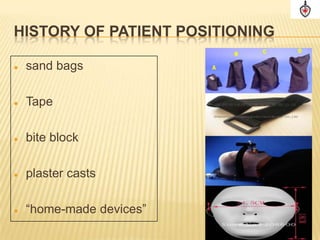
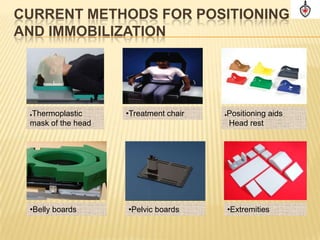
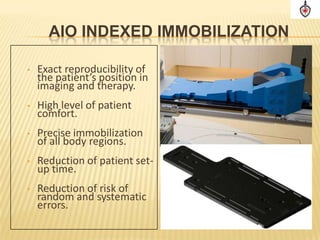
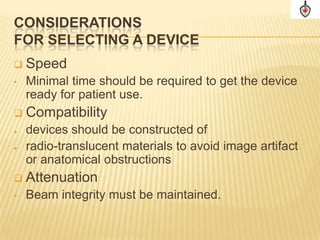
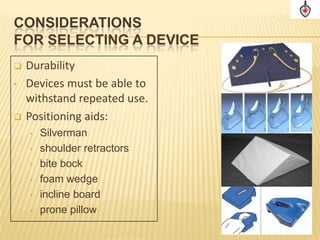
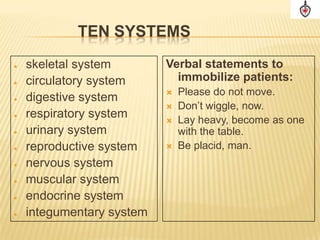
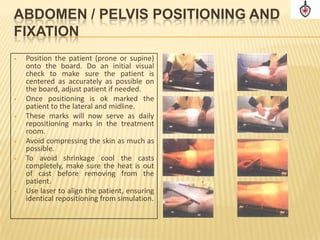
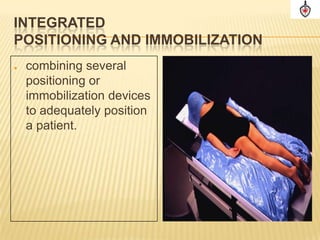
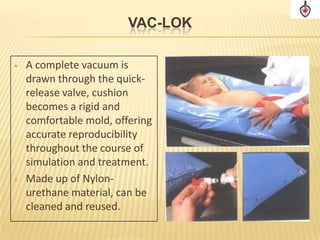
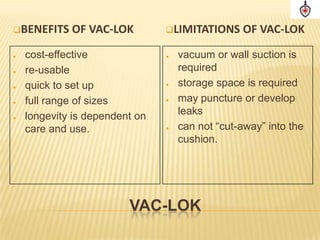
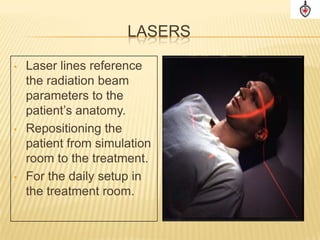
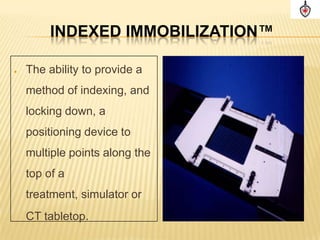
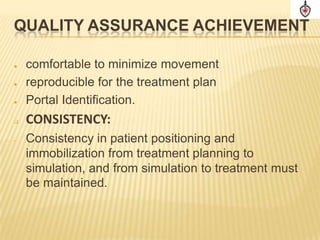
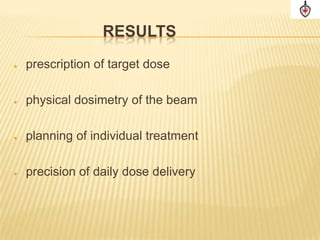
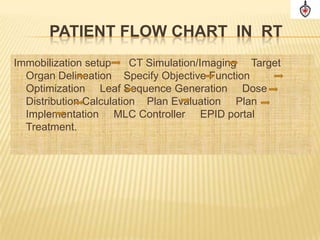
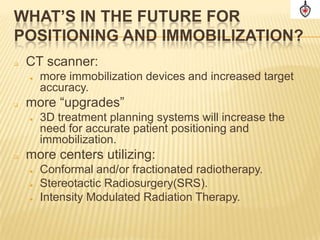
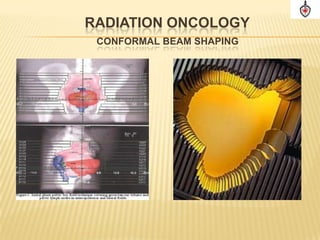
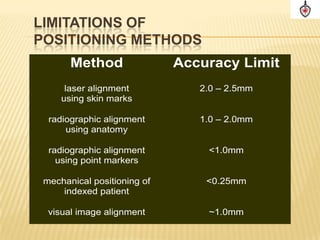
The document discusses quality assurance in patient immobilization and positioning for radiation therapy, outlining various immobilization devices and methods used to precisely position patients to maximize dose to cancerous tissues while sparing normal tissues and ensuring reproducibility from simulation to treatment. It analyzes sources of error in positioning and the benefits of immobilization devices in reducing errors and improving accuracy for conformal radiation therapies.