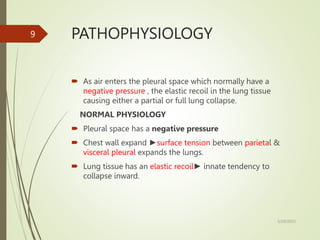
The document discusses pneumothorax and its management. It defines pneumothorax as the presence of air in the pleural cavity, causing partial or full lung collapse. It describes the classification, causes, clinical presentation and investigations of pneumothorax. Needle decompression or chest drain insertion are the initial management steps, while VATS or open thoracostomy may be needed for persistent or traumatic cases. Complications can include respiratory failure, cardiac arrest or hemopneumothorax.