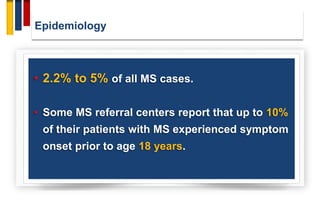
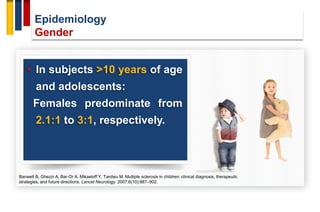
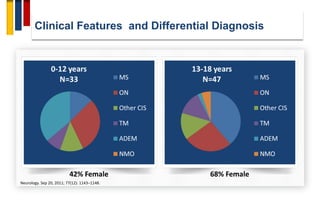
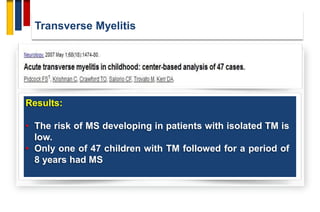
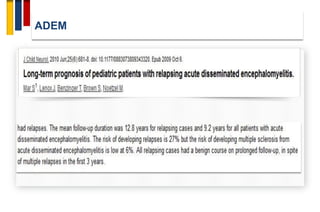
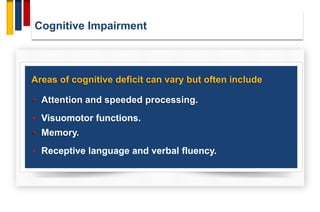
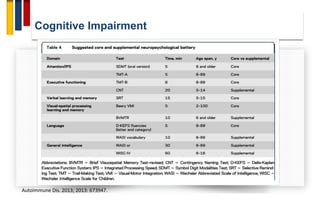
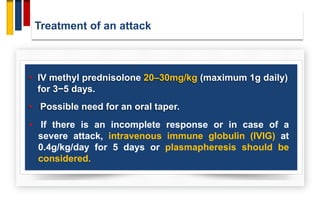
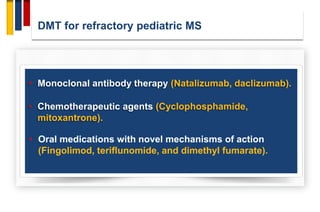
This document discusses pediatric multiple sclerosis. It begins with defining pediatric MS as occurring in children under 18 years old. It then covers the epidemiology, finding the incidence is highest between 13-16 years old and females are more commonly affected than males. Risk factors discussed include genetics, obesity, and passive smoking. The pathophysiology in pediatric MS involves less axonal damage and innate immune response dominance over adaptive. Clinical features can include polysymptomatic or monosymptomatic presentations, and differential diagnosis must consider ADEM, CIS, and other conditions. MRI and CSF findings are discussed. Treatment involves steroids for attacks and first-line DMTs like interferons and glatiramer acetate.