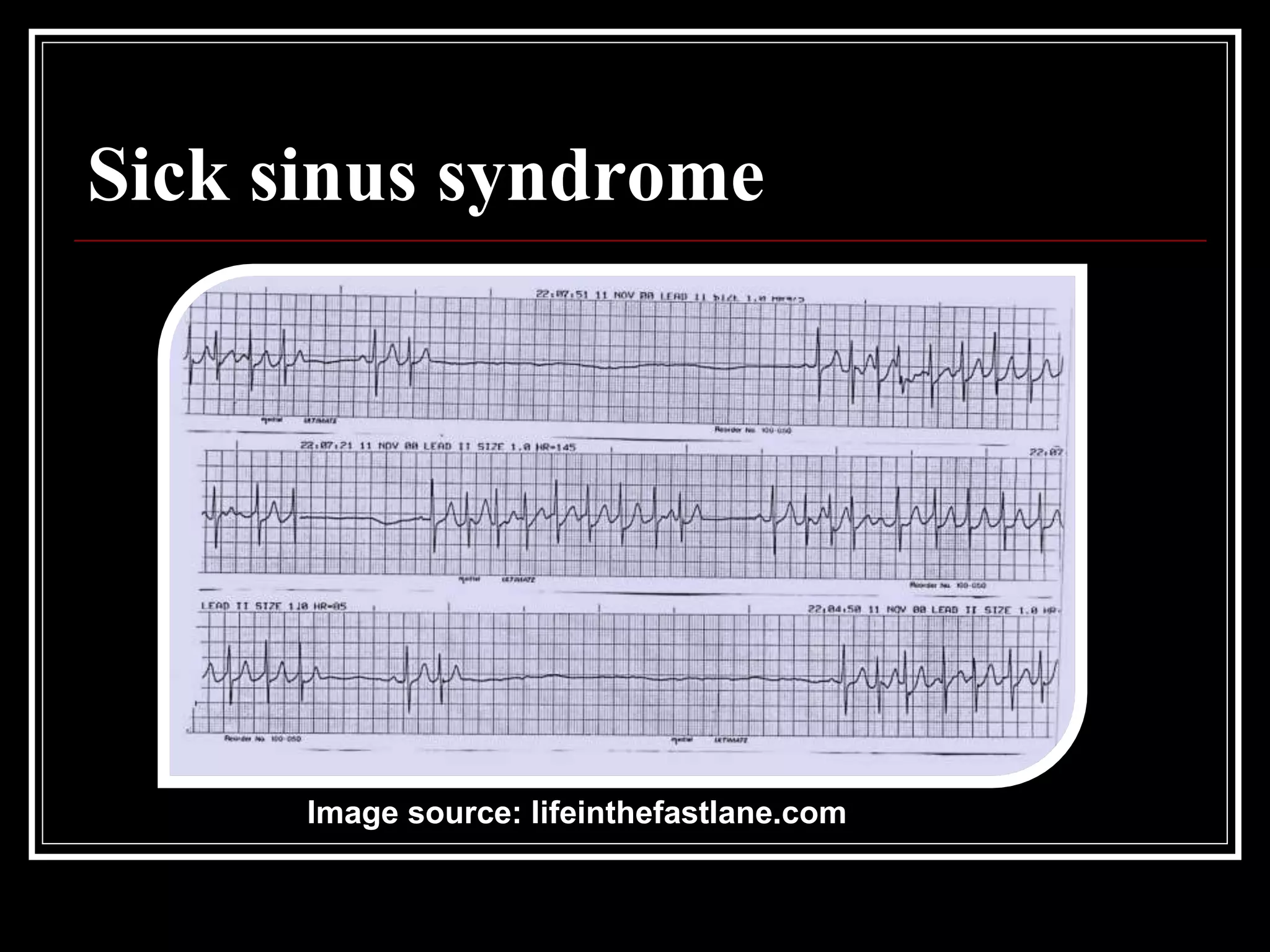
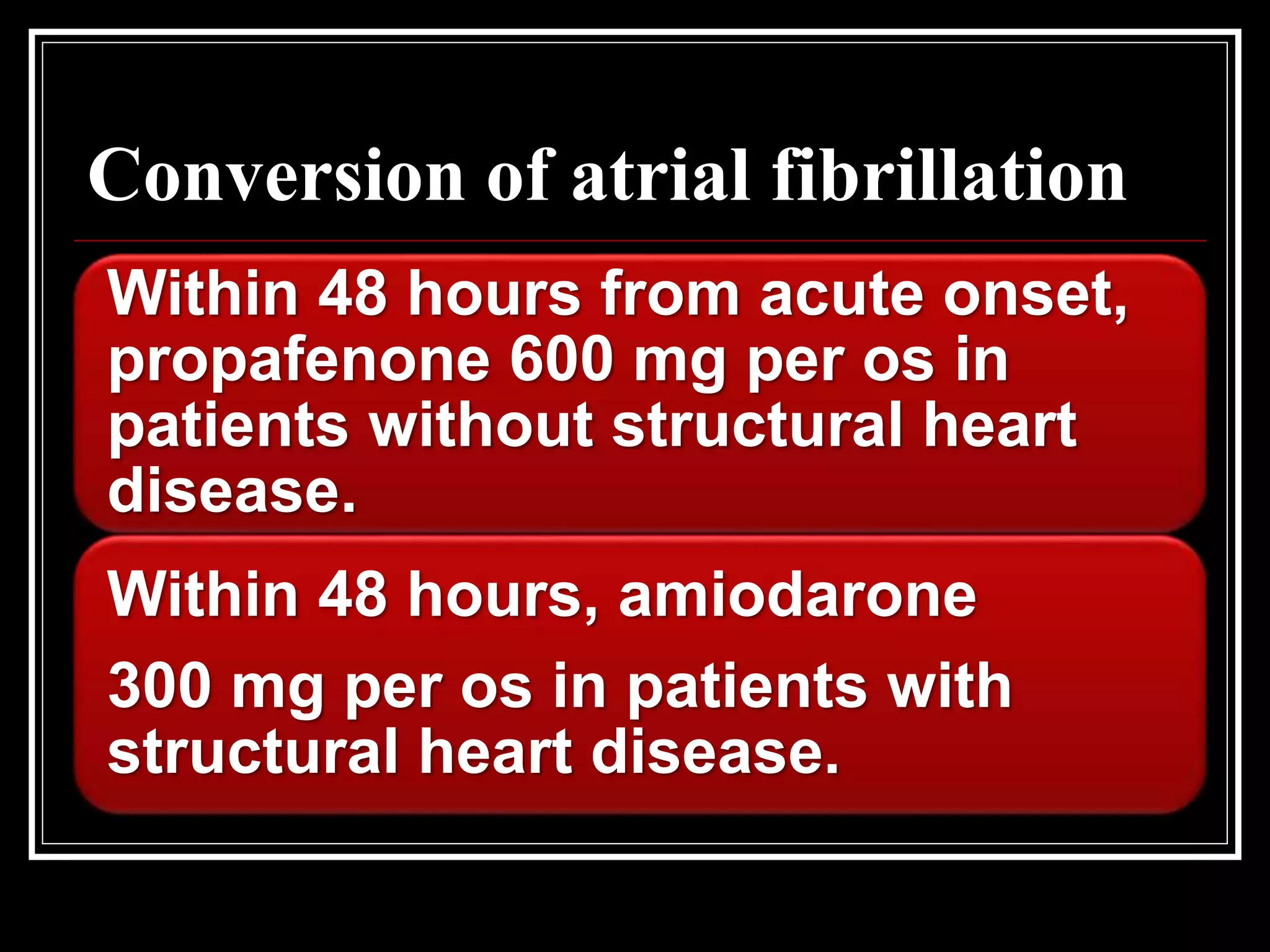
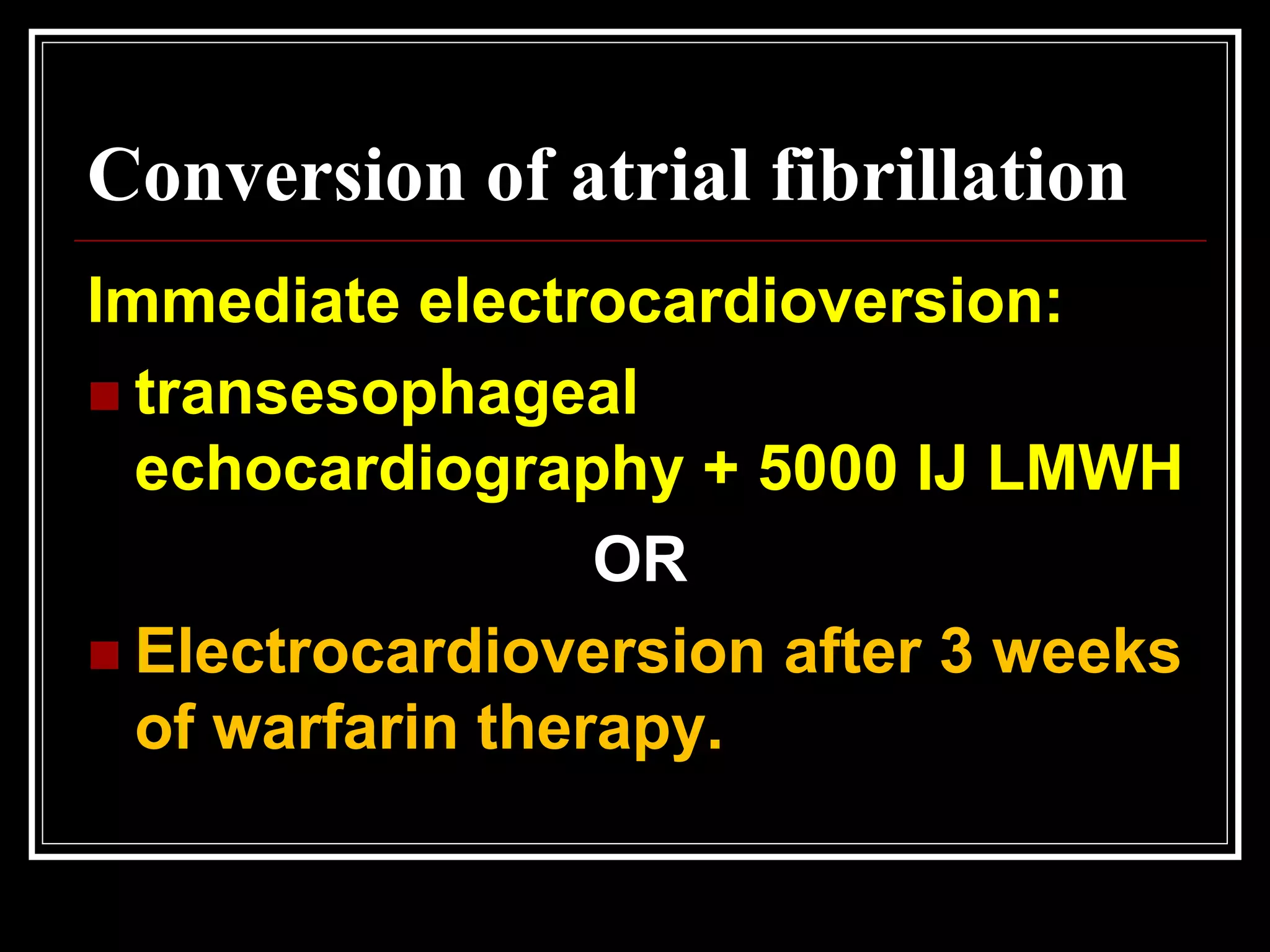
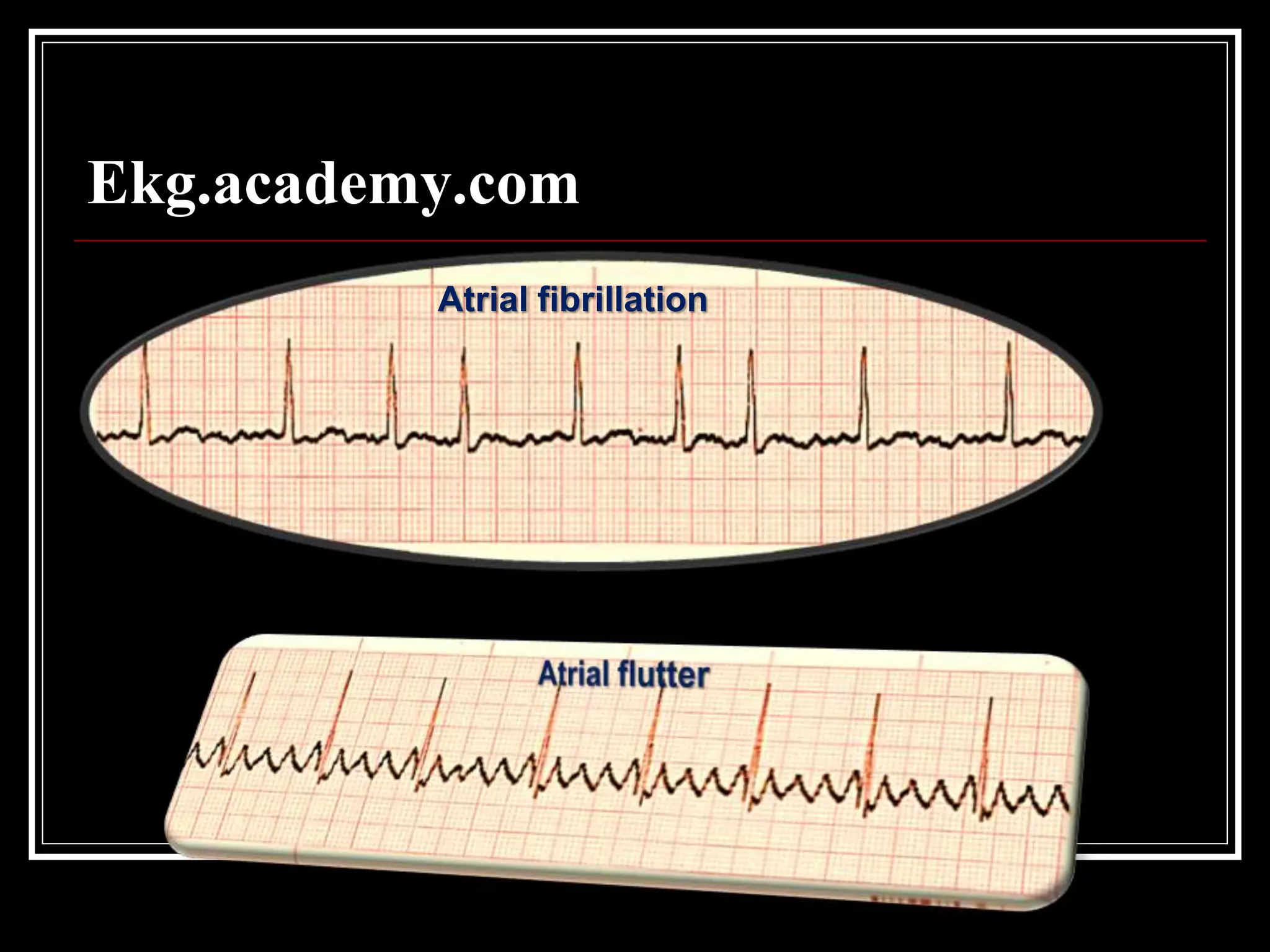
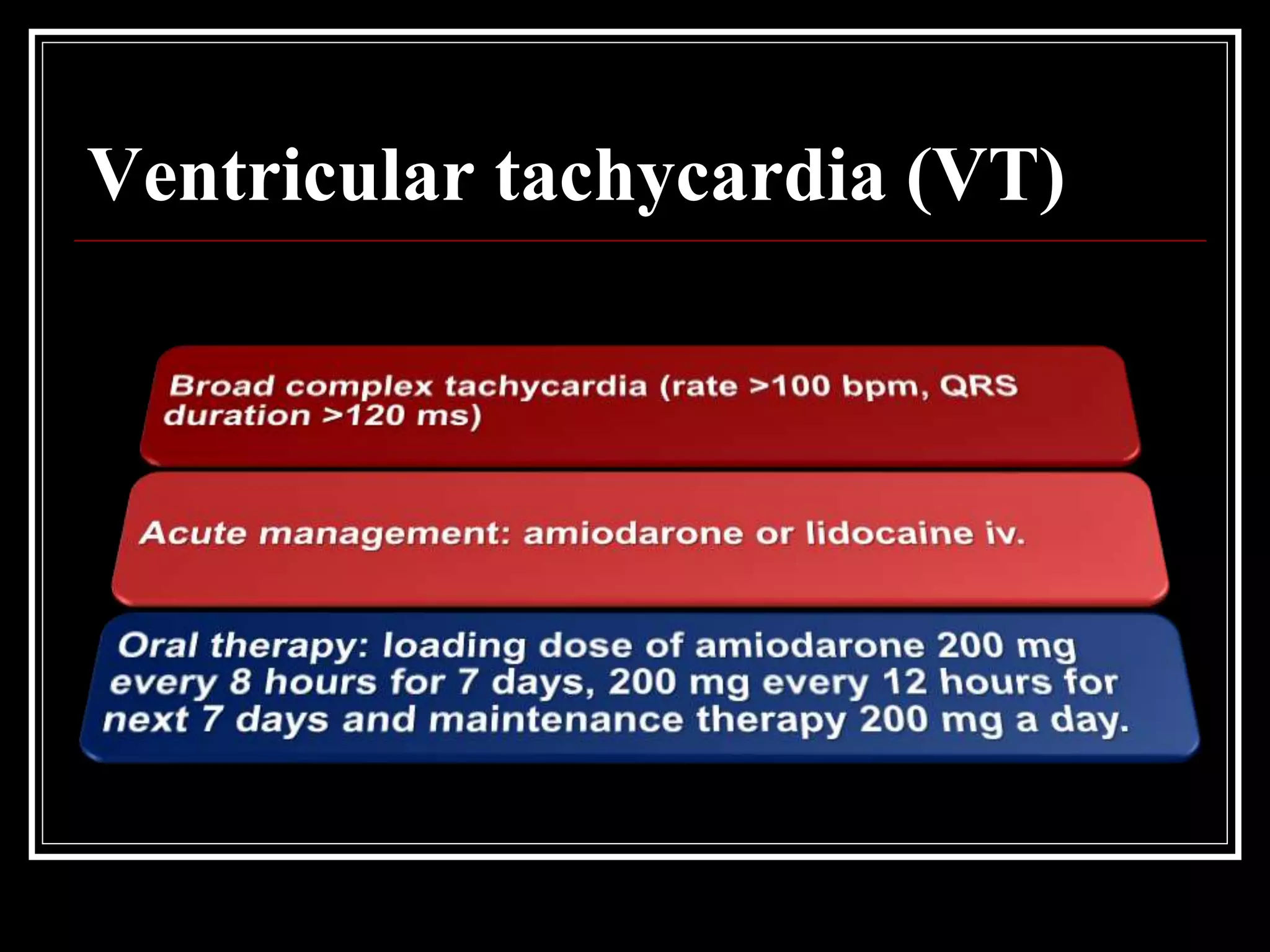
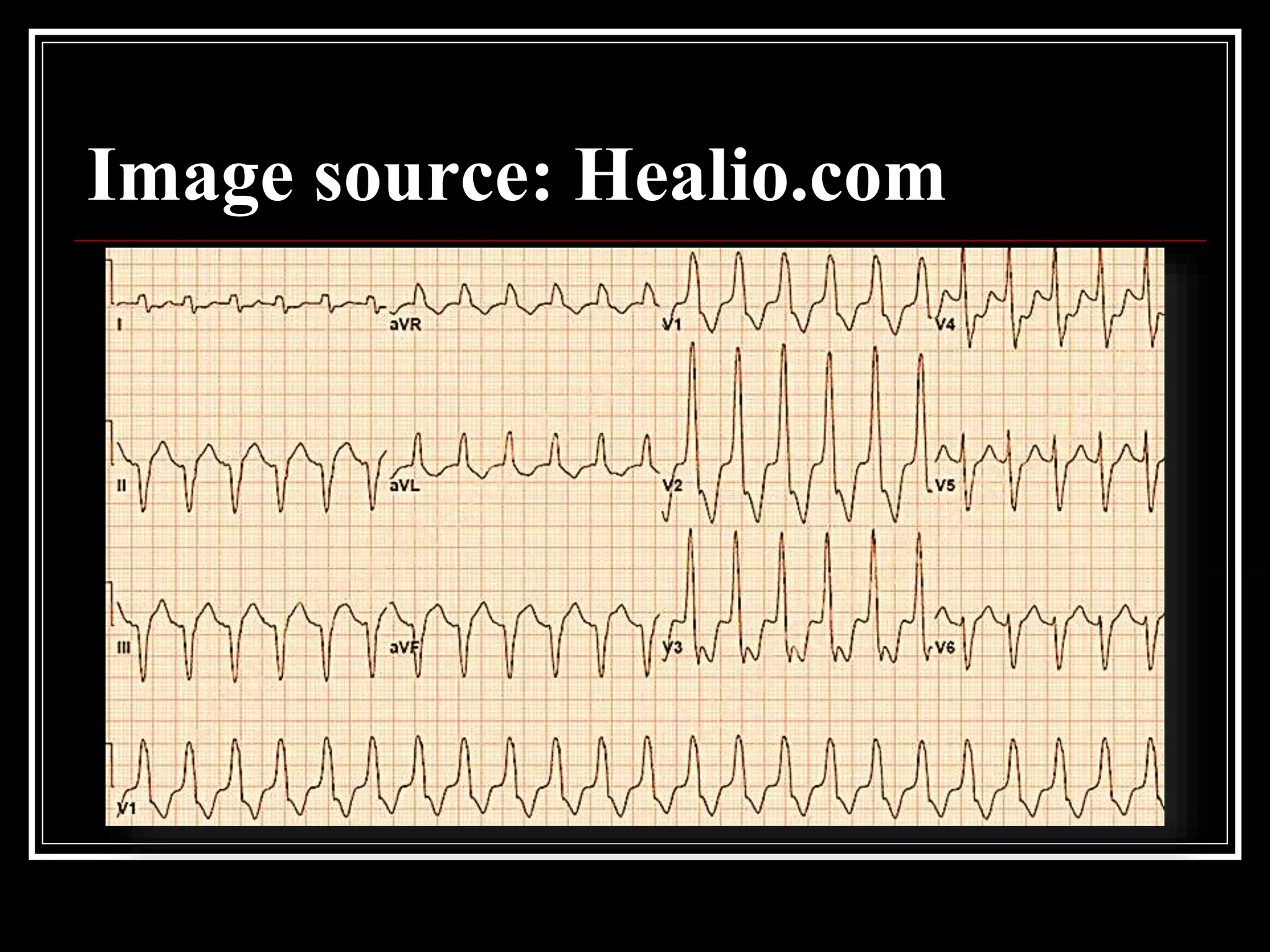
This document discusses arrhythmias, including their causes, symptoms, diagnosis, and treatment. Arrhythmias can be caused by cardiac issues like heart attacks or non-cardiac issues like drugs or metabolic imbalances. Common symptoms include palpitations, chest pain, fainting, and breathlessness. Diagnosis involves blood tests, ECGs, heart monitoring, and imaging. Treatment depends on the type of arrhythmia but may include medications, cardioversion, or pacemakers. The document provides details on evaluating and managing common arrhythmias like bradycardia, atrial fibrillation, and ventricular tachycardia.