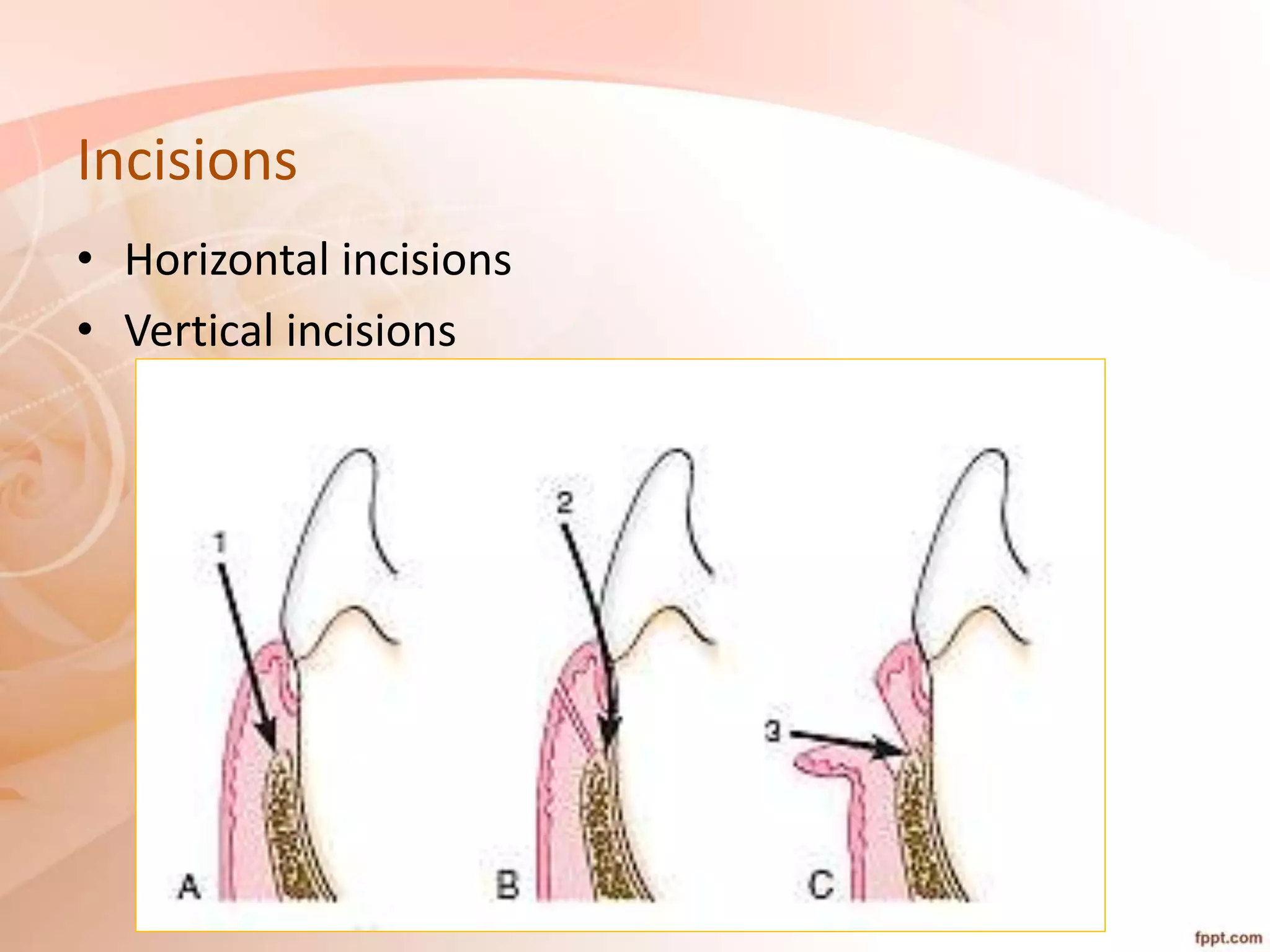
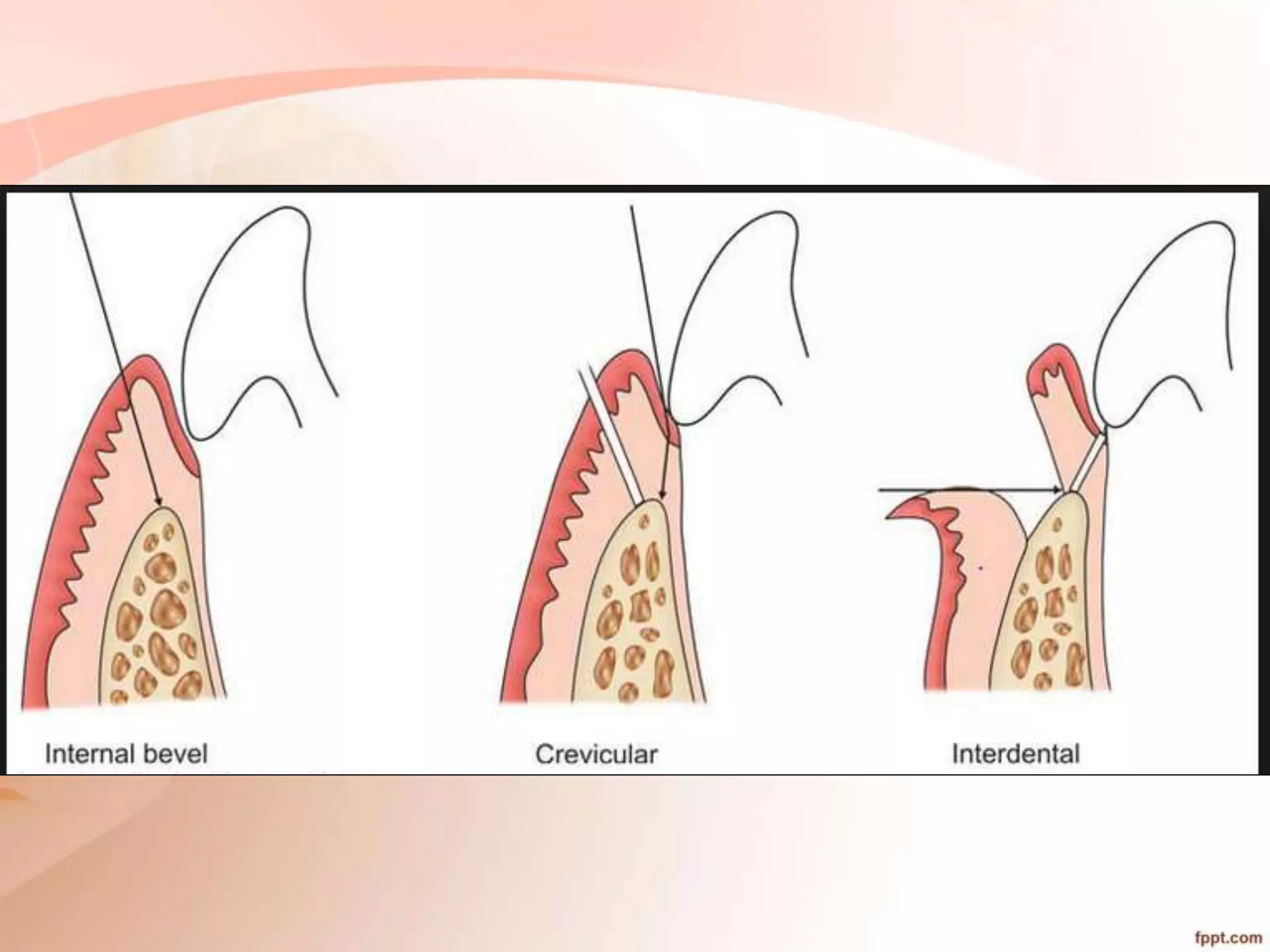
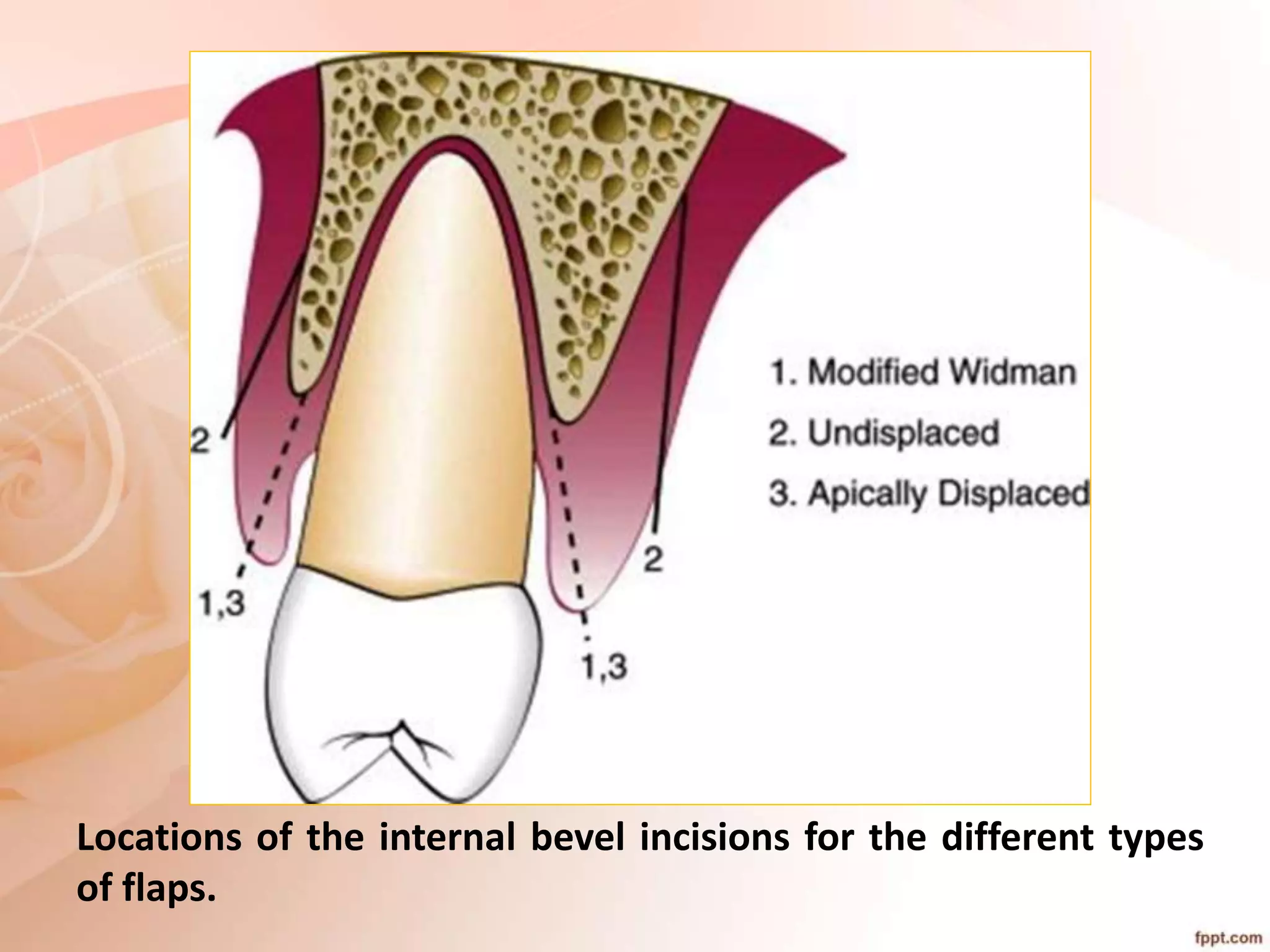
The document discusses the role of periodontal flap surgeries in correcting periodontal pockets. It describes how a periodontal flap provides visibility and access to the bone and root surfaces. The goals of flap surgery are to gain access for root preparation, establish favorable gingival contours, facilitate oral hygiene, lengthen clinical crowns, and promote periodontal regeneration. Indications for flap surgery include deep pockets, furcation involvement, and persistent inflammation. Contraindications include poor health and poor oral hygiene. The document outlines principles of periodontal surgery and details techniques for various flap incisions and designs used to treat different areas.