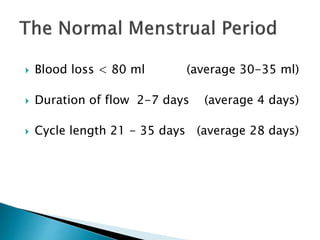
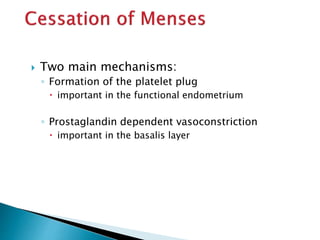
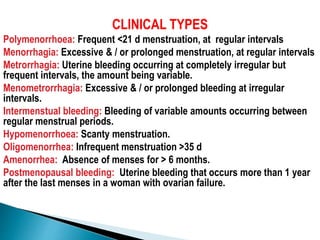
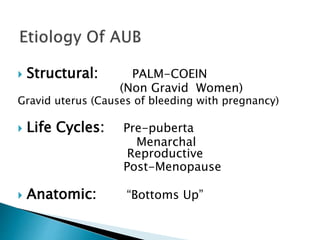
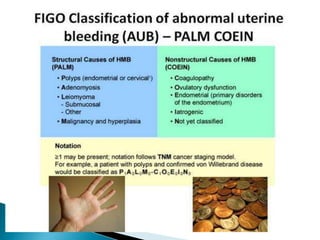
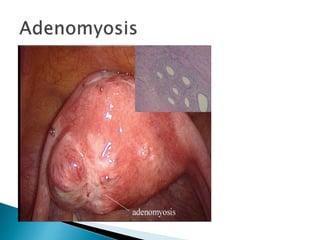
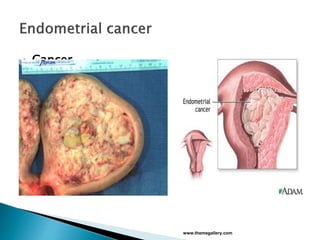
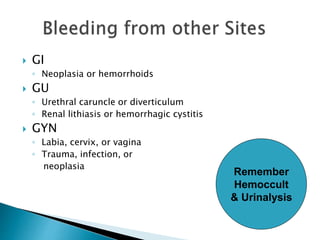
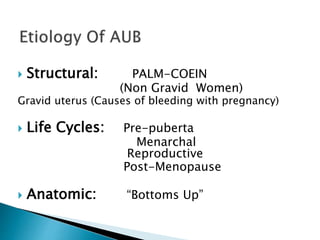
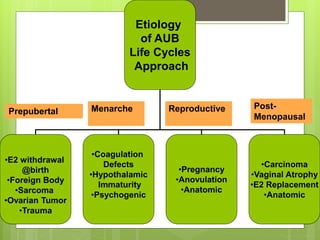
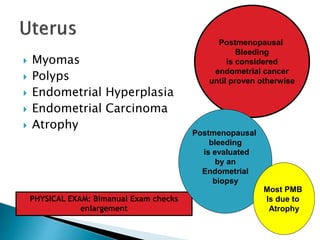
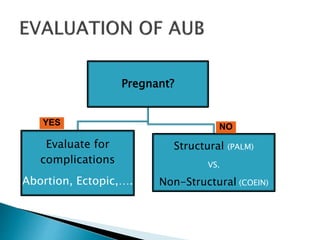
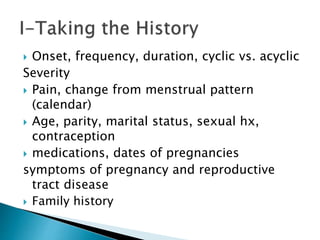
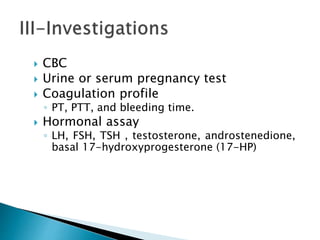
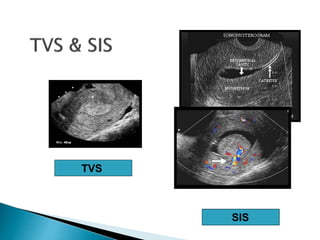
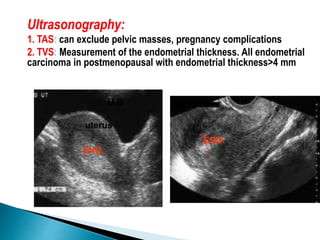
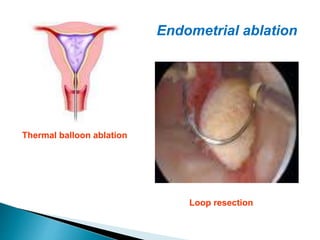
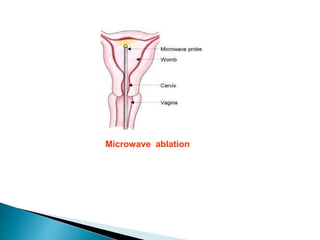
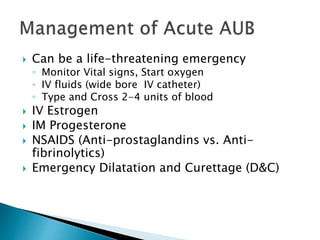
The document summarizes information about the menstrual cycle and abnormal uterine bleeding. It describes the typical phases and hormone levels during a normal menstrual cycle. It then defines and categorizes different types of abnormal uterine bleeding and lists potential structural and non-structural causes. The document outlines evaluation and treatment approaches, including general measures, medical management, minimally invasive procedures, and major surgery.