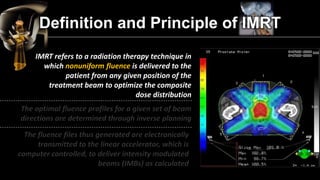
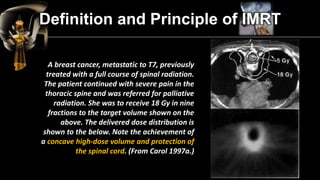
The document discusses intensity modulated radiation therapy (IMRT) and its advantages over conventional radiotherapy. It describes how IMRT uses non-uniform beam intensities to optimize dose distribution and improve tumor targeting while sparing nearby healthy tissues. Treatment planning for IMRT involves determining optimal fluence profiles for multiple beams and inverse planning. Key benefits of IMRT include better tissue sparing to reduce side effects and potentially higher doses to more effectively treat tumors.