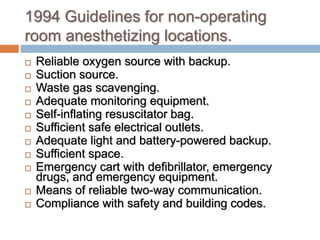
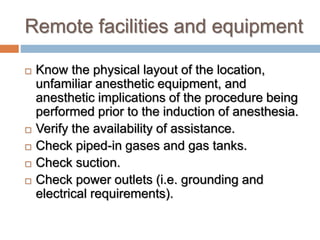
The document outlines the principles and guidelines for administering anesthesia outside of the operating room, emphasizing the need for standard care, safety measures, and effective communication in various settings. It details challenges unique to remote locations such as equipment condition, environmental factors, and specific patient needs, while also reviewing sedation levels and procedural anesthesia for various medical procedures. Key guidelines include ensuring adequate monitoring, emergency preparedness, and compliance with safety standards.