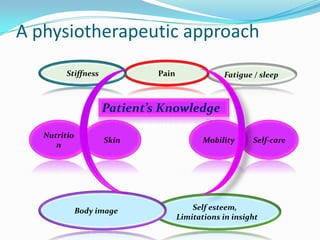
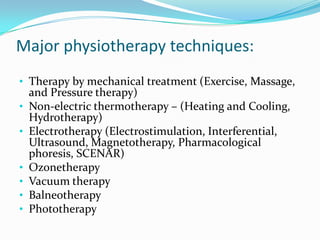
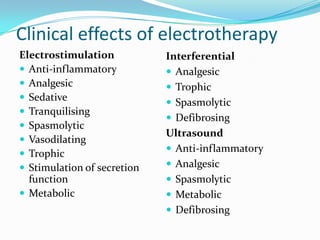
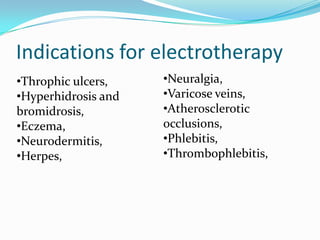
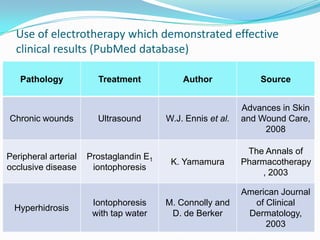
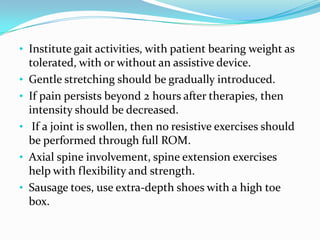
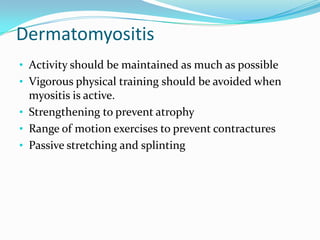
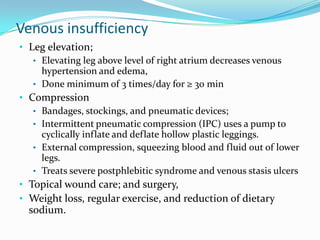
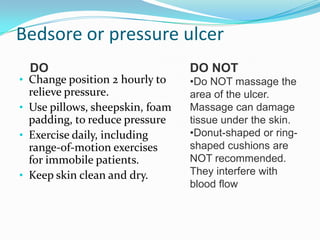
Physiotherapy aims to preserve, enhance or restore movement and physical function impaired by disability, injury or disease. It utilizes techniques like therapeutic exercises, physical modalities, assistive devices and patient education. Physiotherapy can improve function by minimizing contractures, loss of strength and decreased skin compliance, although it may not change underlying pathology or prevent all disability. Major physiotherapy techniques include therapy using mechanical treatment, non-electric thermotherapy, electrotherapy, ozonetherapy, vacuum therapy and balneotherapy. Electrotherapy techniques like electrostimulation, ultrasound and magnetotherapy have anti-inflammatory, analgesic, spasmolytic and trophic clinical effects. Physiotherapy plays an important role in managing various conditions like wounds,