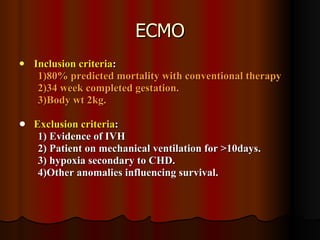
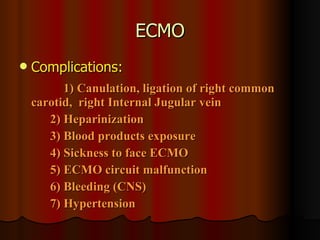
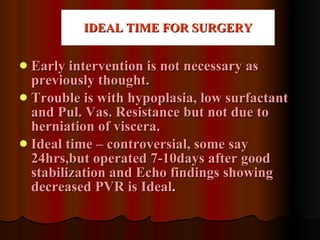
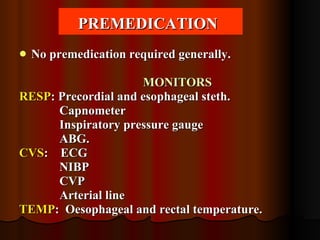
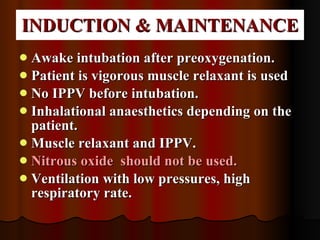
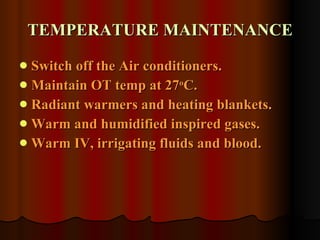
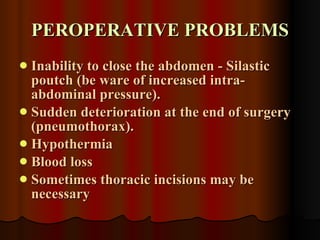
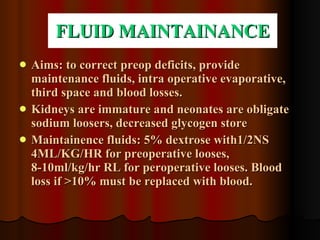
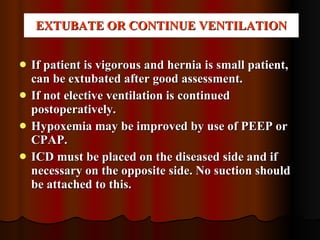
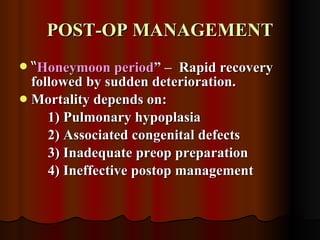
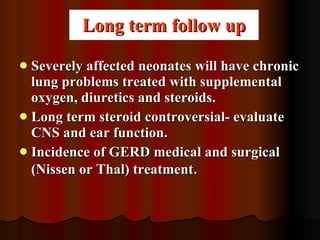
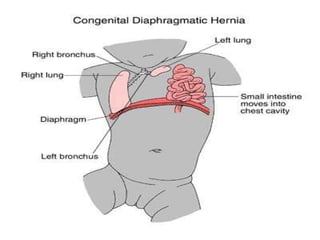
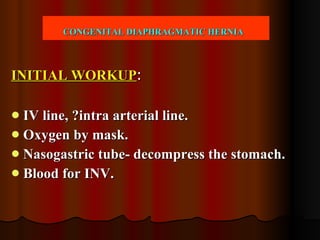
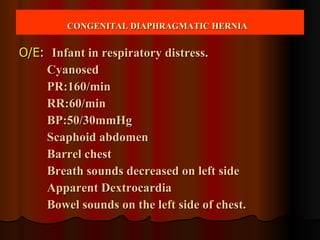
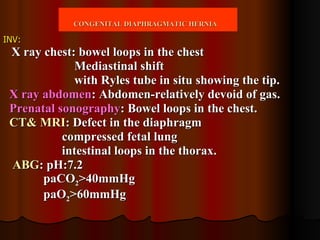
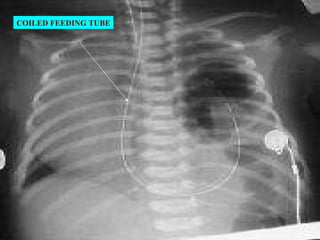
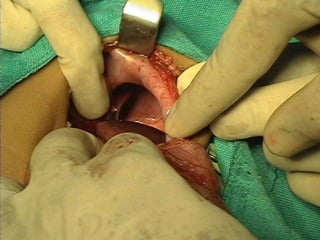
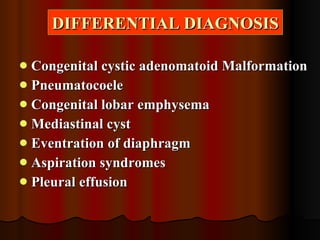
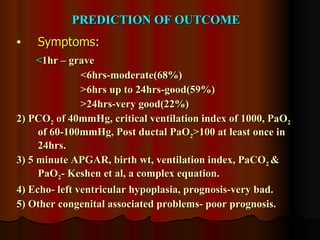
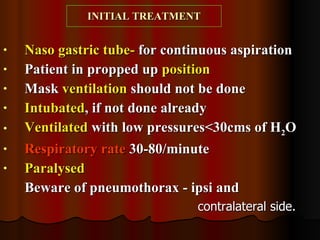
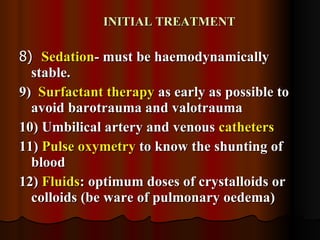
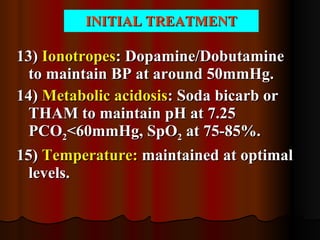
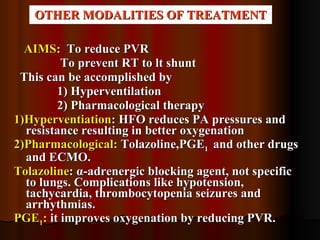
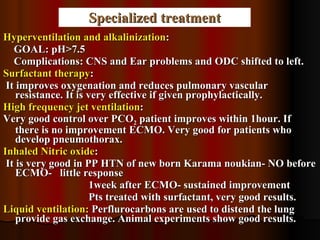
This document discusses the treatment of congenital diaphragmatic hernia in infants. It outlines the initial workup, assessment, differential diagnosis, prediction of outcomes, initial treatment including ventilation and medication management. It also discusses specialized treatments like ECMO, timing of surgery, anesthesia management during surgery, postoperative care and long term follow up.





![ECMO ECMO : VV/VA. Indications: 1) Failure of medical treatment to reverse hypoxia. 2) Acute clinical deterioration 3) P[(A-a)O 2 ]>600mmHg for 8hrs 4) O 2 Index [(FIO 2 X MAP)/PaO] of 51 for 5hrs. 5) Failure to respond to maximal therapy. 6) Cardiac arrest. VA ECMO- Flow 100ML/KG/MIN Goals: PaO2:60-100mmHg PaCO 2 ;30-45mmHg. VV ECMO- Does not support cardiovascular function and PaO 2 less.](https://image.slidesharecdn.com/congenitaldiaphragmatichernia2-110903045950-phpapp02/85/Congenital-diaphragmatic-hernia2-21-320.jpg)