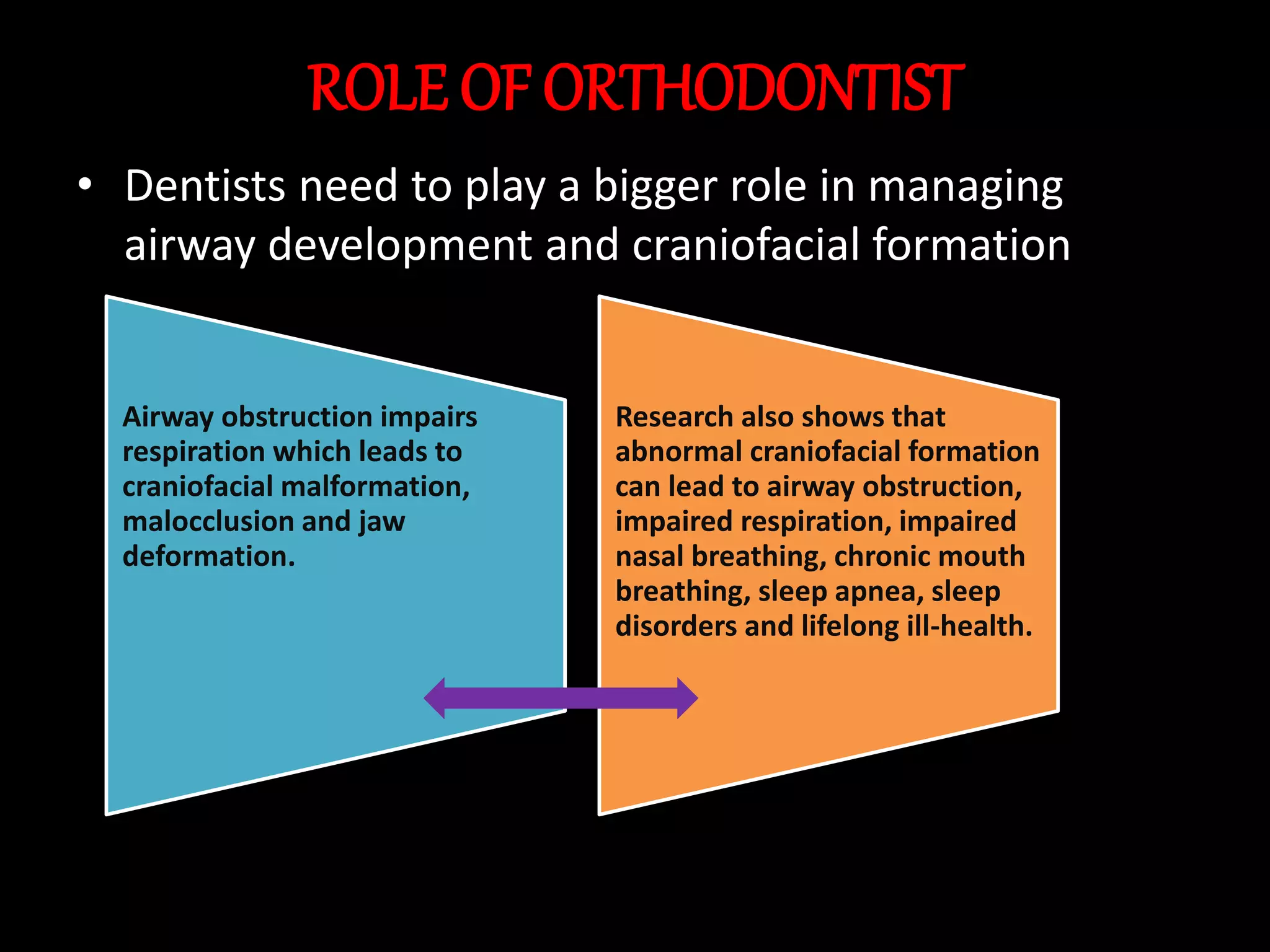
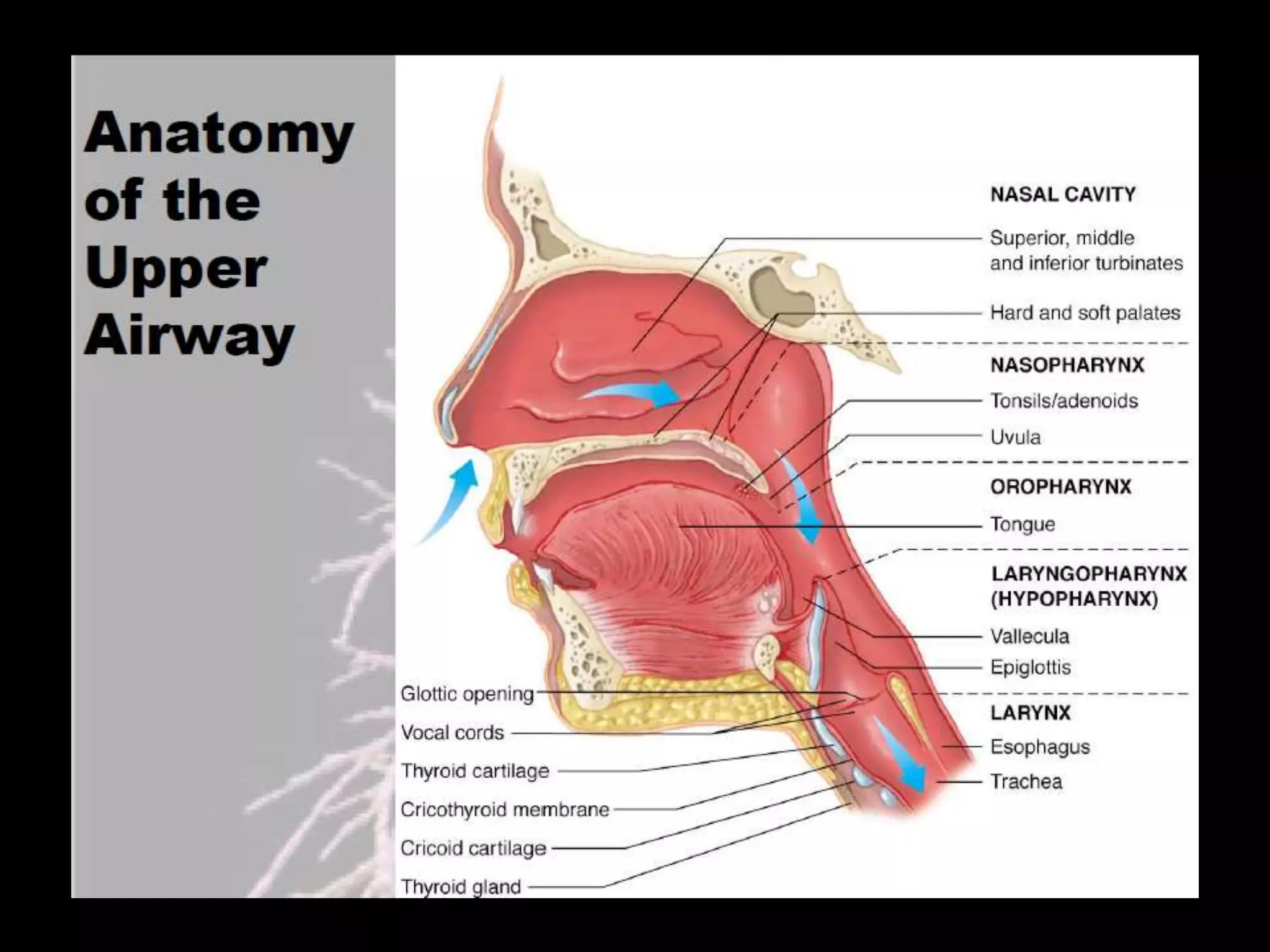
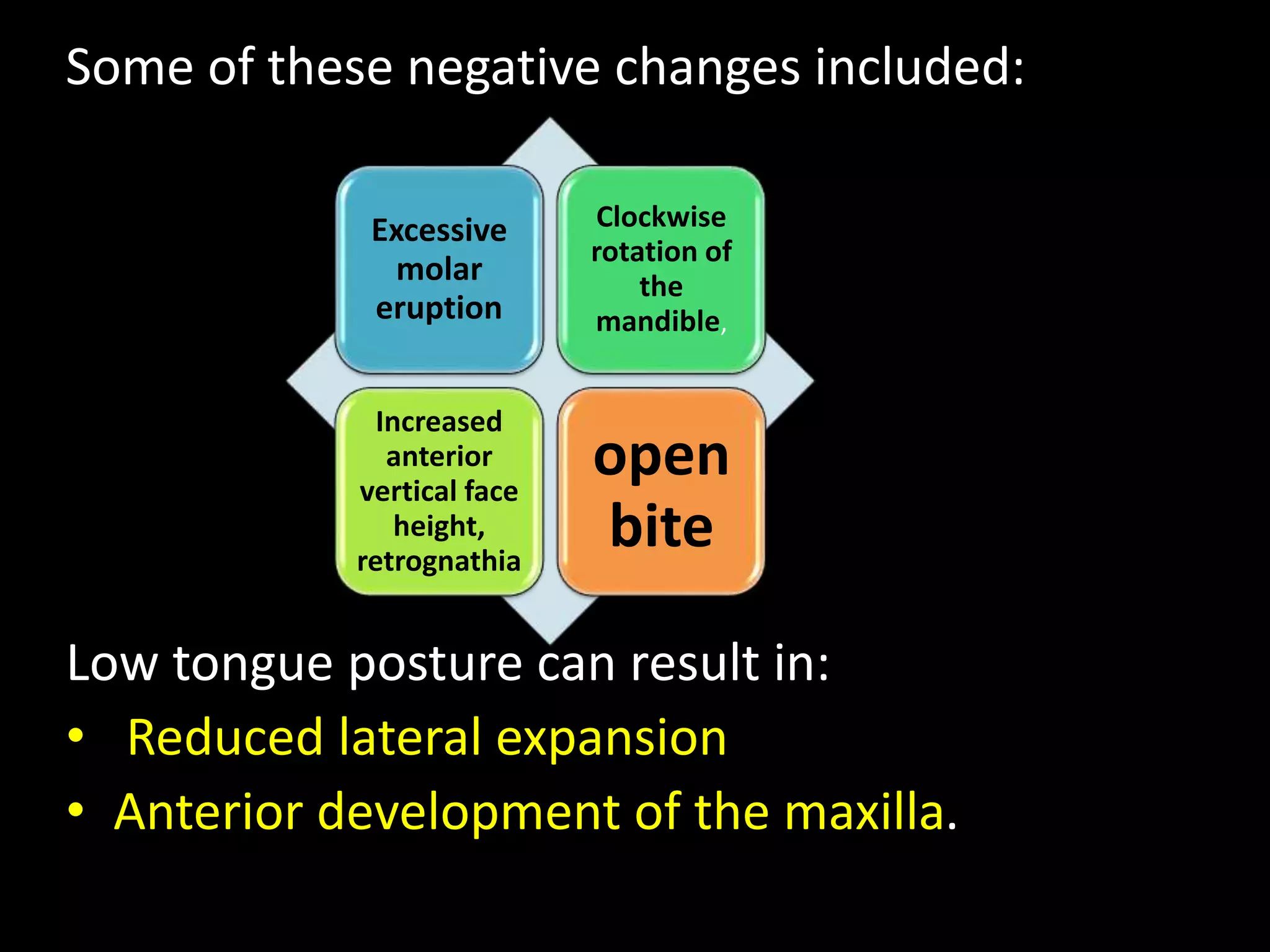
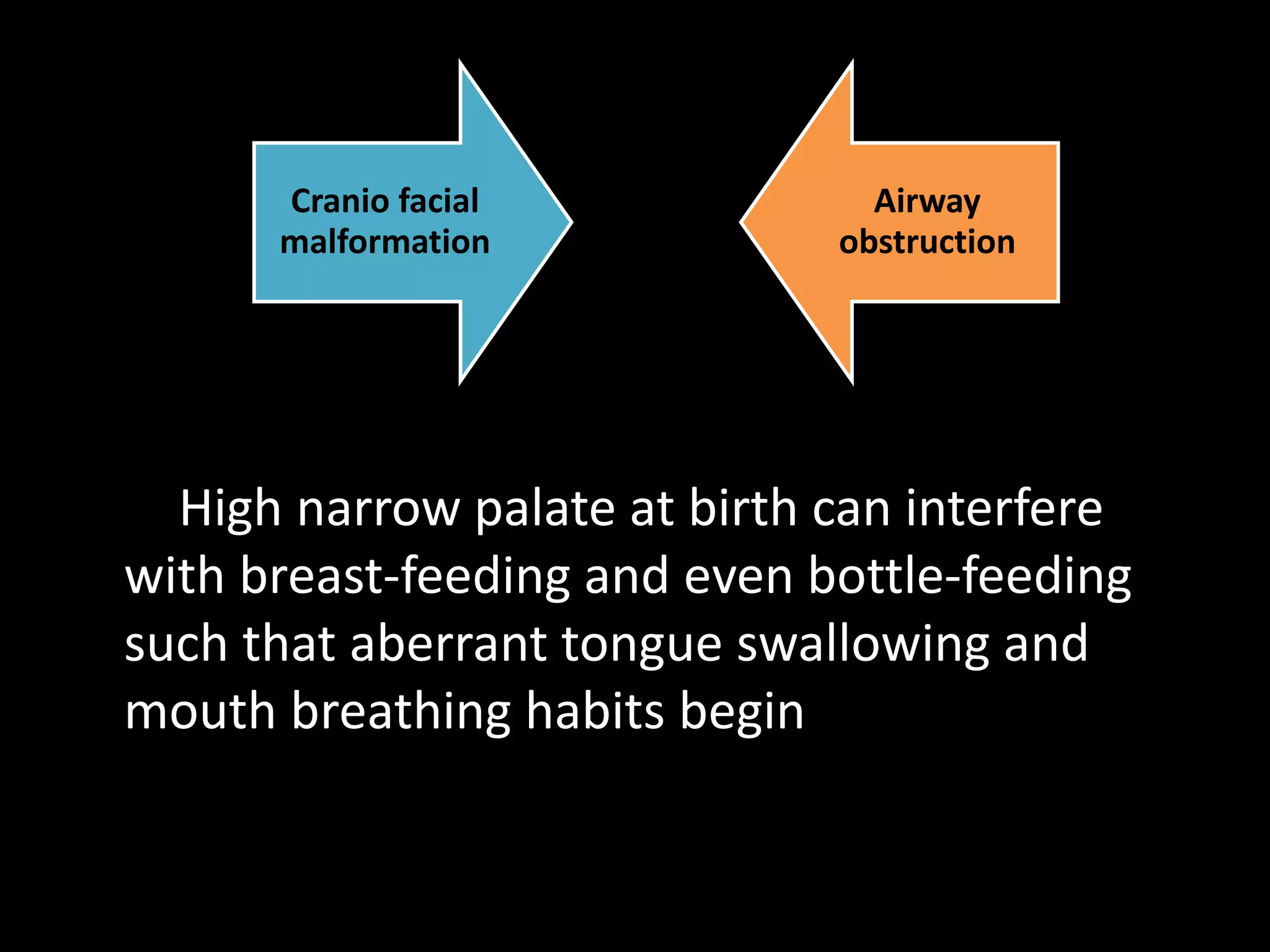
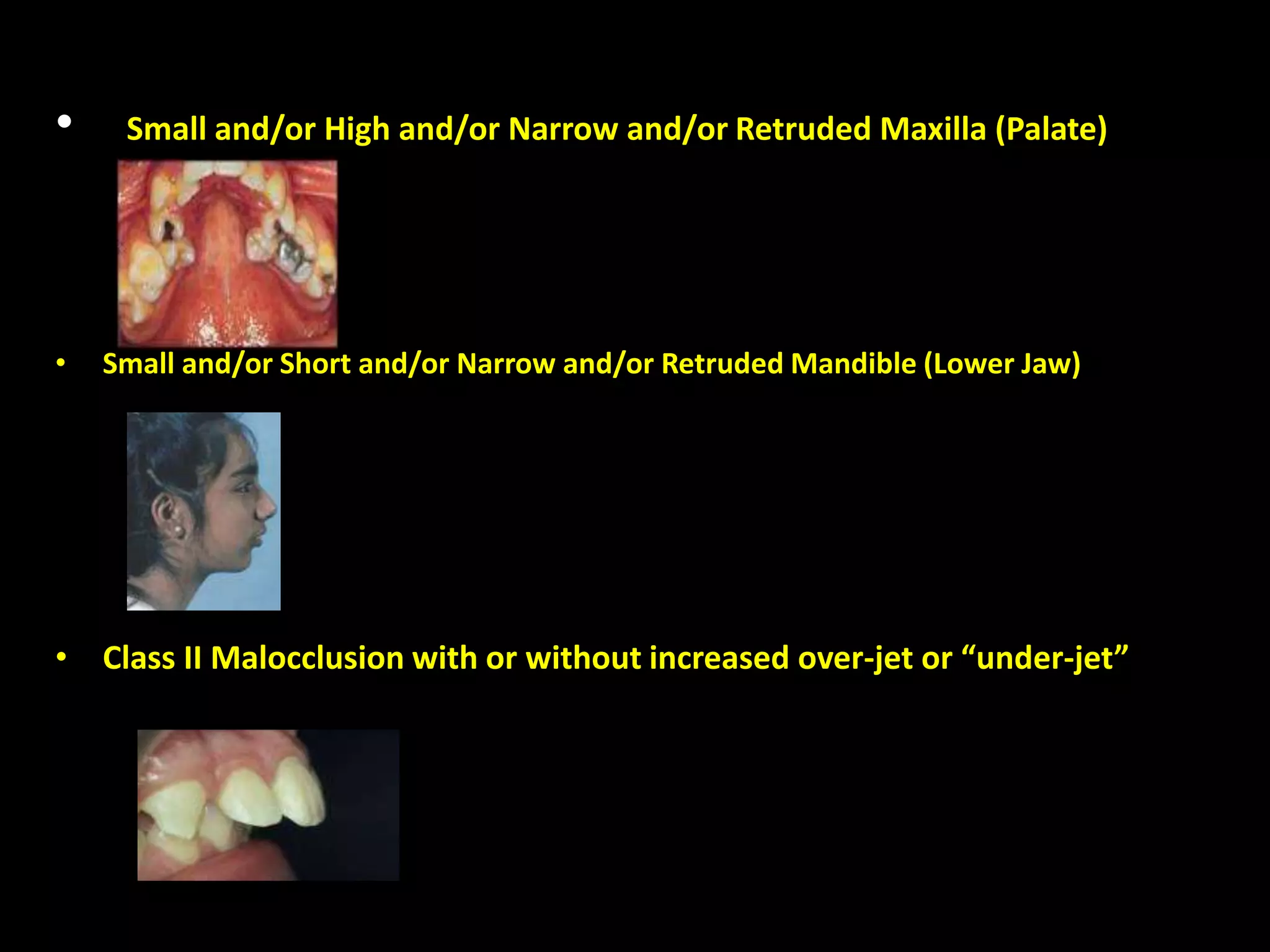
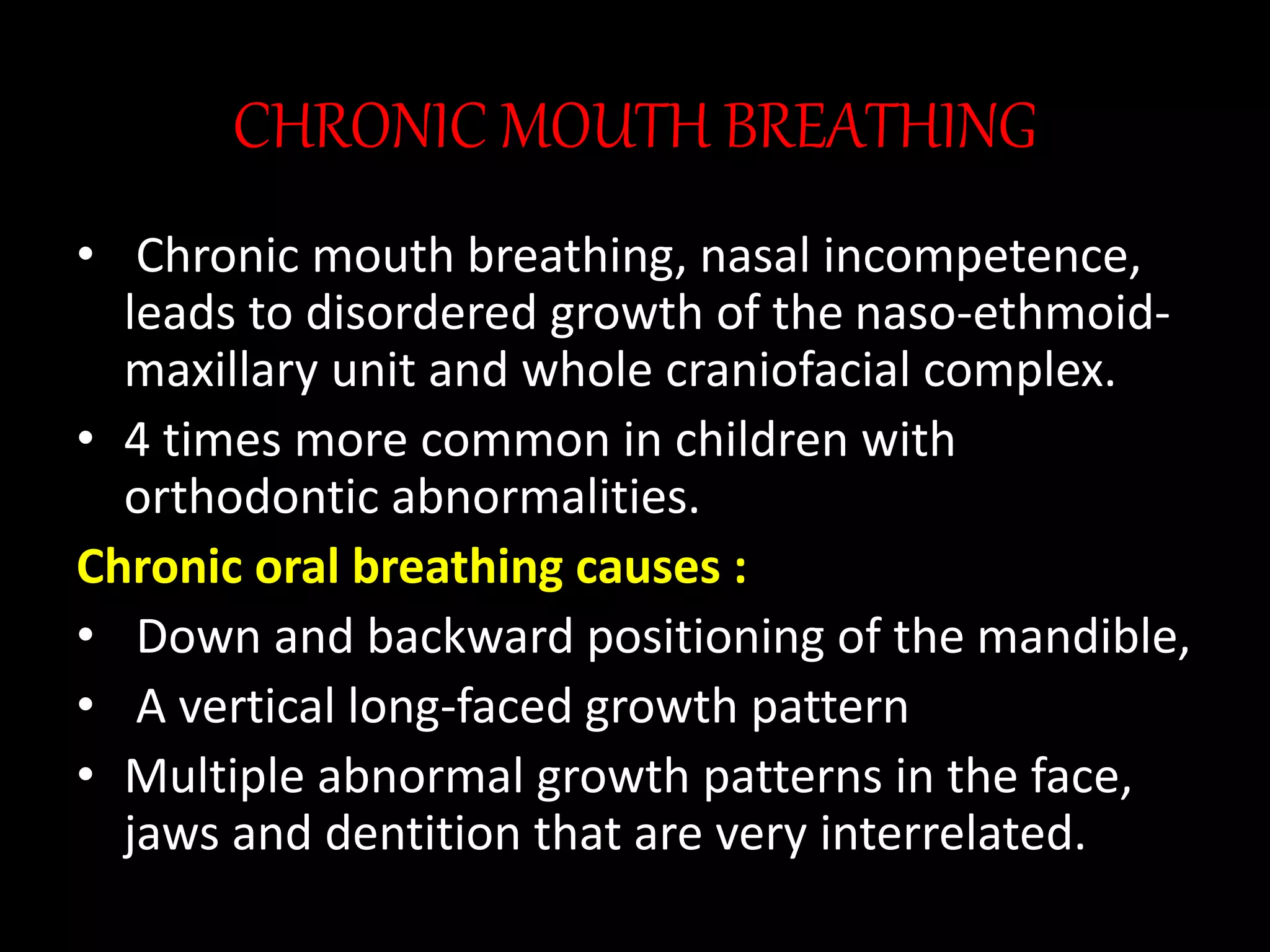
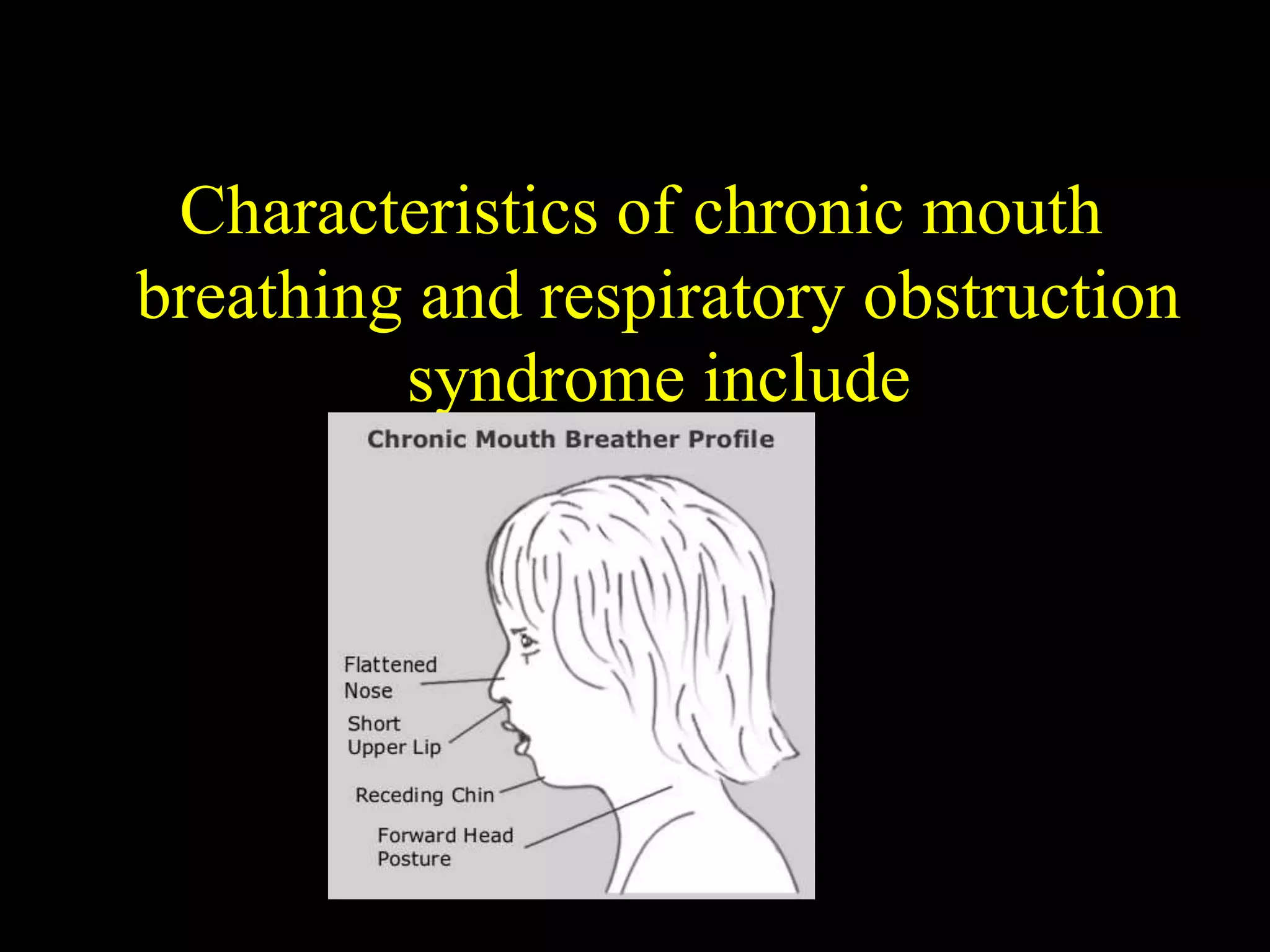
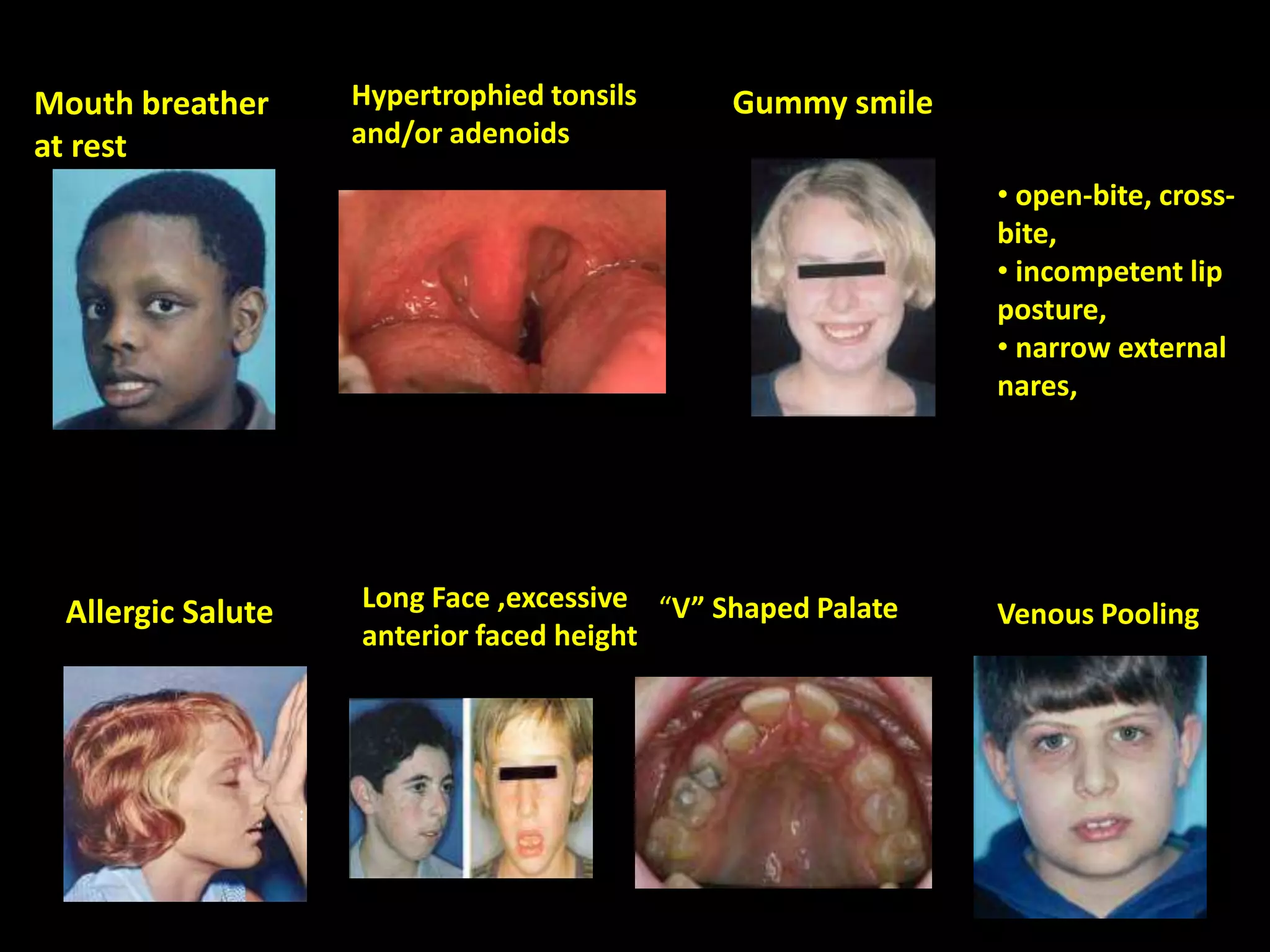
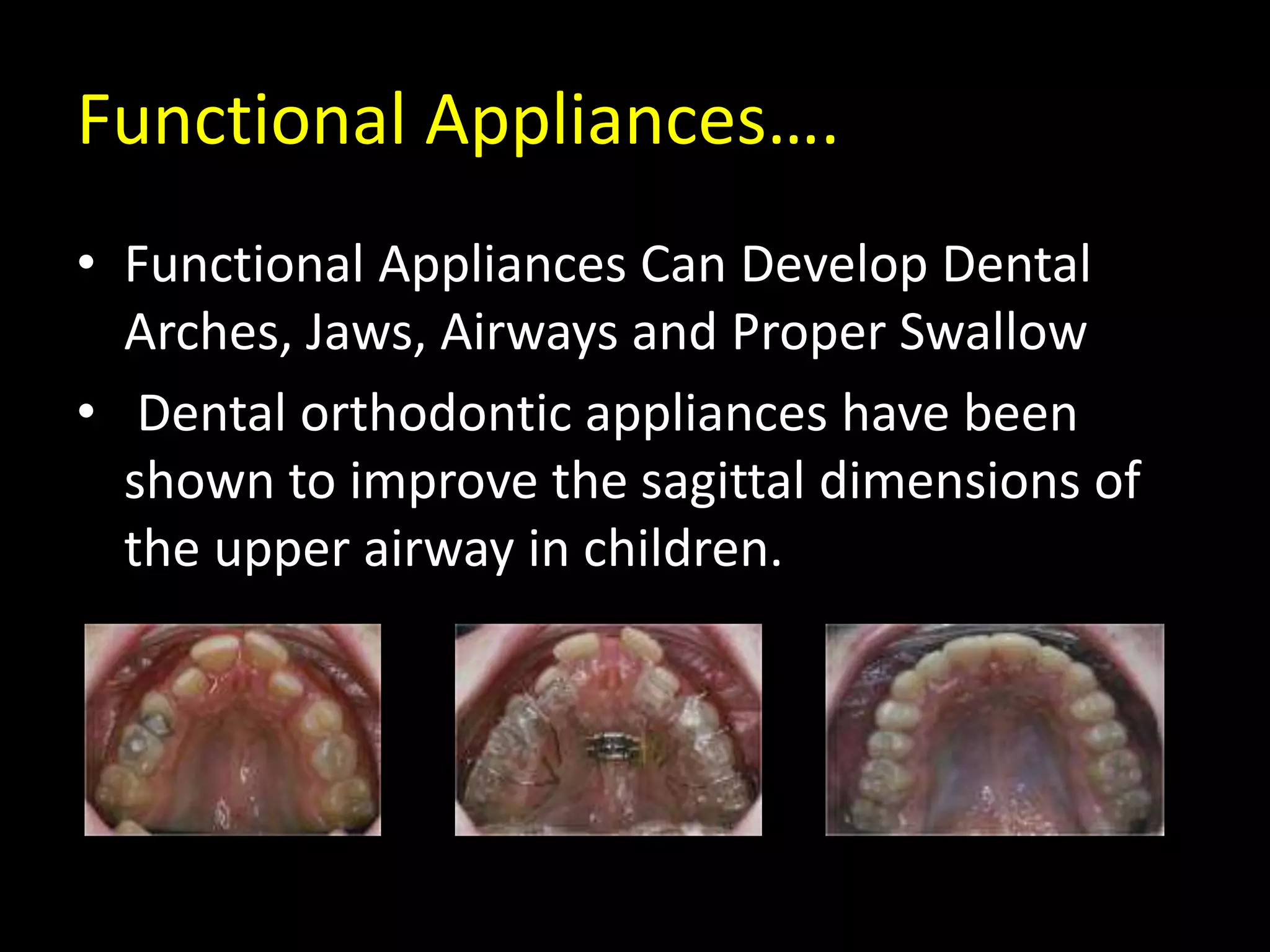
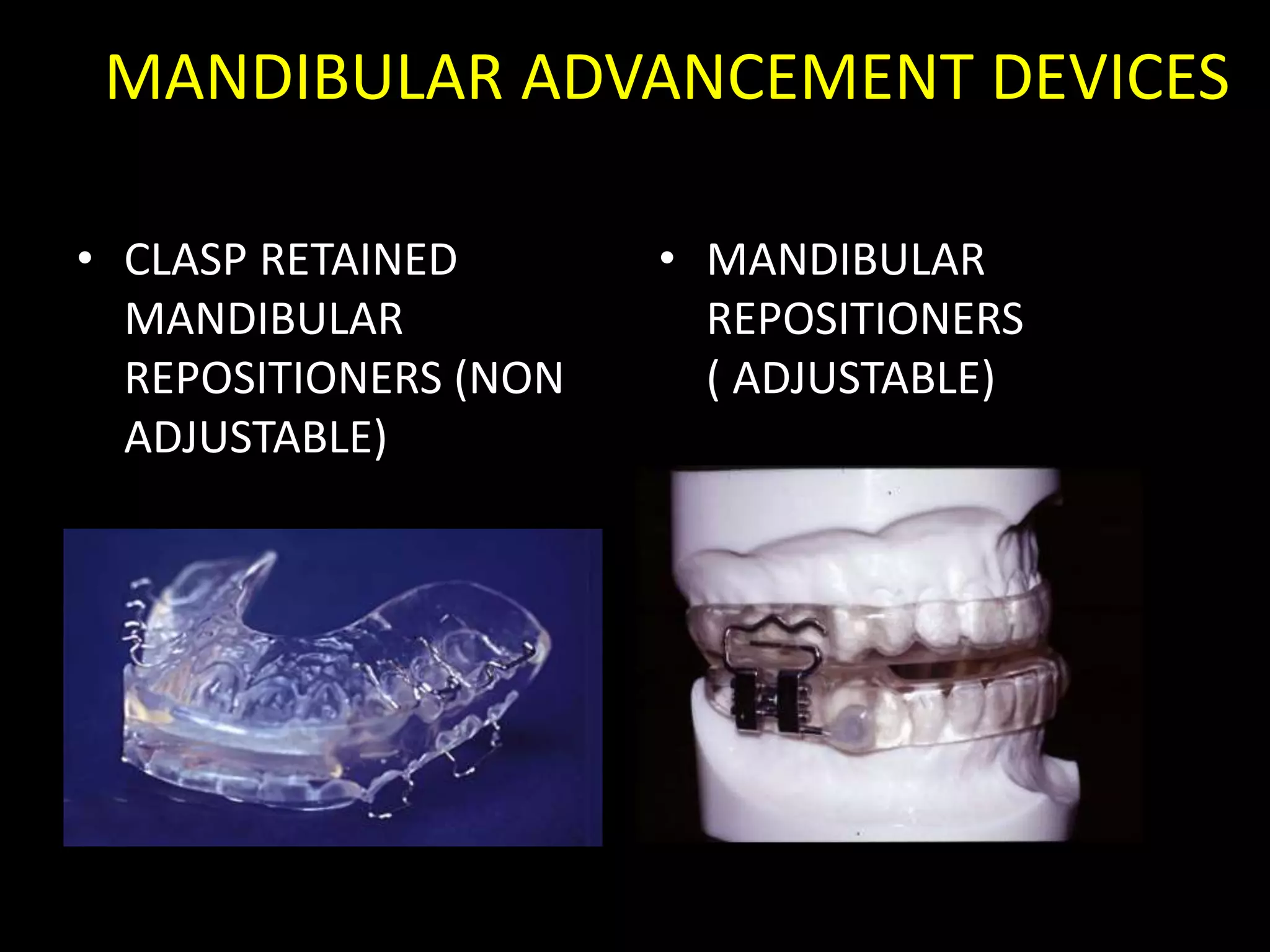
This document discusses the relationship between upper airway, breathing, and craniofacial morphology. It notes that the airway dimensions change with different mandibular positions and that airway, breathing, and craniofacial formation influence each other during development. Early diagnosis and treatment are important to normalize form and function. Dentists and orthodontists need to play a role in managing airway development and craniofacial growth. Conditions like chronic mouth breathing and obstructive sleep apnea can lead to craniofacial malformations and orthodontic issues, so a multidisciplinary approach is needed.