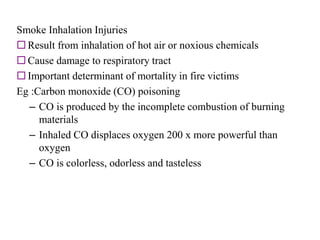
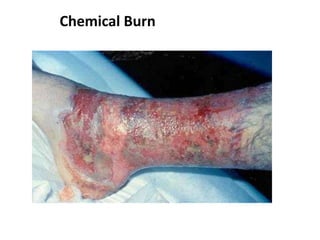
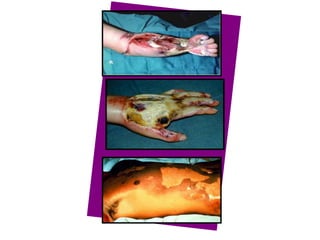
1. A burn is an injury to the skin or flesh caused by heat, electricity, chemicals, friction or radiation. The severity depends on the temperature and duration of exposure.
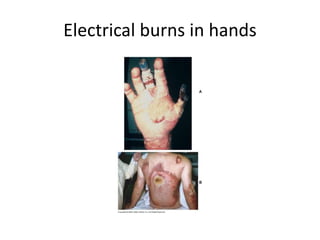
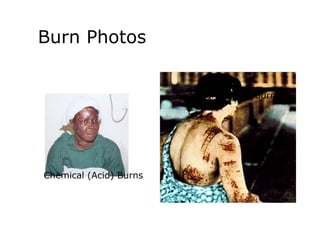
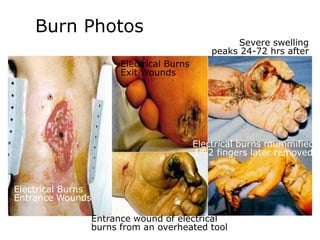
2. About 2.4 million people suffer burns annually in the US, with 700,000 cases requiring medical treatment. The main causes are thermal, electrical, chemical and radiation burns.
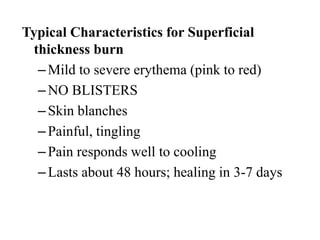
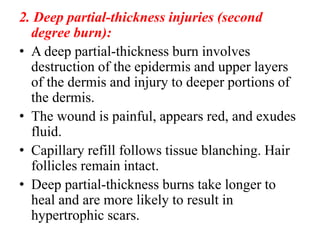
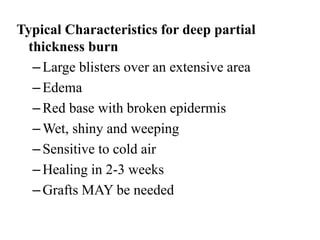
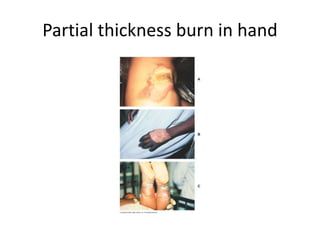
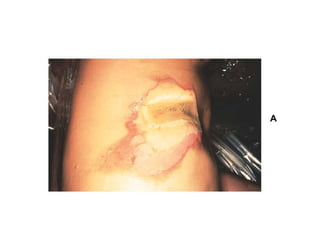
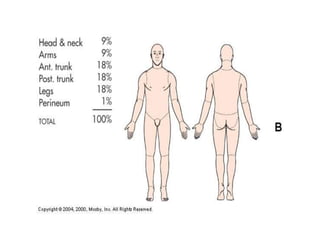
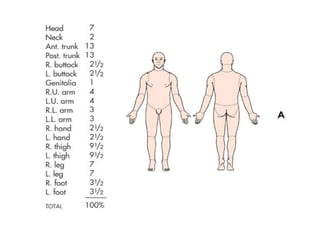
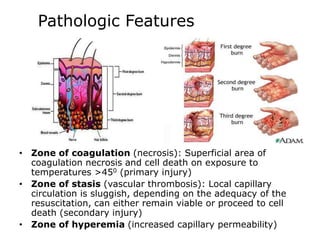
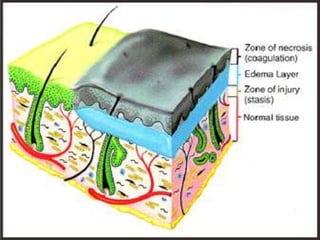
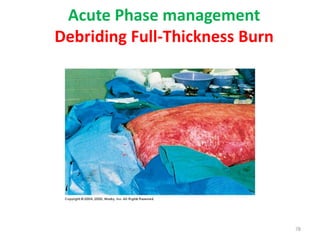
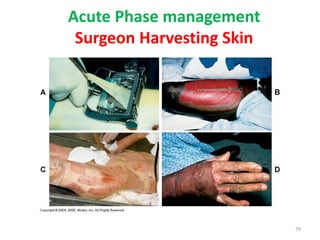
3. Burns are classified by depth and extent of the affected body surface area. Depth is classified as superficial, partial-thickness, or full-thickness. Extent is classified using methods like the Rule of Nines or Lund and Browder chart.