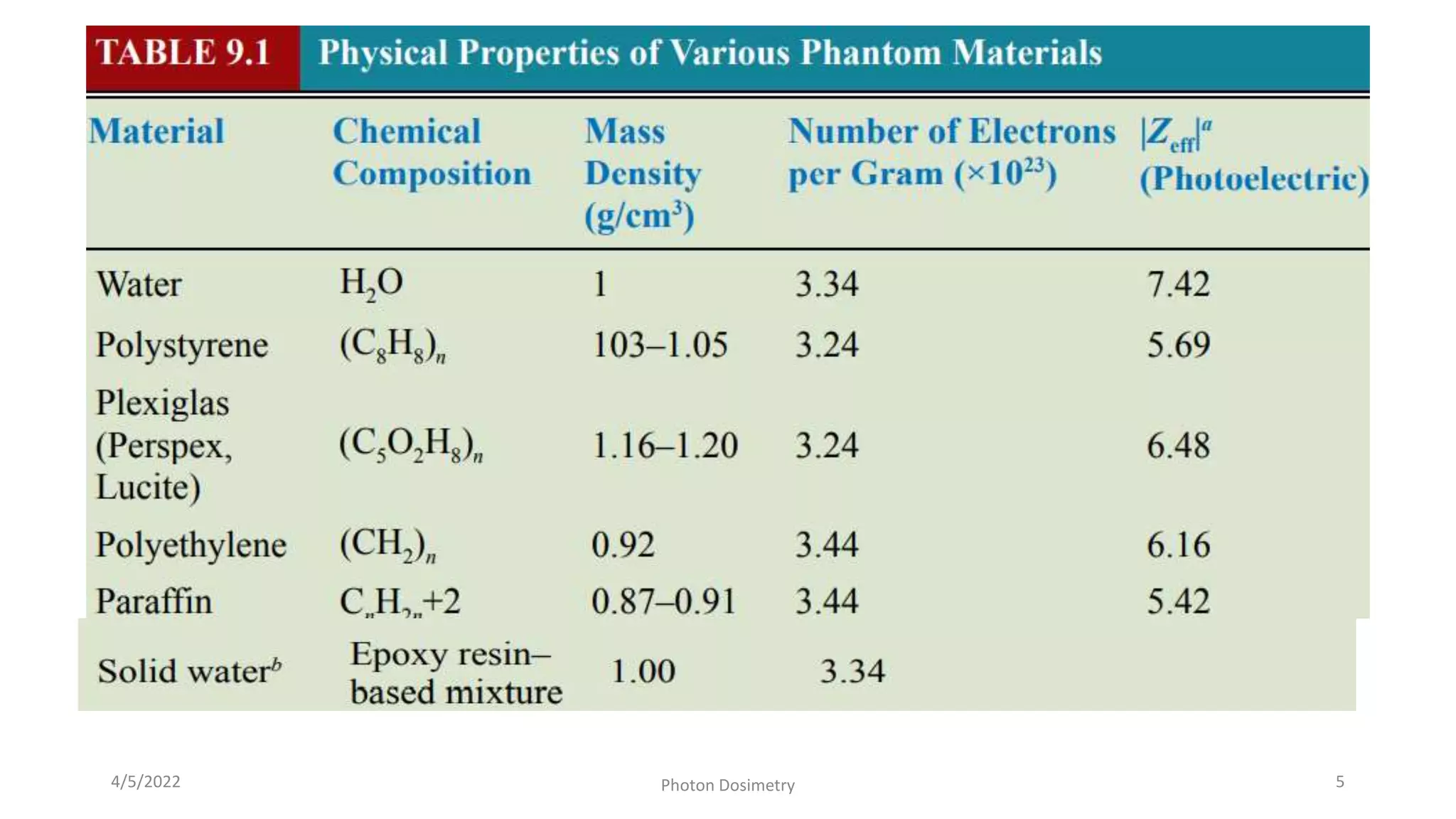
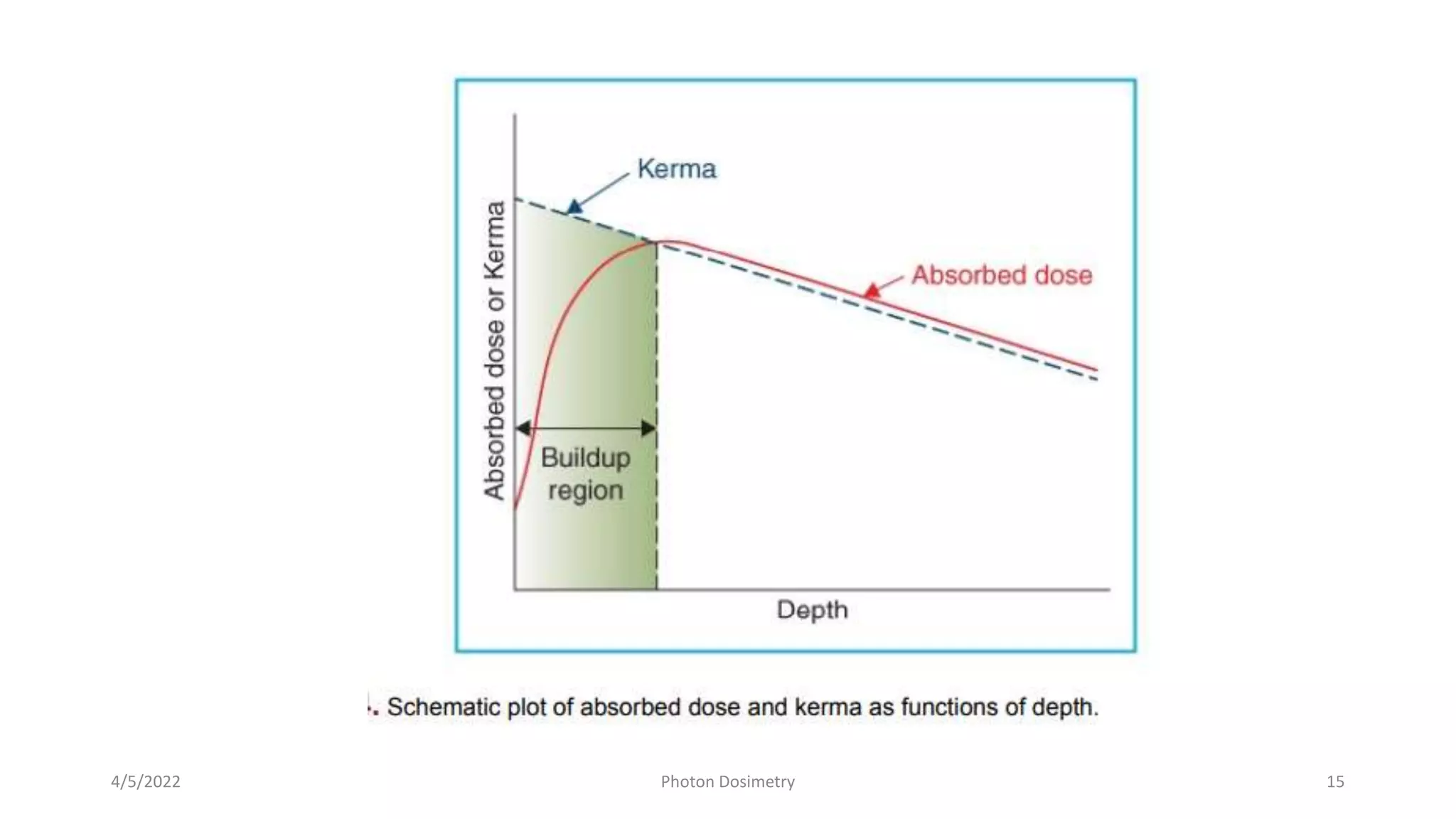
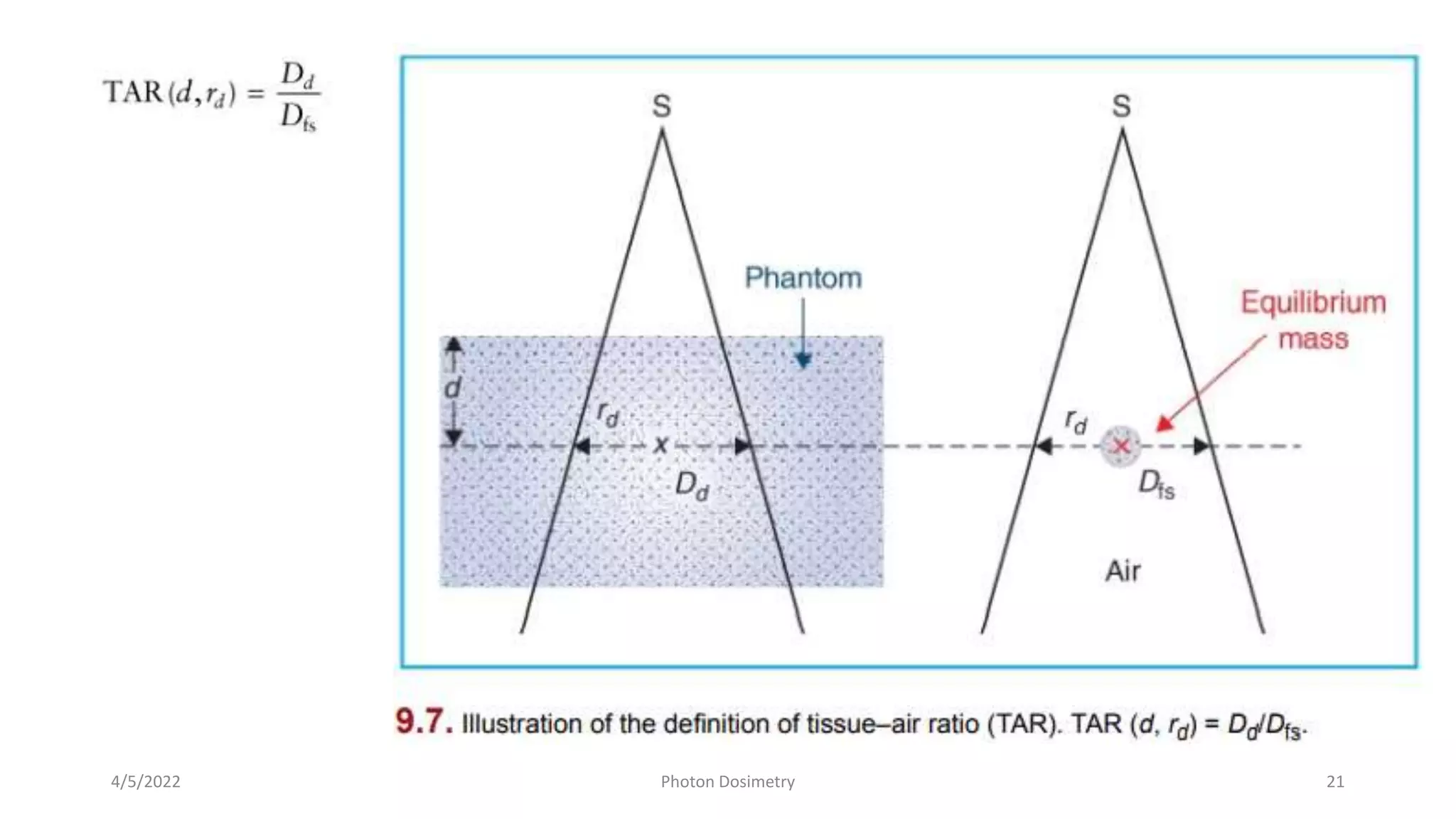
This document discusses various photon beam dosimetry concepts and quantities used in radiation therapy treatment planning. It begins with an introduction to how dose is measured in phantoms rather than patients. Percentage depth dose (PDD) curves are defined as the dose at a given depth normalized to a reference depth. PDD depends on factors like beam energy, depth, field size, and source-surface distance. Tissue-air ratios (TARs) relate dose in a phantom to dose in free space and are independent of source-surface distance. Backscatter factors are the TAR measured at the depth of maximum dose. The document provides details on each of these quantities and their measurement and application in treatment planning.