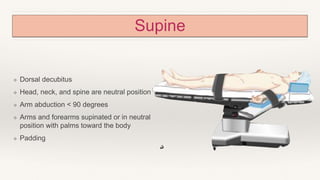
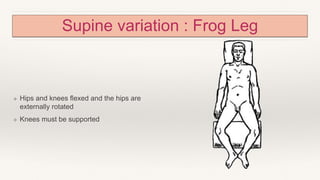
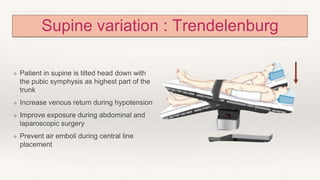
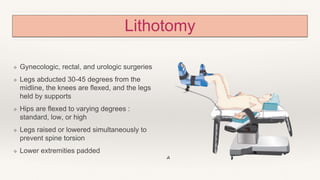
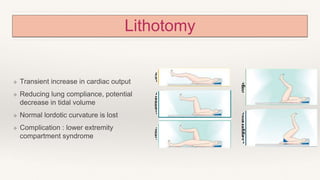
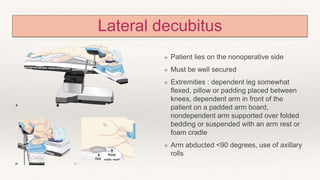
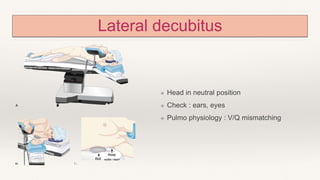
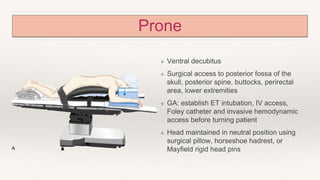
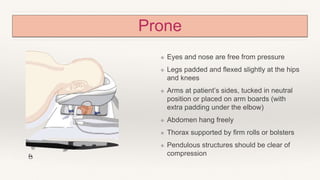
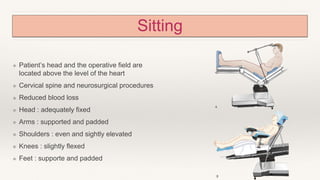
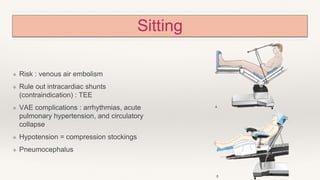
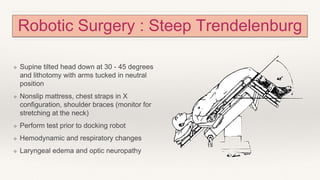
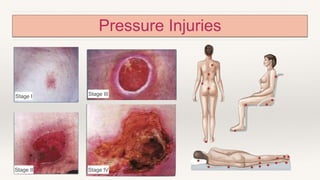
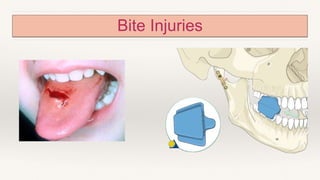
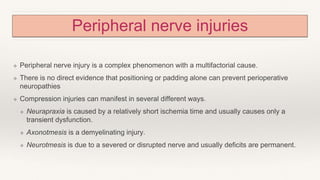
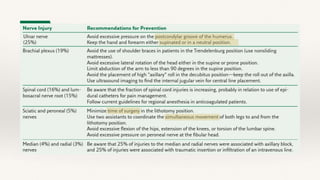
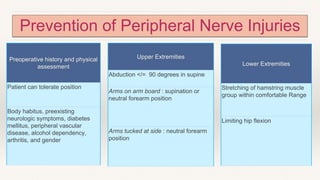
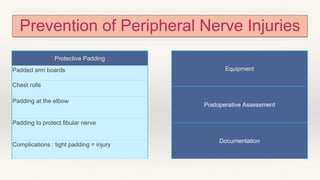
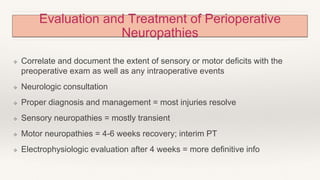
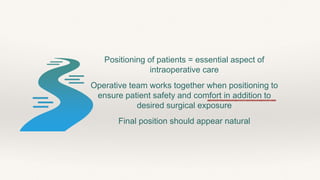
The document outlines the importance of proper patient positioning during surgical procedures, detailing various positions such as supine, lithotomy, lateral decubitus, prone, and sitting, along with associated physiological risks and complications. It emphasizes the role of surgical teams in ensuring patient safety, comfort, and optimal surgical exposure while considering factors like hemodynamics and respiratory function. Additionally, it addresses the prevention of peripheral nerve injuries and postoperative complications, such as eye injuries and visual loss.