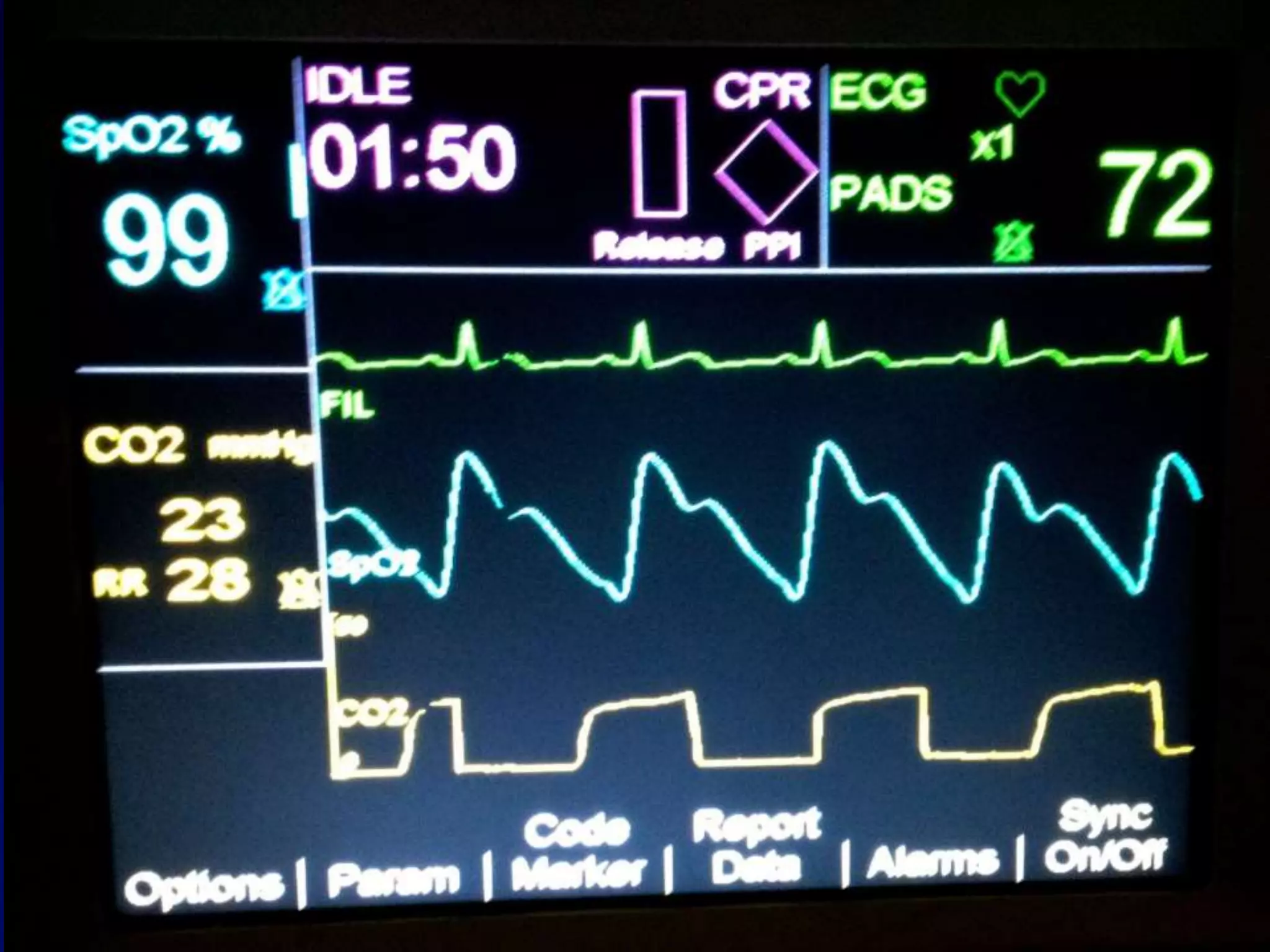
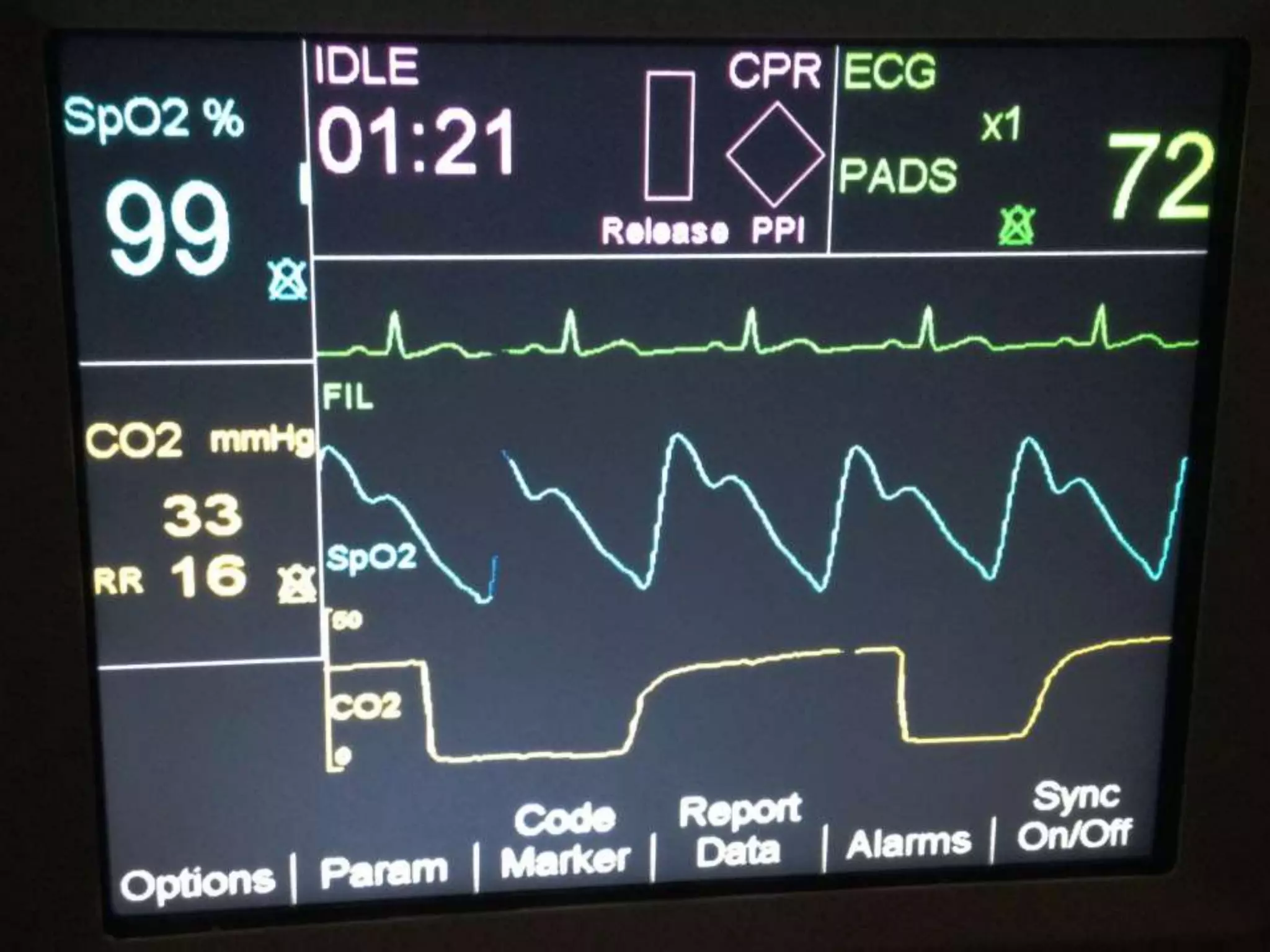
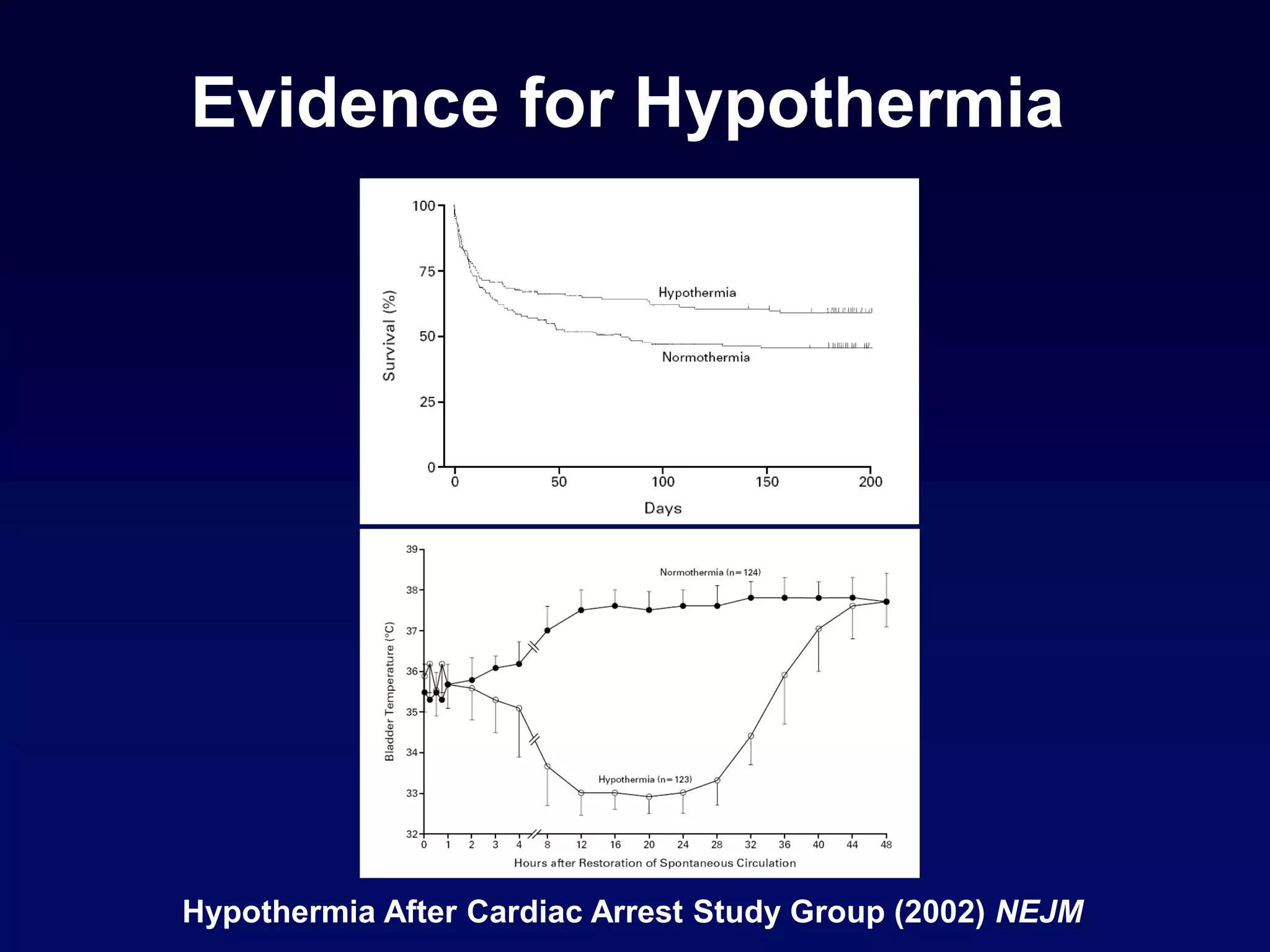
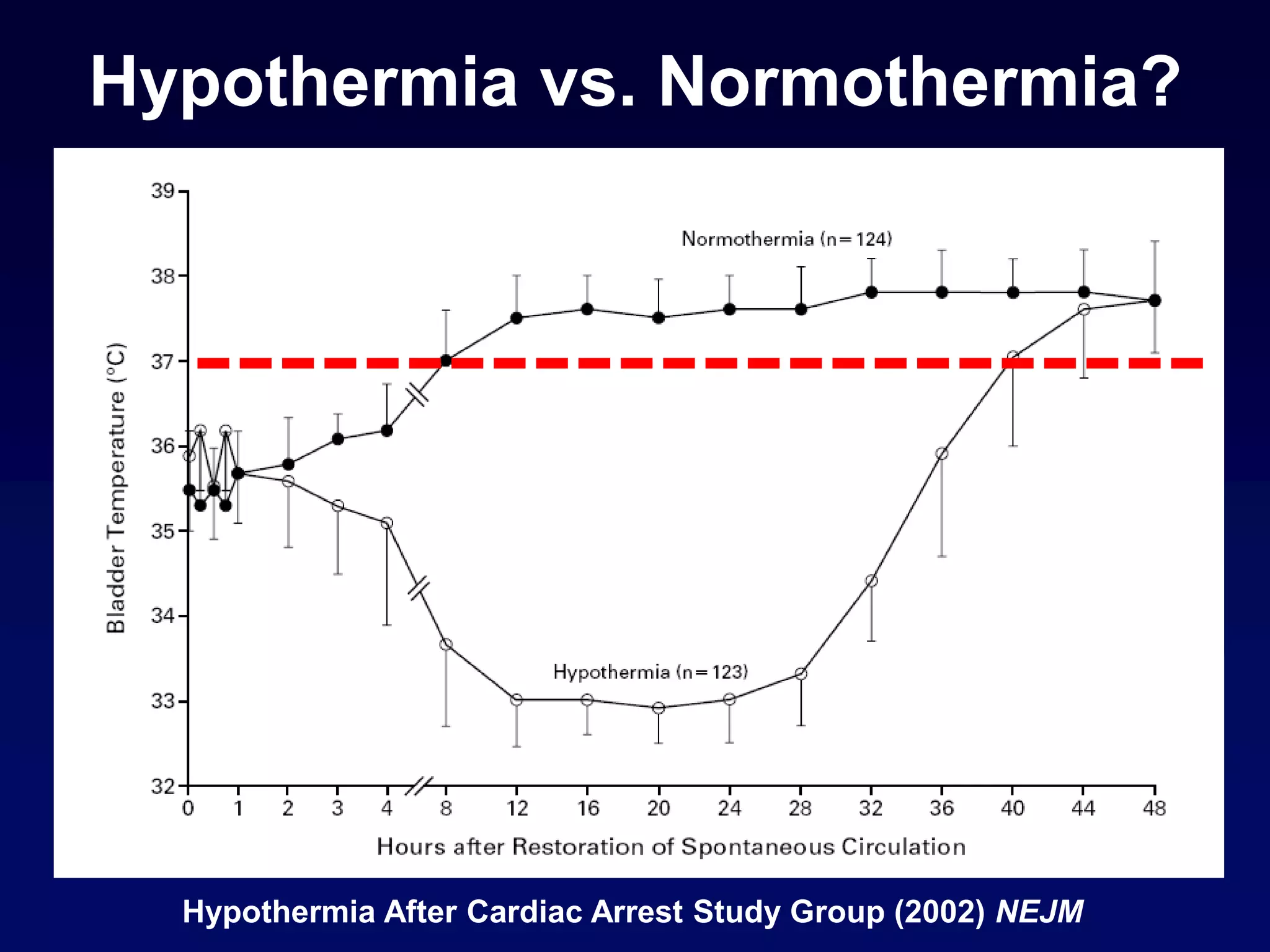
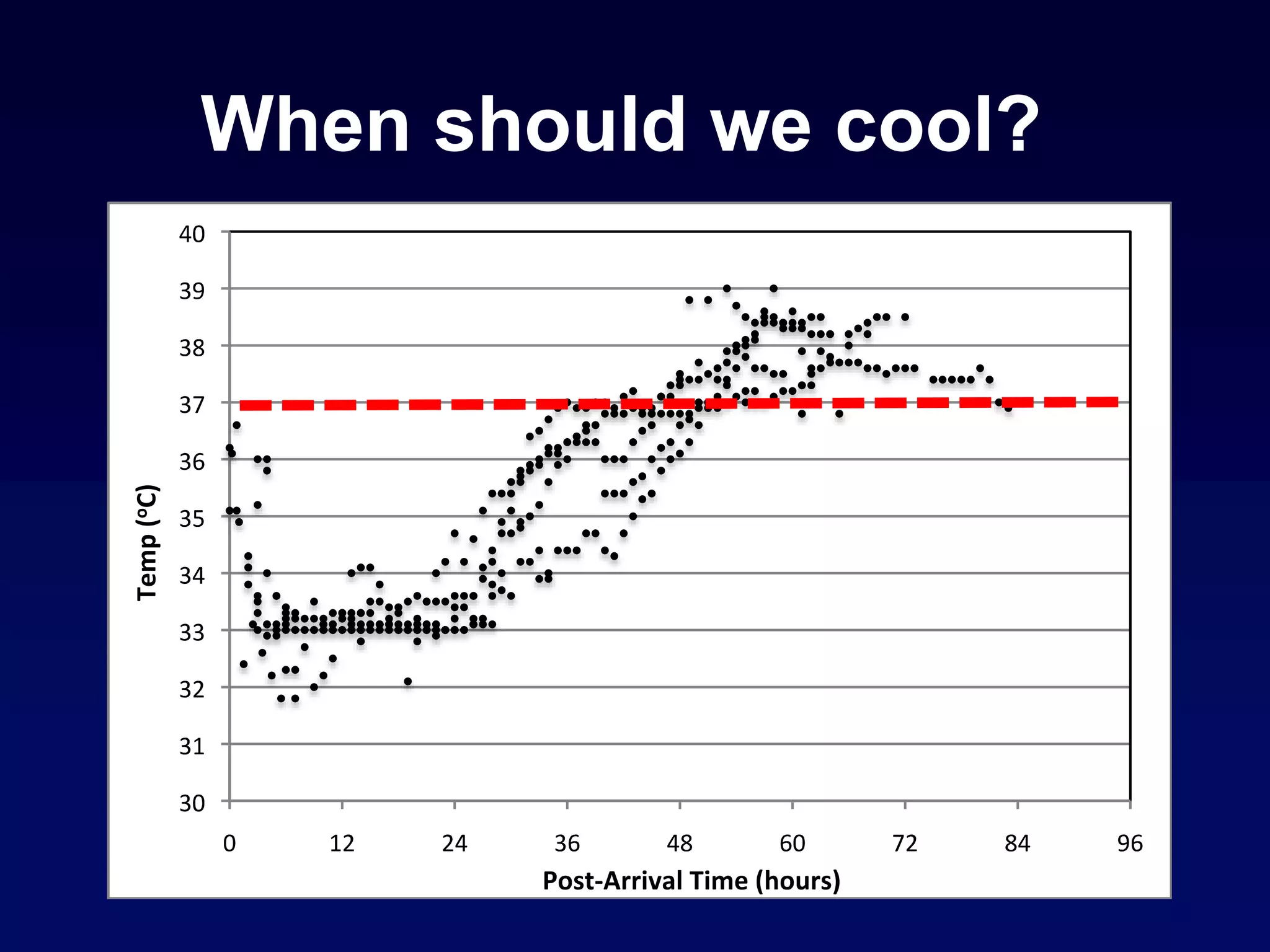
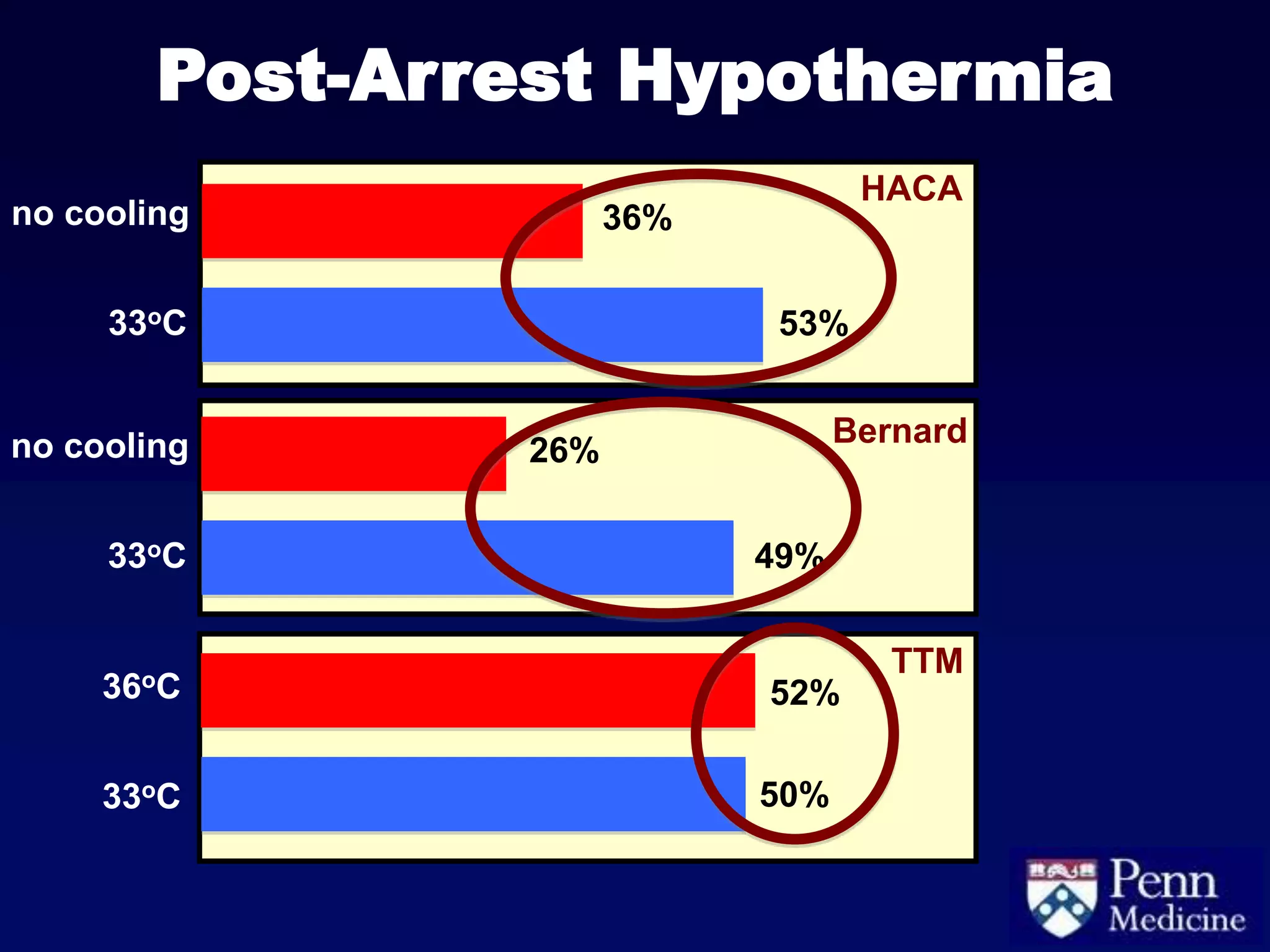
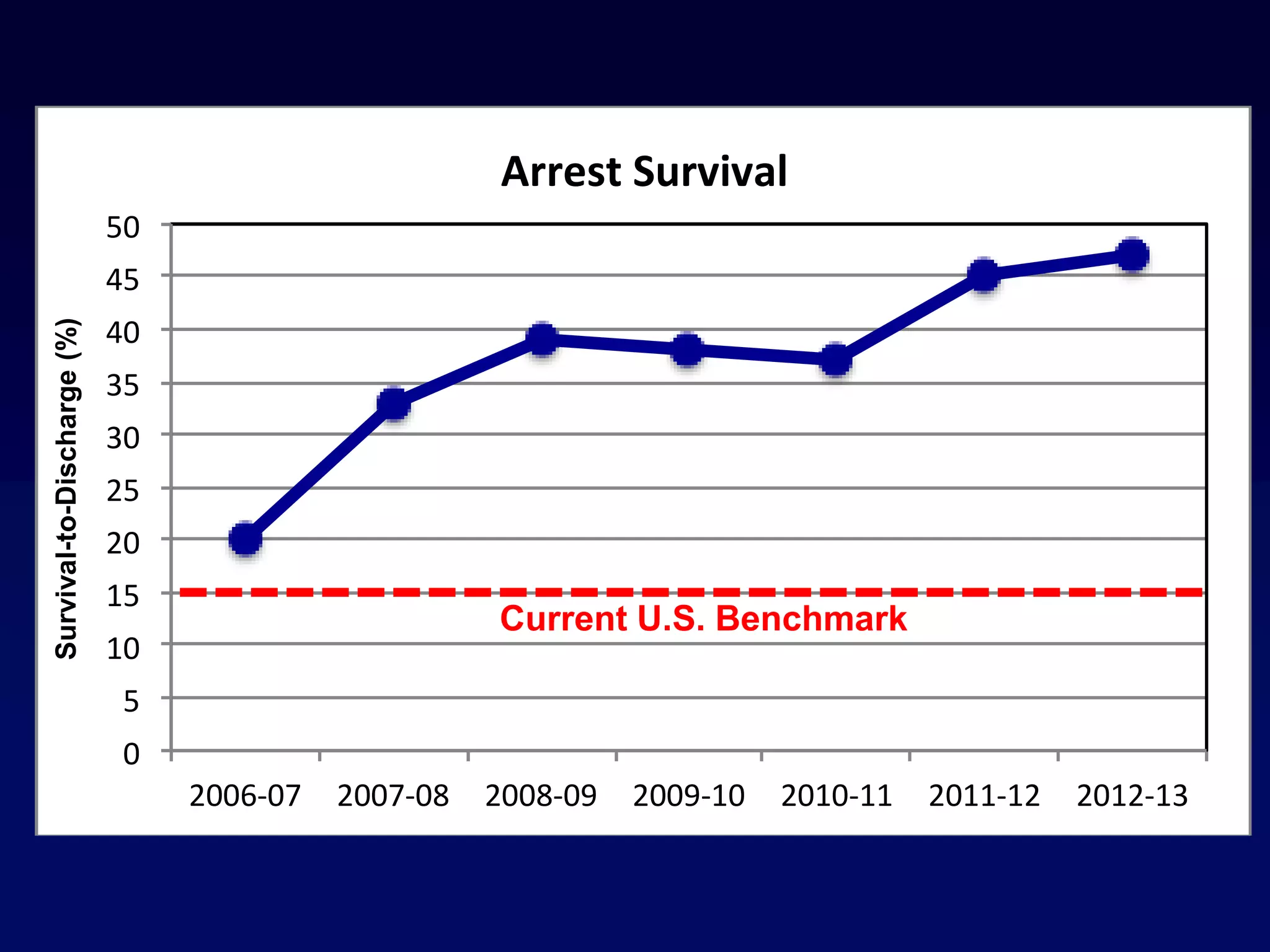
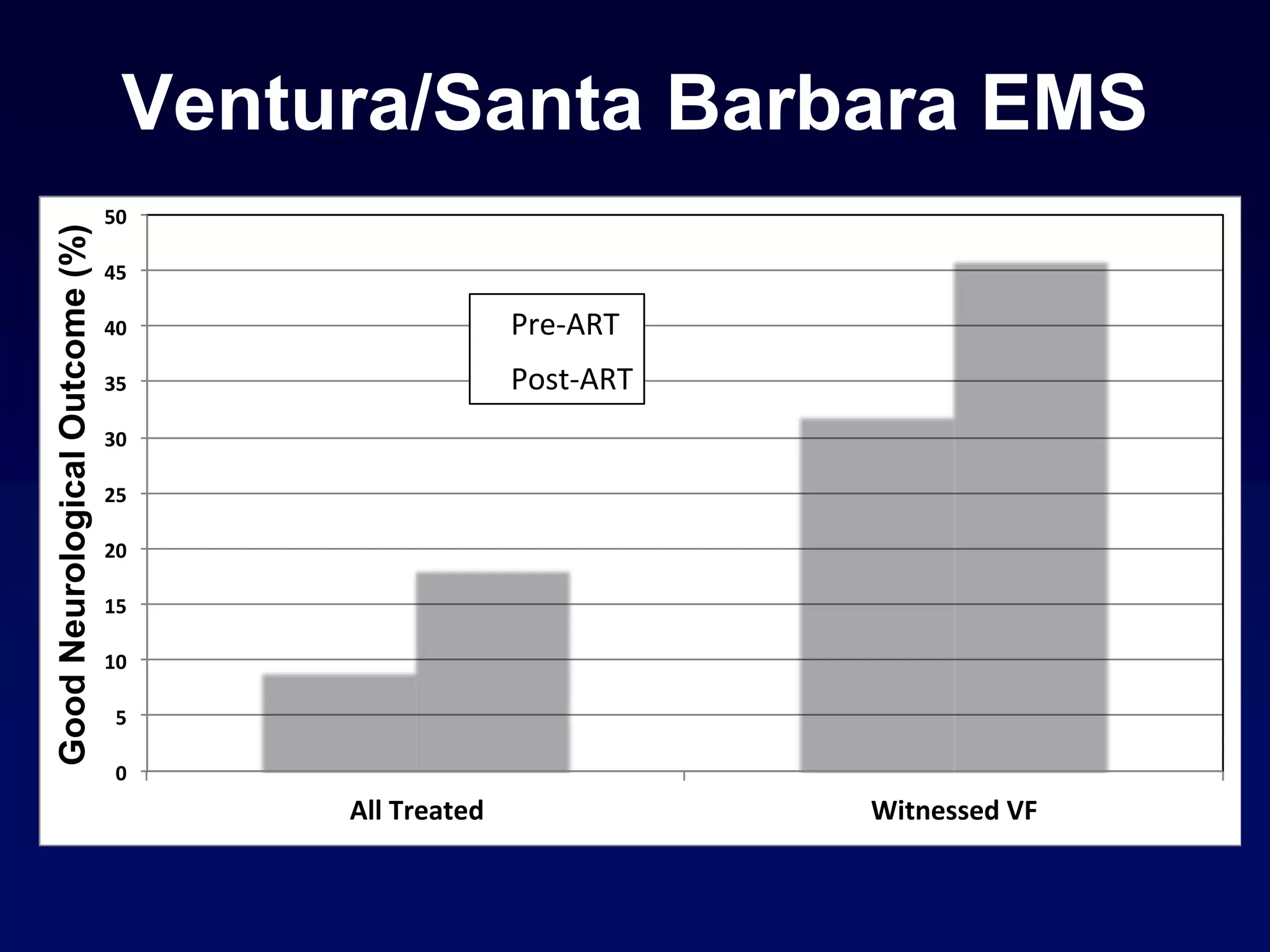
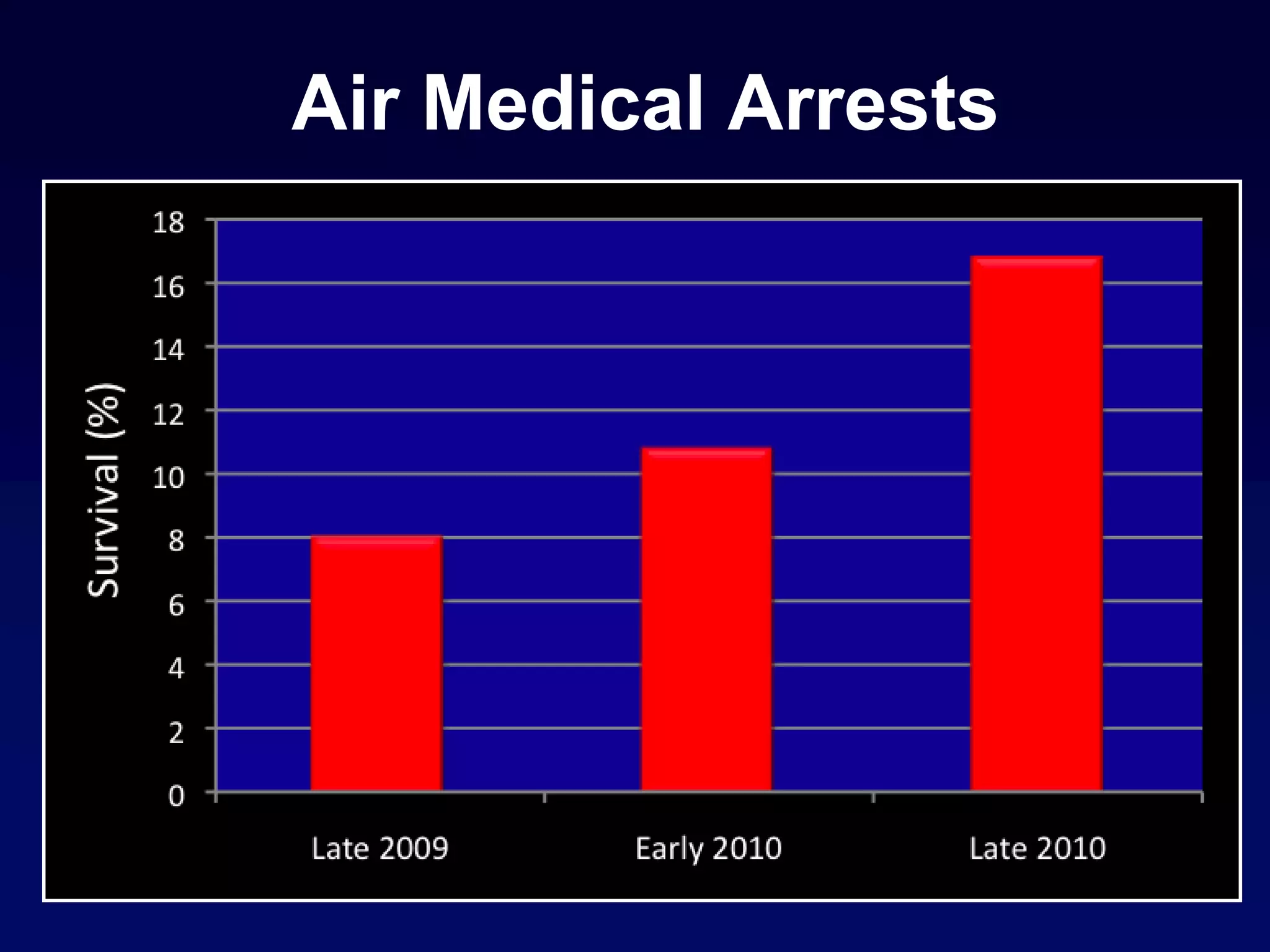
The document discusses the integration of technology in resuscitation practices, emphasizing the importance of continuous chest compressions and real-time feedback for performance improvement. It highlights the significance of compression depth and associated monitoring metrics, as well as the role of hypothermia in post-arrest management. Overall, the document presents evidence-based approaches to enhance survival rates and outcomes in cardiac arrest scenarios.