The document discusses Transcatheter Aortic Valve Implantation (TAVI) as a treatment for severe aortic stenosis, particularly in patients with high operative risk or who are not candidates for surgical aortic valve replacement (SAVR). It reviews patient evaluation, procedural techniques, potential complications, and management strategies, as well as ongoing clinical trials assessing TAVI's efficacy in various patient populations. TAVI is recognized as a preferred treatment for high-risk patients while exploring its applications in lower-risk groups.































![BAV
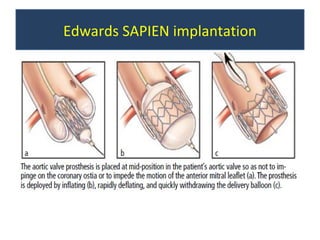
• Balloon aortic valvuloplasty: 20x30
mm (for # 23) or 23x30 mm (for #
26)
• Appropriate angiographic projection
in line with the plane of annulus
[LAO200/Cran200]
• midpoint of balloon at the annular
level PACE INFLATE CHECK
DEFLATE stop pacing](https://image.slidesharecdn.com/tavi-130322204511-phpapp02/85/TAVI-39-320.jpg)






















![Complications & Management
Causes of hypotension after TAVI
••Vascularcomplications—iliac rupture
Vascular complications—iliac rupture
••Ventricularrupture
Ventricular rupture
••Acutevalve dysfunction
Acute valve dysfunction
••Coronaryartery obstruction
Coronary artery obstruction
••Multiplerapid pacing episodes in pts with poor LV function
Multiple rapid pacing episodes in pts with poor LV function
••‘Suicidal’LV in severe LVH [After removing AV obstruction LV
‘Suicidal’ LV in severe LVH [After removing AV obstruction LV
decompresses to such an extent that the subvalvular hypertrophy
decompresses to such an extent that the subvalvular hypertrophy
obstructs outflow] treated with fluids & avoiding diuretics
obstructs outflow] treated with fluids & avoiding diuretics](https://image.slidesharecdn.com/tavi-130322204511-phpapp02/85/TAVI-65-320.jpg)




![Complications & Management
Aortic Regurgitation
••Typicallyparavalvular mild or
Typically paravalvular mild or
mild-moderate severity
mild-moderate severity
••Mostof AR disappears or reduces
Most of AR disappears or reduces
at 11yr follow-up [13% absent, 80%
at yr follow-up [13% absent, 80%
mild AR]
mild AR]](https://image.slidesharecdn.com/tavi-130322204511-phpapp02/85/TAVI-74-320.jpg)







![PARTNER II Trial: Placement of
AoRTic TraNscathetER Valves Trial
Edwards SAPIEN XTTM device and
delivery systems: NovaFlex (transfemoral
access) and Ascendra2 (transapical access) in
patients with symptomatic, calcific, severe
aortic stenosis.
intermediate risk [ STS score of 4-8% ]](https://image.slidesharecdn.com/tavi-130322204511-phpapp02/85/TAVI-88-320.jpg)
![SURTAVI
• Safety and Efficacy Study of the Medtronic
CoreValve® System in the Treatment of
Severe, Symptomatic Aortic Stenosis in
Intermediate Risk Subjects Who Need Aortic
Valve Replacement (SURTAVI).
intermediate risk [ STS score of 3-8% ]](https://image.slidesharecdn.com/tavi-130322204511-phpapp02/85/TAVI-89-320.jpg)