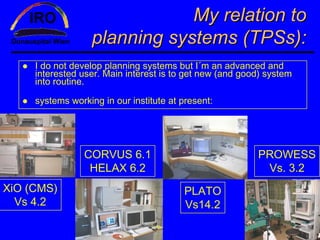
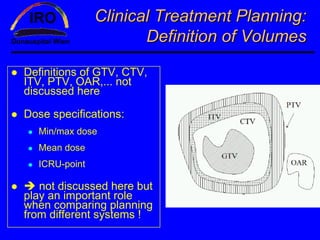
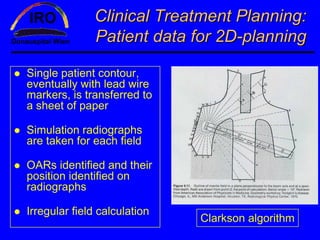
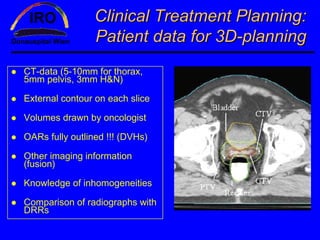
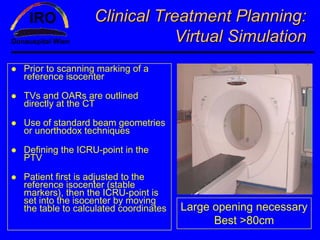
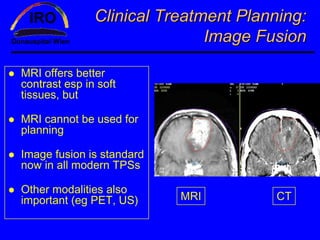
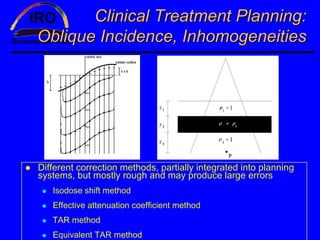
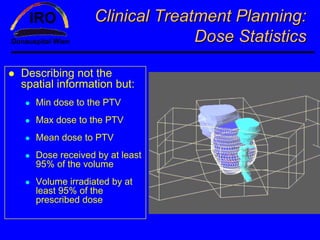
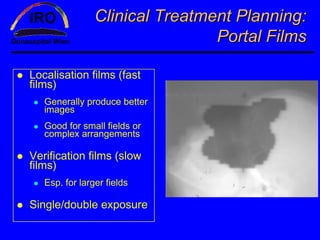
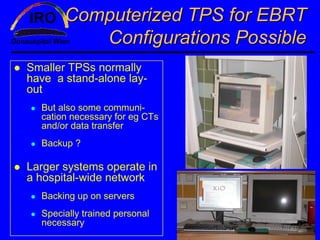
This document provides an overview of planning systems in radiotherapy and discusses various topics related to clinical treatment planning using computerized treatment planning systems. It begins with an introduction to the author and their experience with different treatment planning systems. It then covers definitions and concepts important for clinical treatment planning such as volumes, dose specifications, patient data acquisition, beam combinations, and dose statistics. The document also discusses virtual simulation, image fusion, treatment aids, oblique incidence corrections, and portal imaging. It provides details on the hardware, calculations algorithms, and commissioning of computerized treatment planning systems. In summary, the document offers a comprehensive review of clinical treatment planning processes and considerations for computerized treatment planning systems.