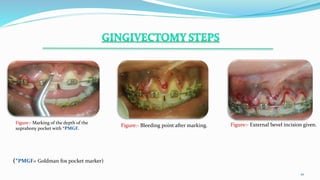
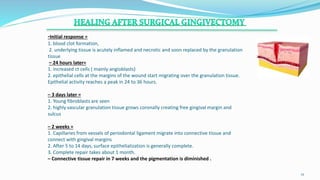
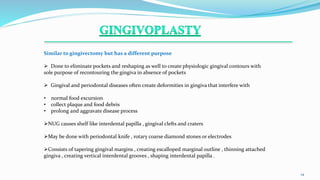
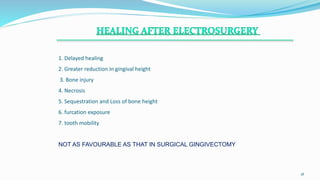
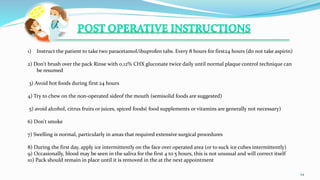
This document discusses different methods of gingivectomy including surgical, electrosurgical, laser, and chemical gingivectomy. It provides definitions and indications for gingivectomy as well as contraindications. The document describes the surgical technique for traditional gingivectomy and postoperative instructions. It compares the healing process and outcomes of different gingivectomy methods and their advantages and disadvantages. Electrosurgery, lasers, and chemosurgery are less favorable than surgical gingivectomy due to greater bone injury, necrosis, and delayed healing.