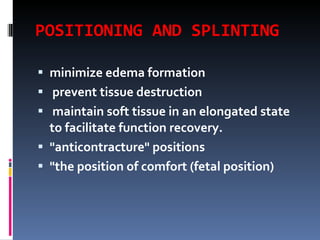
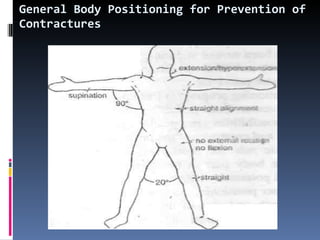
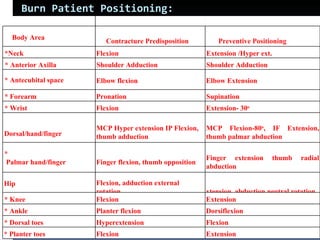
Physiotherapy plays an important role in the management of burn injuries. It focuses on positioning, splinting, and scar management to prevent contractures and promote wound healing. Positioning aims to maintain joints in functional positions opposite to the direction of potential contracture. Splinting is used during the acute inflammatory phase and following skin grafting to maintain positioning. Physiotherapy also addresses scar management through pressure therapy, stretching, and exercises to improve range of motion and function.