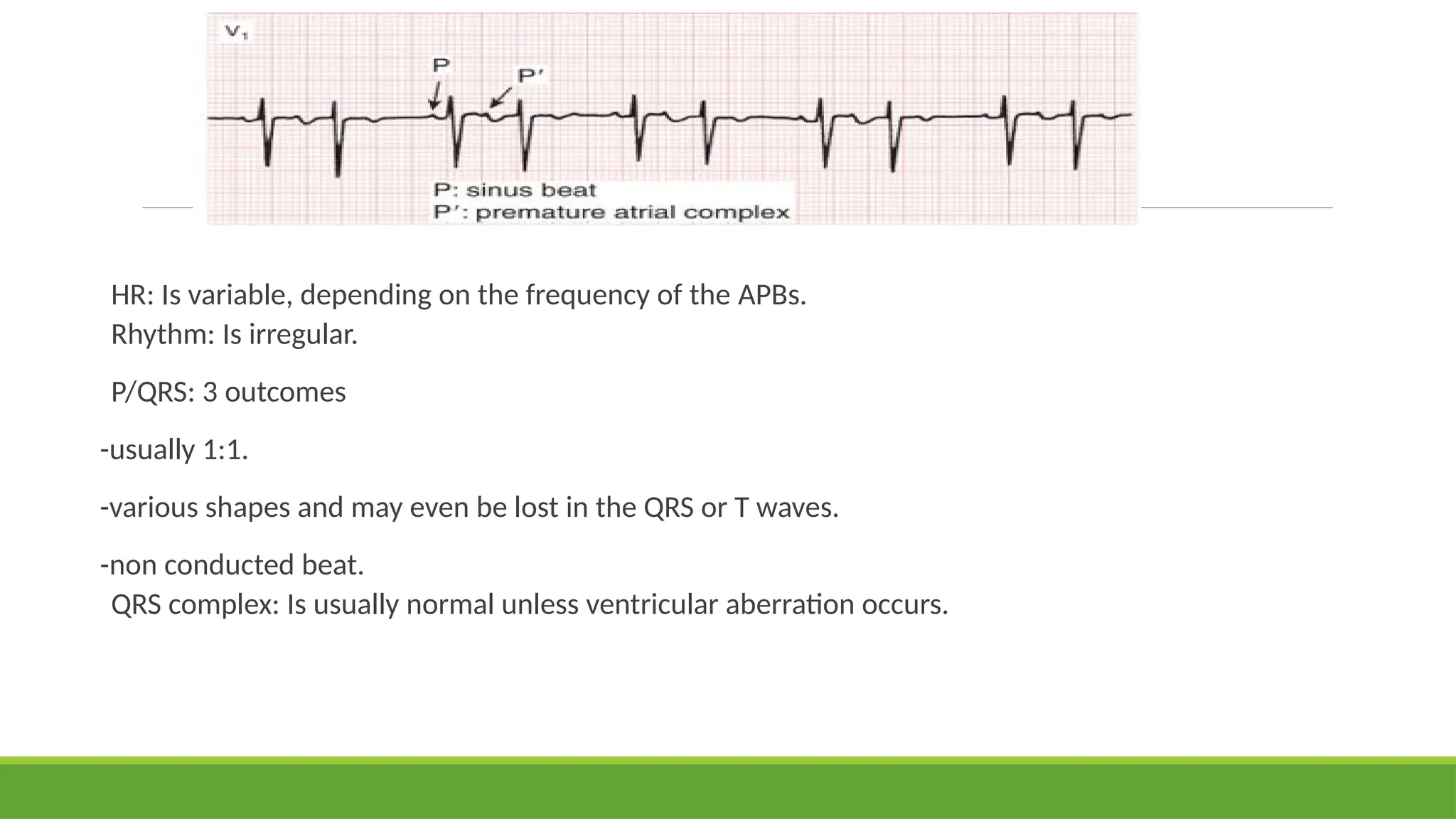
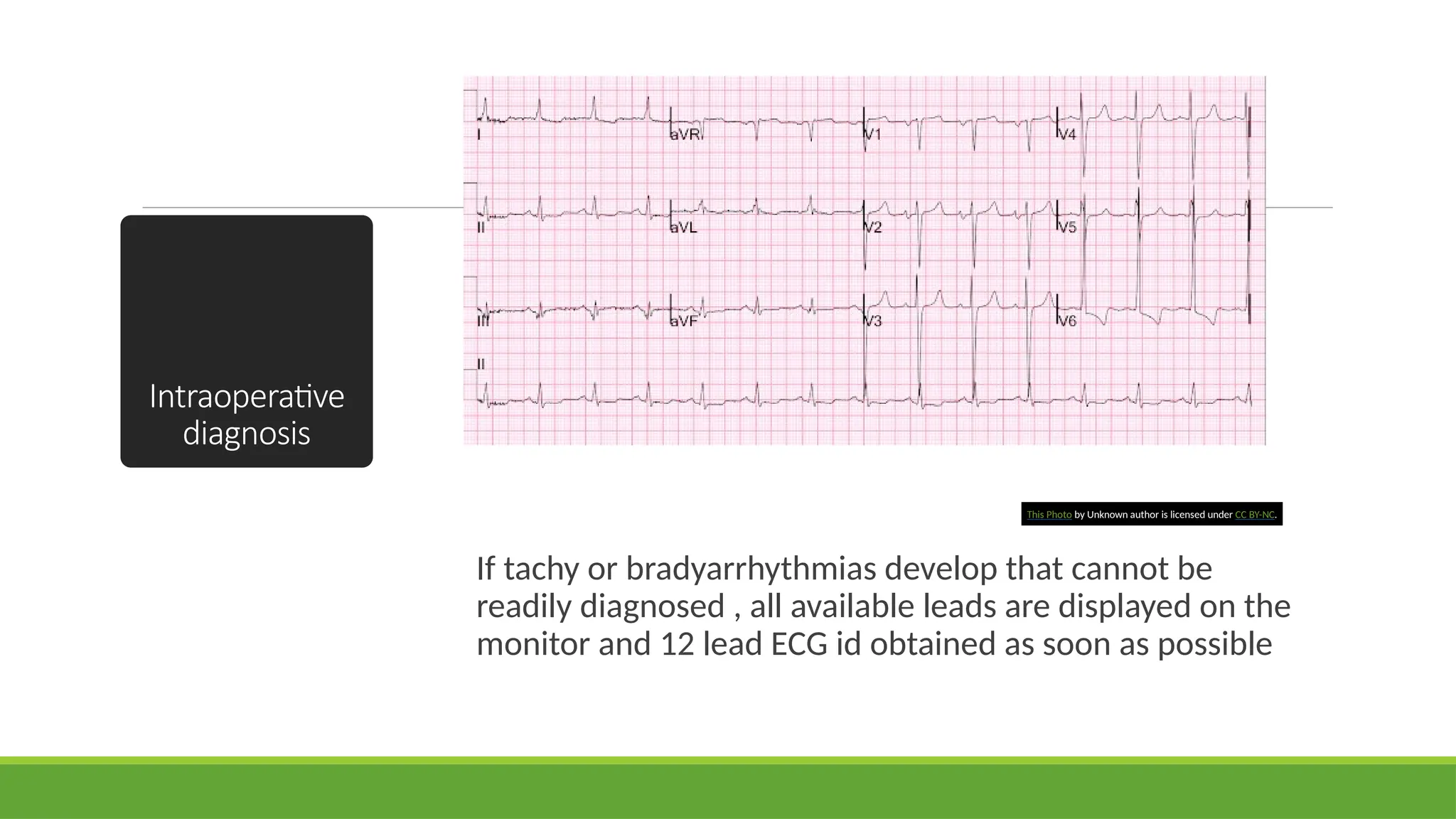
The document discusses perioperative cardiac arrhythmias, including their contributing factors, mechanisms, and management strategies. It covers bradyarrhythmias and tachyarrhythmias, detailing the causes, symptoms, diagnosis methods, and treatments for various types of heart rhythm disturbances. The presentation emphasizes the importance of identifying arrhythmias early and managing them effectively within the perioperative context.


















![Narrow complex tachycardia : QRS < 0.12 sec
Regular (supraventricular tachycardia [SVT])
Sinus tachycardia
Physiological response to insult. Impulse originates from sino-atrial (SA) node.
Atrial tachycardia
Aberrant atrial focus producing impulse independent of SA node
Atrioventricular nodal re-entry tachycardia (AVNRT)
Re-entry circuit within or near AV node
AV re-entry tachycardia (AVRT)
Re-entry circuit conducted from atria to ventricles via abnormal accessory pathway; usually due to
Wolff-Parkinson-White (WPW) syndrome
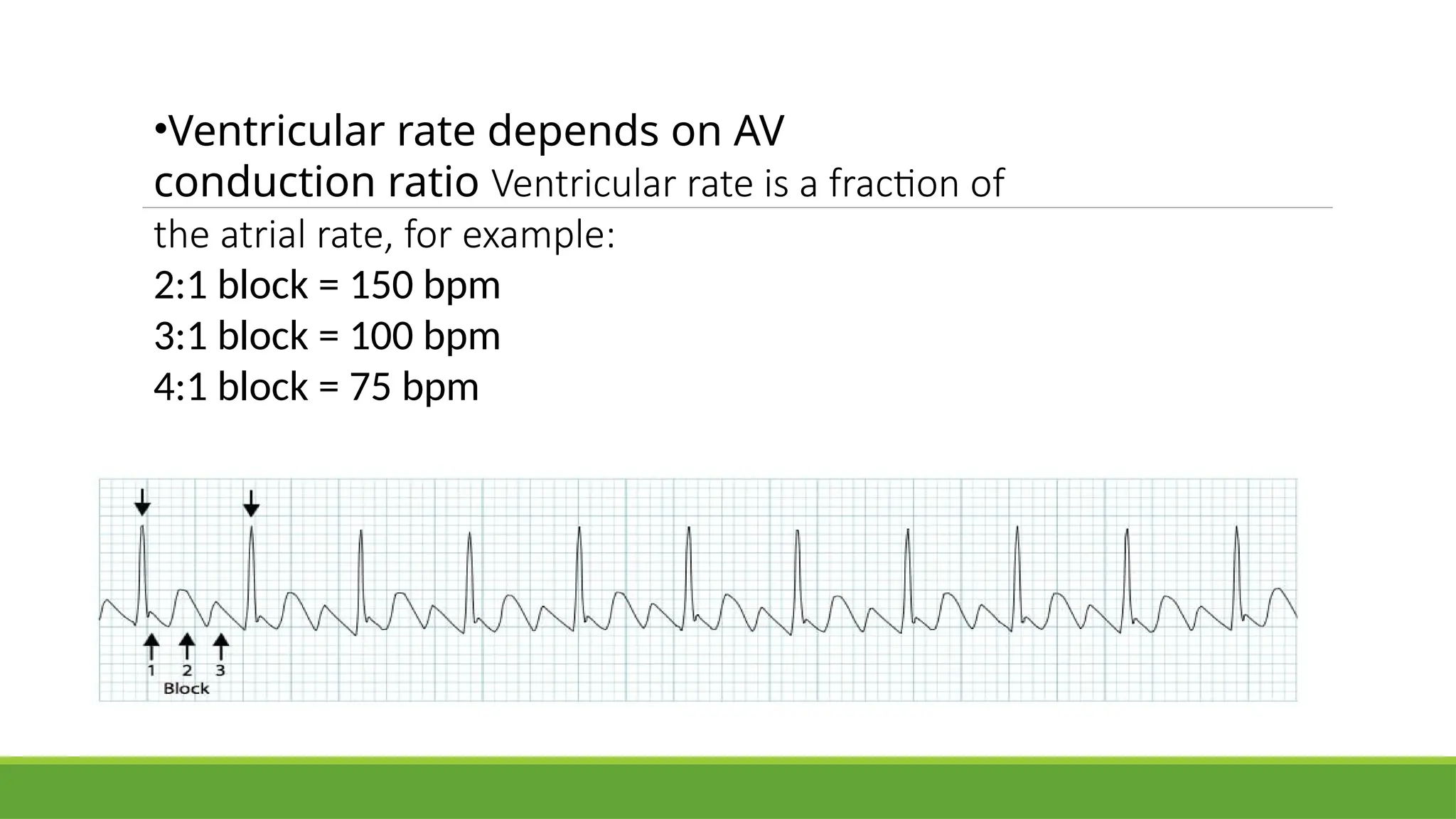
Atrial flutter with regular AV block(e.g., 2:1, 3:1)
Re-entry circuit within the atria
IrregularAtrial fibrillation (AF)
Atria twitch instead of beating in a coordinated manner](https://image.slidesharecdn.com/cardiacarrhythmias21-240812020206-b1ee82ba/75/Arrhythmias-vascular-and-hemorrhage-2-1-pptx-23-2048.jpg)