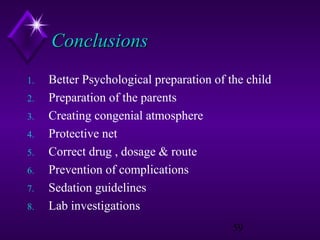
Modern Trends in Paediatric Preparation and Premedication discusses:
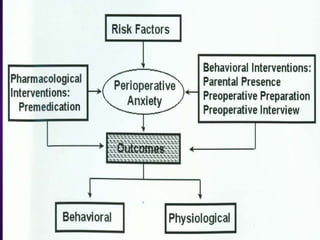
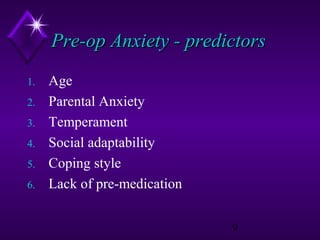
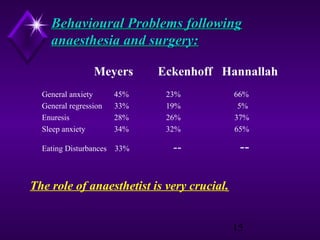
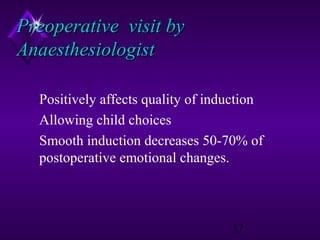
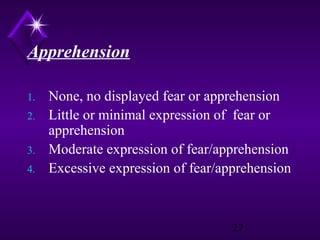
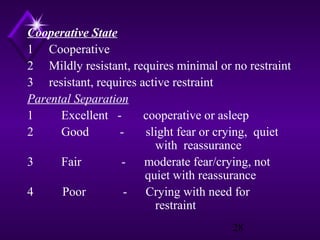
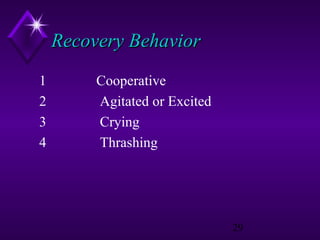
1. Various risk factors for pre-op anxiety in children and interventions like behavioral and pharmacological approaches.
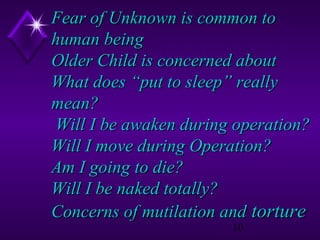
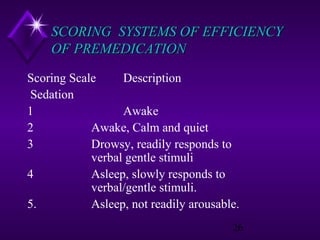
2. Psychological effects of surgery and anesthesia on children and the importance of pre-medication.
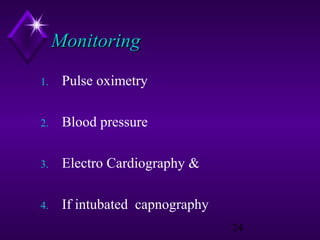
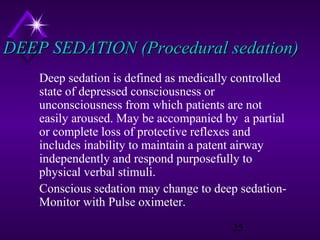
3. Guidelines for monitoring patients under sedation and different levels of sedation.
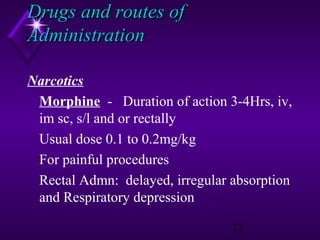
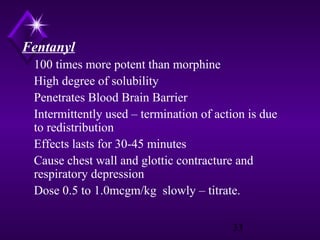
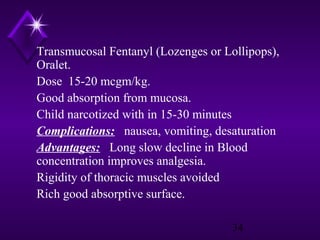
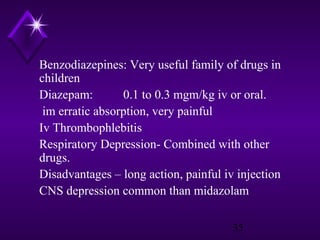
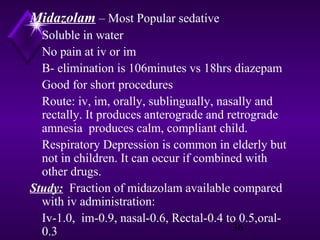
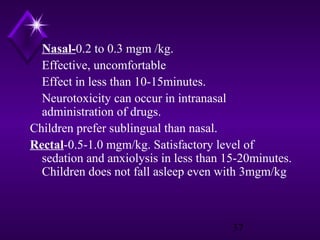
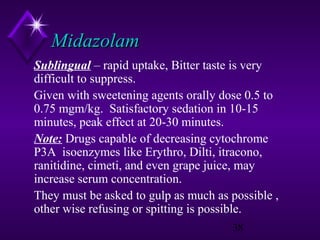
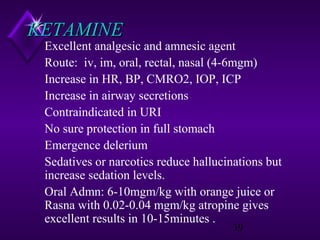
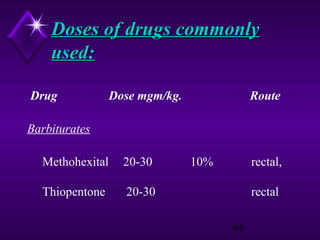
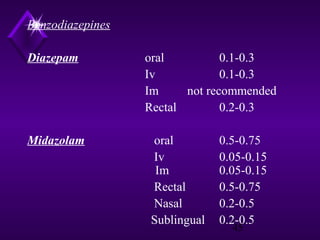
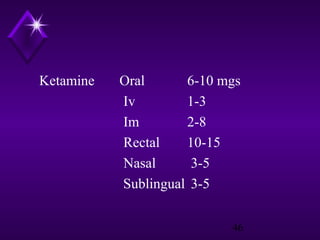
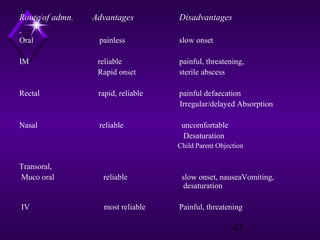
4. Common drugs used for pre-medication like midazolam, ketamine and fentanyl, their doses, routes of administration and potential complications."