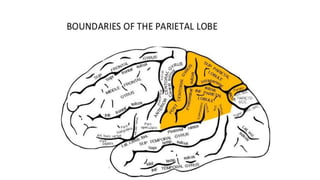
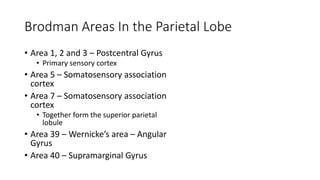
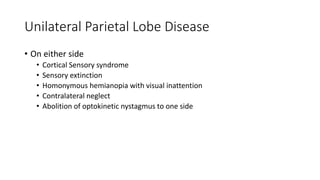
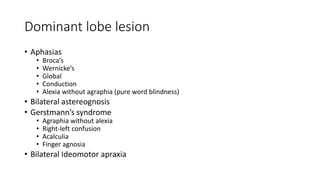
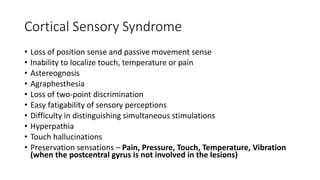
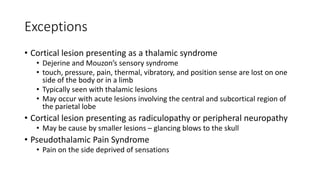
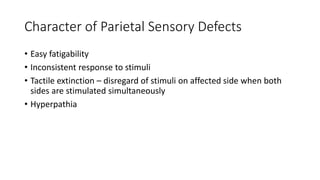
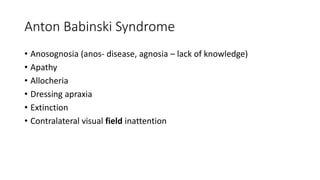
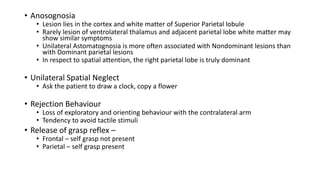
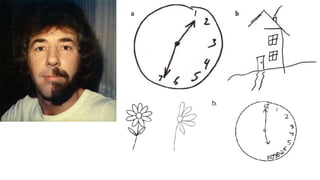
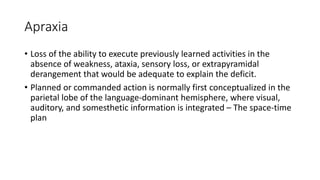
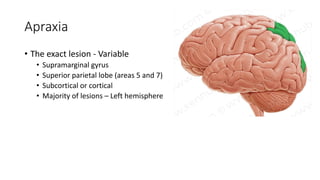
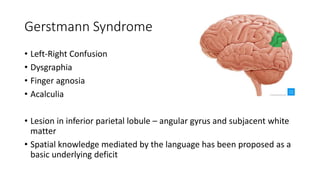
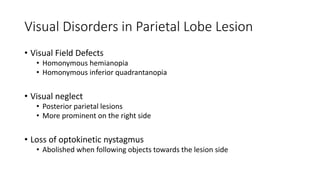
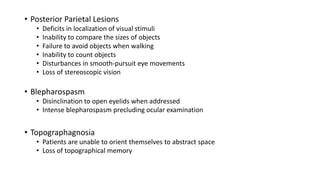
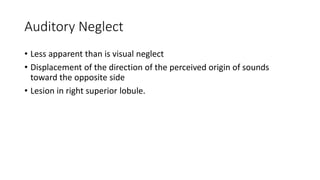
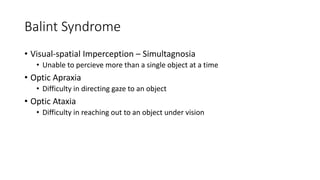
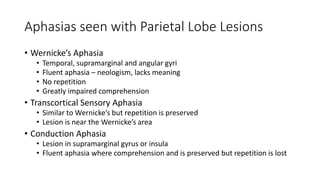
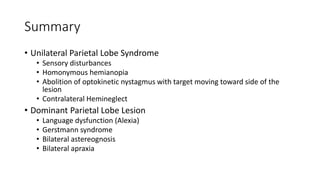
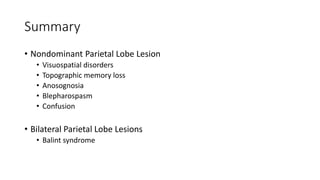
The parietal lobe is involved in sensory processing, spatial awareness, and motor coordination. Unilateral lesions can cause sensory deficits, visual field cuts, and neglect of the opposite side of space. Bilateral lesions are associated with Balint's syndrome of simultanagnosia, optic ataxia, and ocular apraxia. Dominant parietal lesions may induce Gerstmann syndrome, alexia, or conduction aphasia, while nondominant lesions can result in anosognosia, topographic disorientation, and blepharospasm.