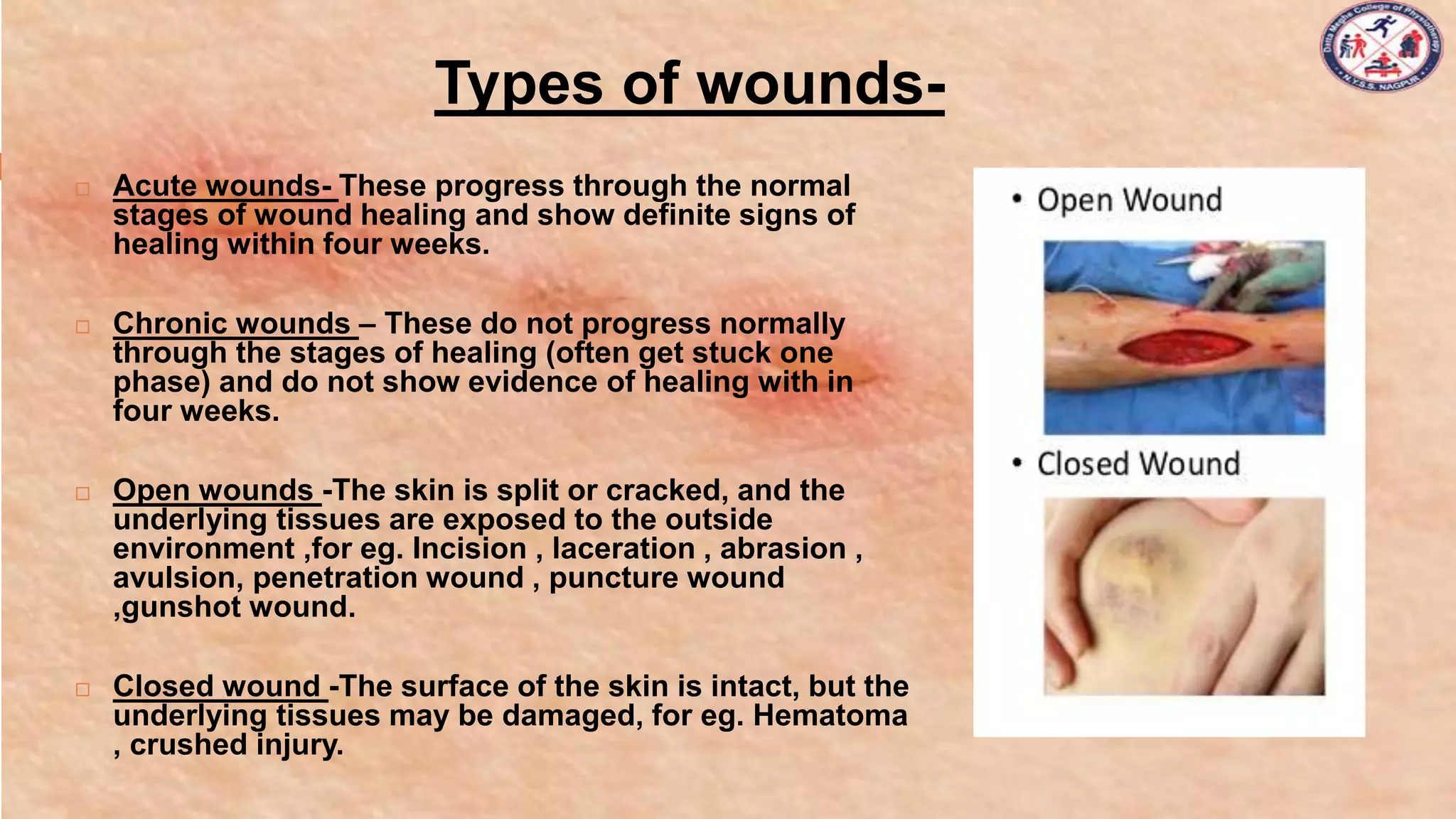
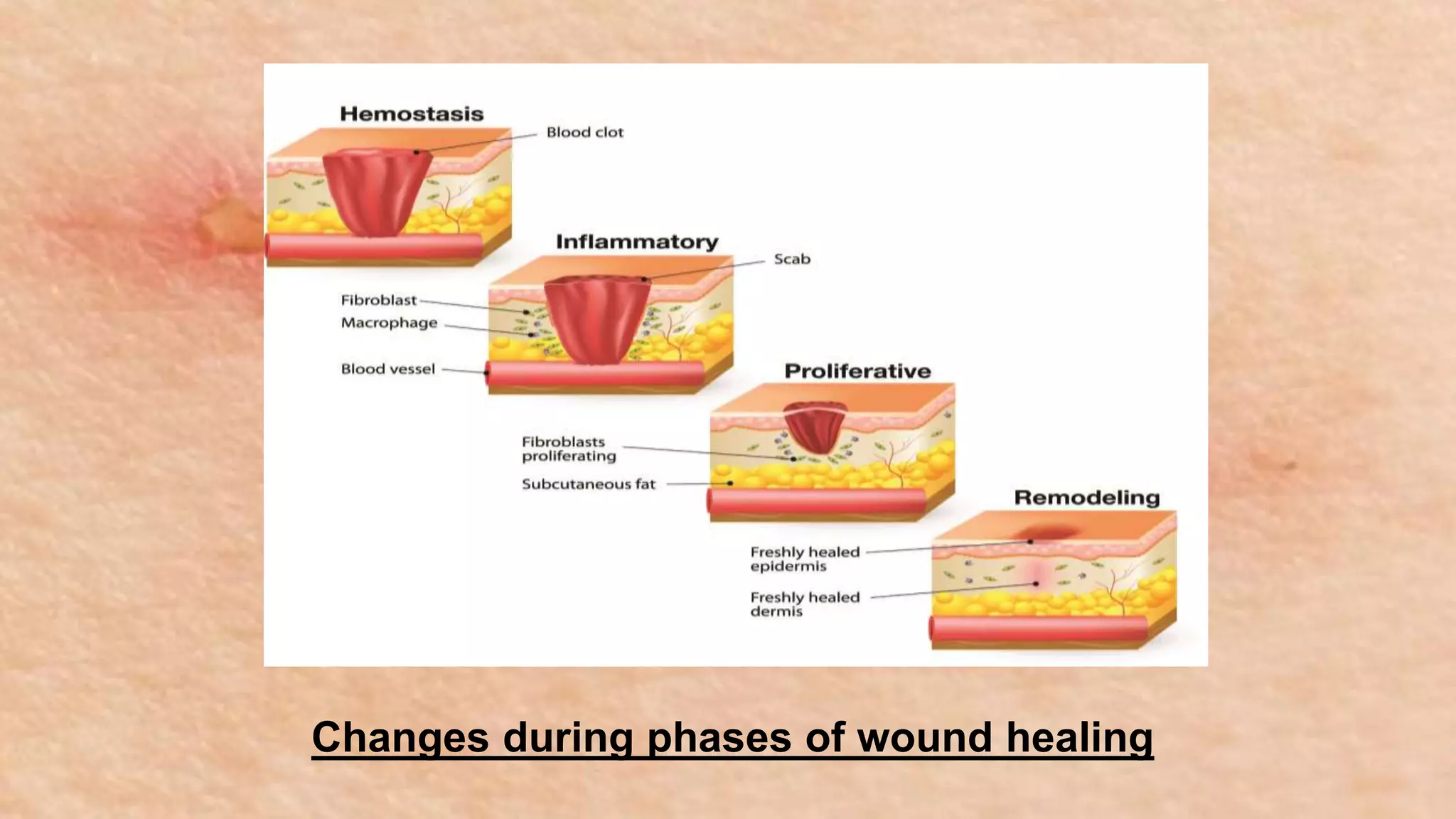
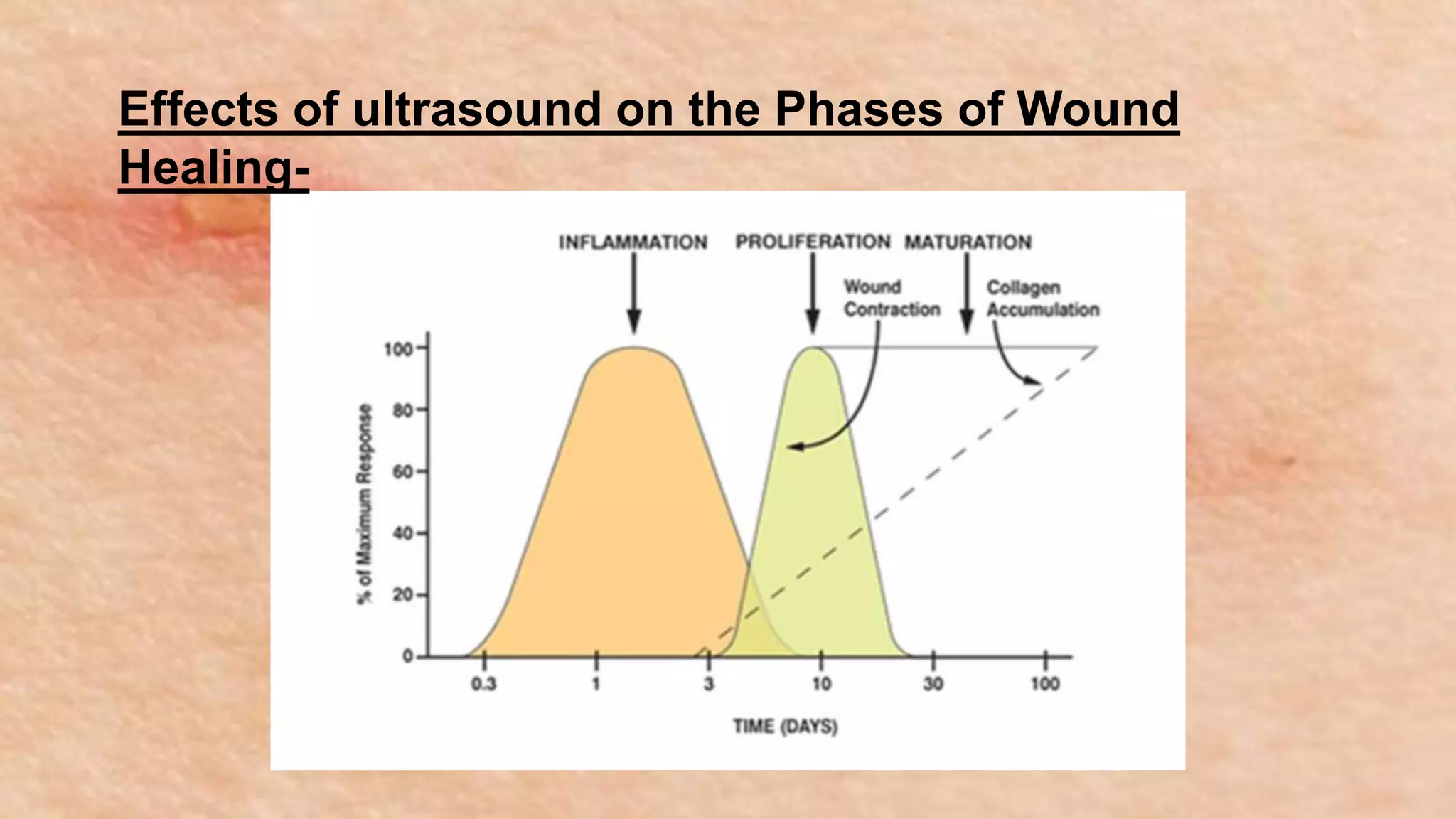
The document discusses wound care and the role of physiotherapy in wound healing. It begins by defining a wound and describing the stages of wound healing: hemostasis, inflammation, proliferation, and maturation. It then discusses types of wounds, factors affecting healing, and complications. The role of physiotherapy includes wound cleaning, debridement, dressing selection and application, education, and use of modalities like ultrasound, ultraviolet light therapy, and low-level laser therapy to accelerate healing. Ultrasound increases circulation and tissue mobility while UV light and laser therapy reduce bacteria and promote cell proliferation and collagen formation. Precautions are described for each modality's application.