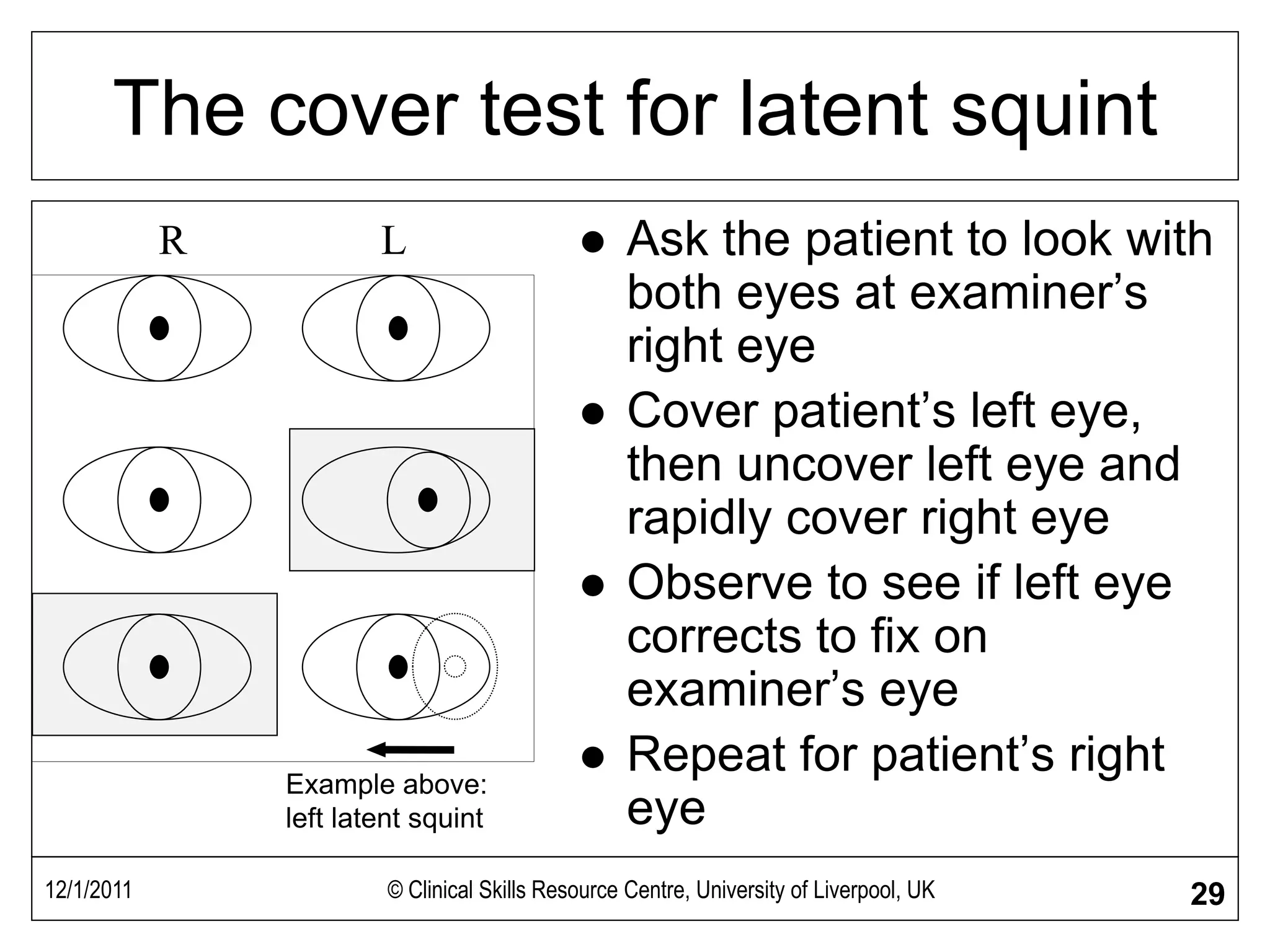
This document provides information on examining the 12 cranial nerves, with a focus on testing the functions of nerves 1-7. It describes how to test smell (cranial nerve 1), visual acuity and fields (cranial nerve 2), eye movements and diplopia (cranial nerves 3, 4, 6), sensation and motor function of the face (cranial nerves 5 and 7). Formal testing of each nerve is outlined, including bedside assessments of smell, vision, eye movements, facial expression, and jaw strength.