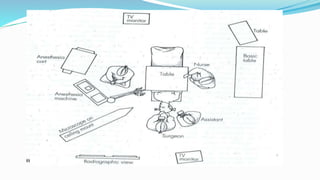
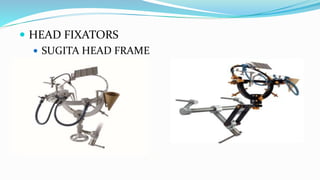
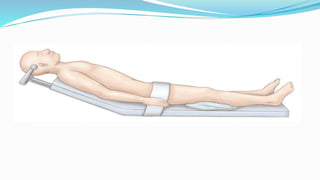
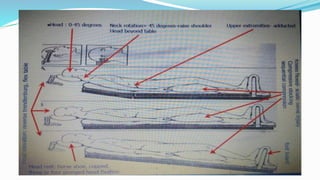
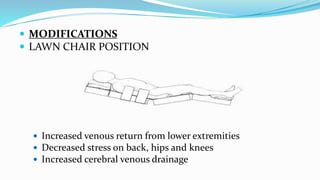
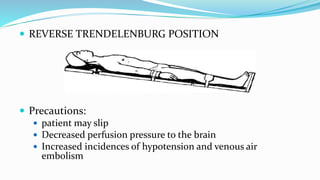
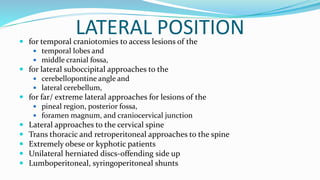
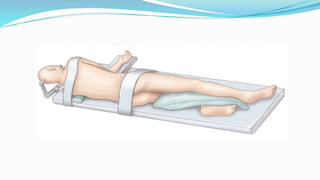
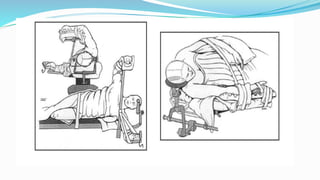
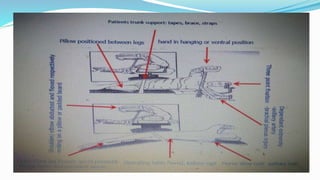
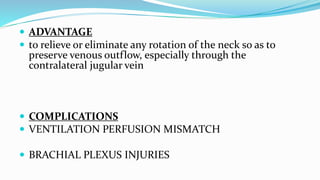
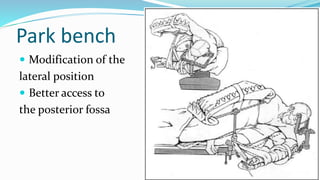
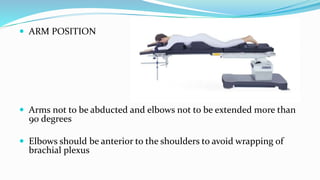
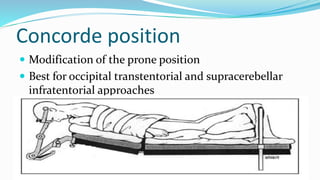
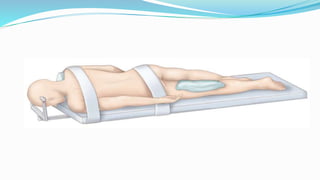
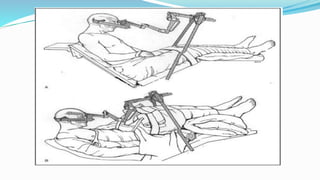
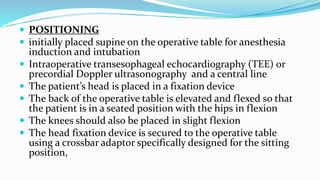
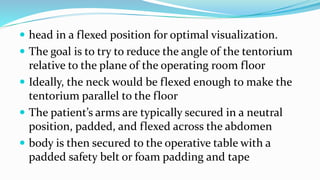
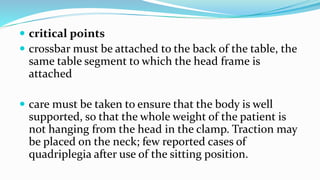
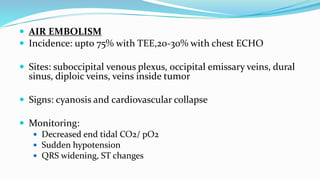
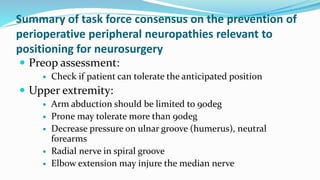
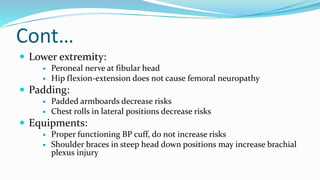
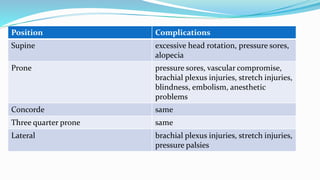
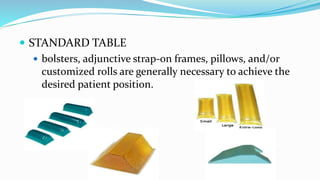
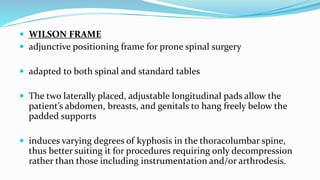
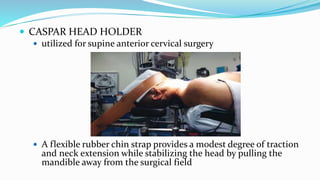
This document discusses various positioning considerations for cranial surgery. It outlines different positions used including supine, lateral, prone, sitting, and variations. Key factors in positioning include access, comfort, safety, and reducing complications. Positions are chosen based on the surgical site and individual patient factors. Proper positioning is important to optimize exposure and outcomes while preventing pressure injuries and neurological complications.