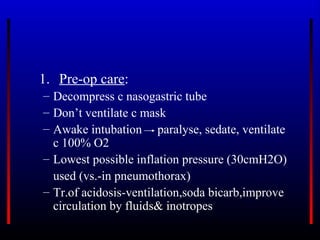
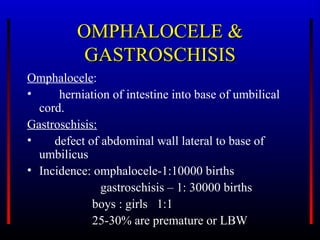
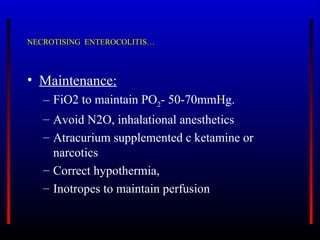
The document discusses various pediatric surgical conditions and their anesthetic management, including pyloric stenosis, tracheoesophageal fistula, congenital diaphragmatic hernia, intestinal obstruction, omphalocele, gastroschisis, and necrotizing enterocolitis. For each condition, it covers topics like incidence, etiology, clinical presentation, pre-operative preparation and management, induction and maintenance of anesthesia, as well as post-operative care and complications.