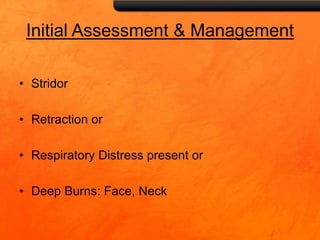
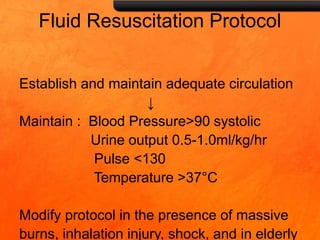
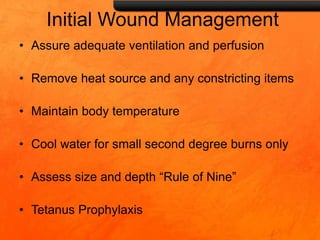
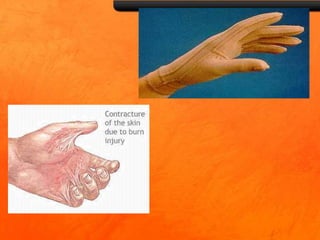
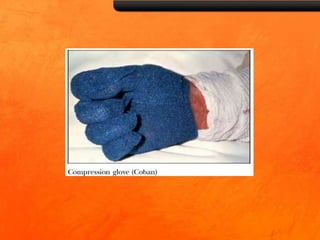
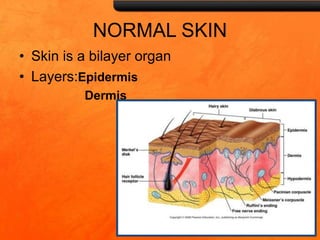
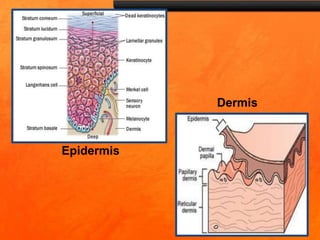
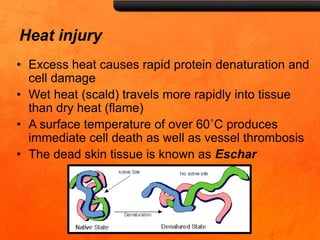
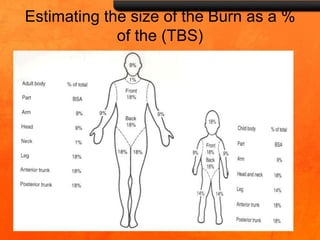
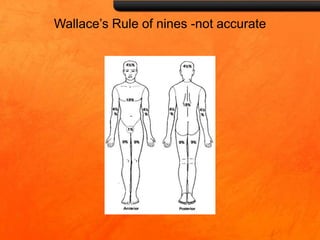
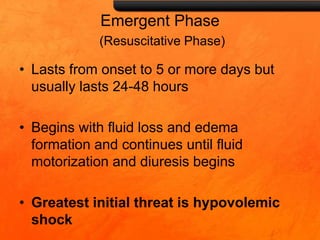
The document outlines a comprehensive overview of burn injuries, including their pathophysiology, classification, and management strategies in physiotherapy. It covers the assessment of burn severity, initial care protocols, and rehabilitation phases while emphasizing the importance of addressing complications and supporting recovery. Key topics include fluid resuscitation, skin grafting, and prevention of scar contractures through various rehabilitative techniques.
![Management
• Anaesthetic consultation
• High flow oxygen
• Tracheobronchial toiletting [ bronchoscopy]
• Physiotherapy
• Close monitoring [preferably ICU ]
• Ventilatory support
• Hemodynamic support, when required](https://image.slidesharecdn.com/burnsmanagement-180412173459/85/Burns-management-18-320.jpg)