This document discusses pharmacological considerations for drug administration in pediatric patients. Key points include:
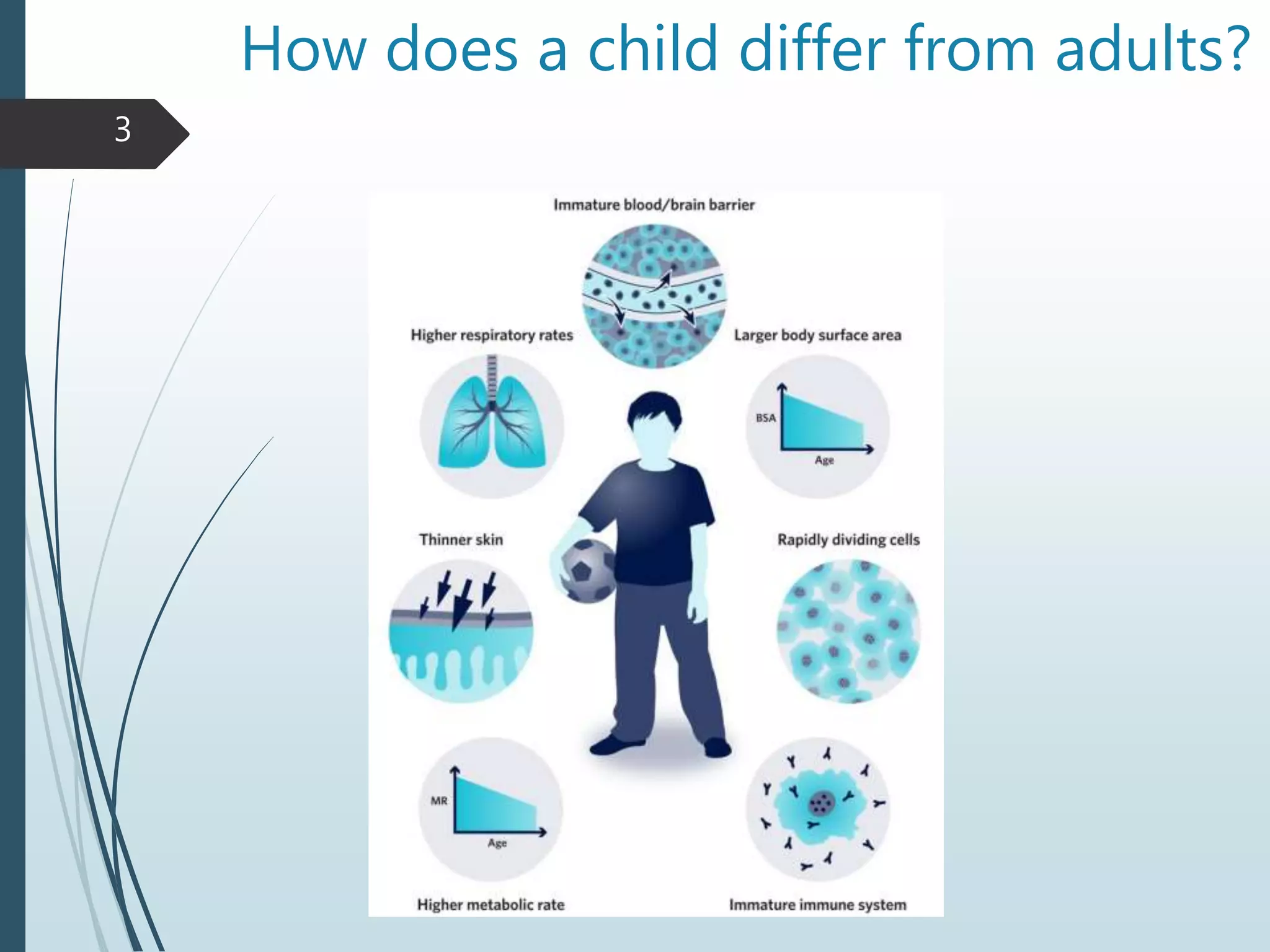
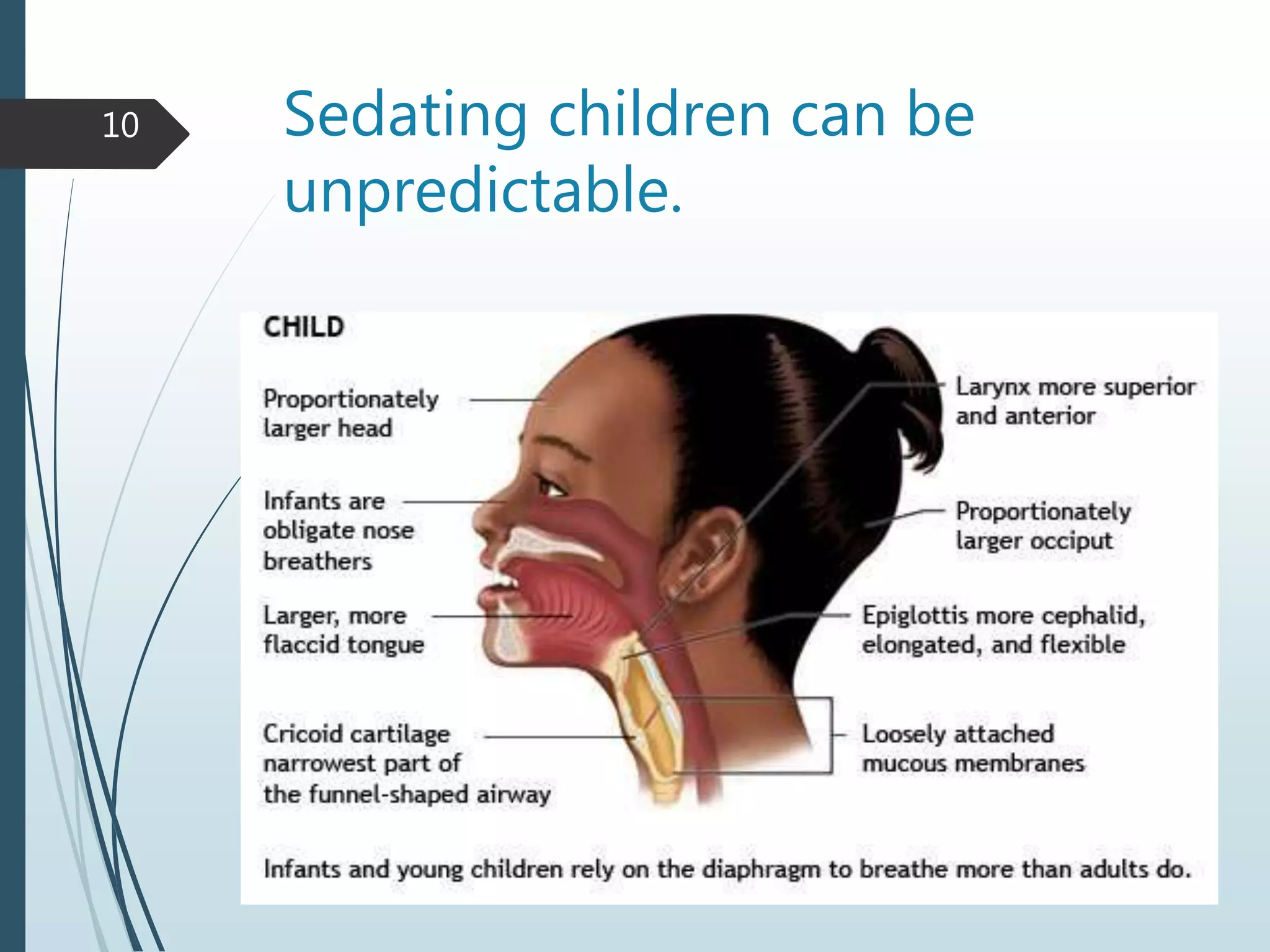
1) Children's bodies differ from adults in ways that impact drug metabolism like lower gastric acidity and immature renal function.
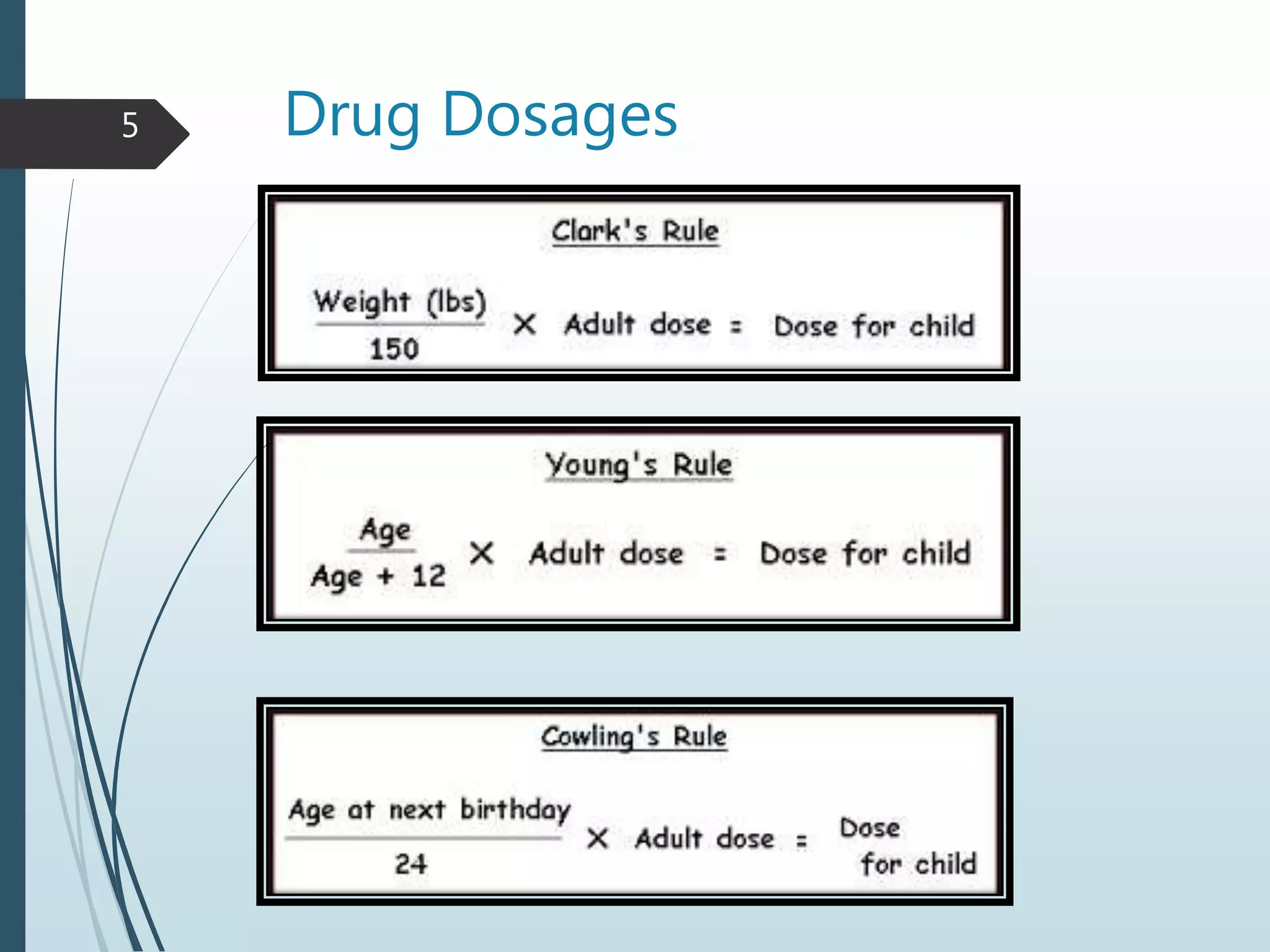
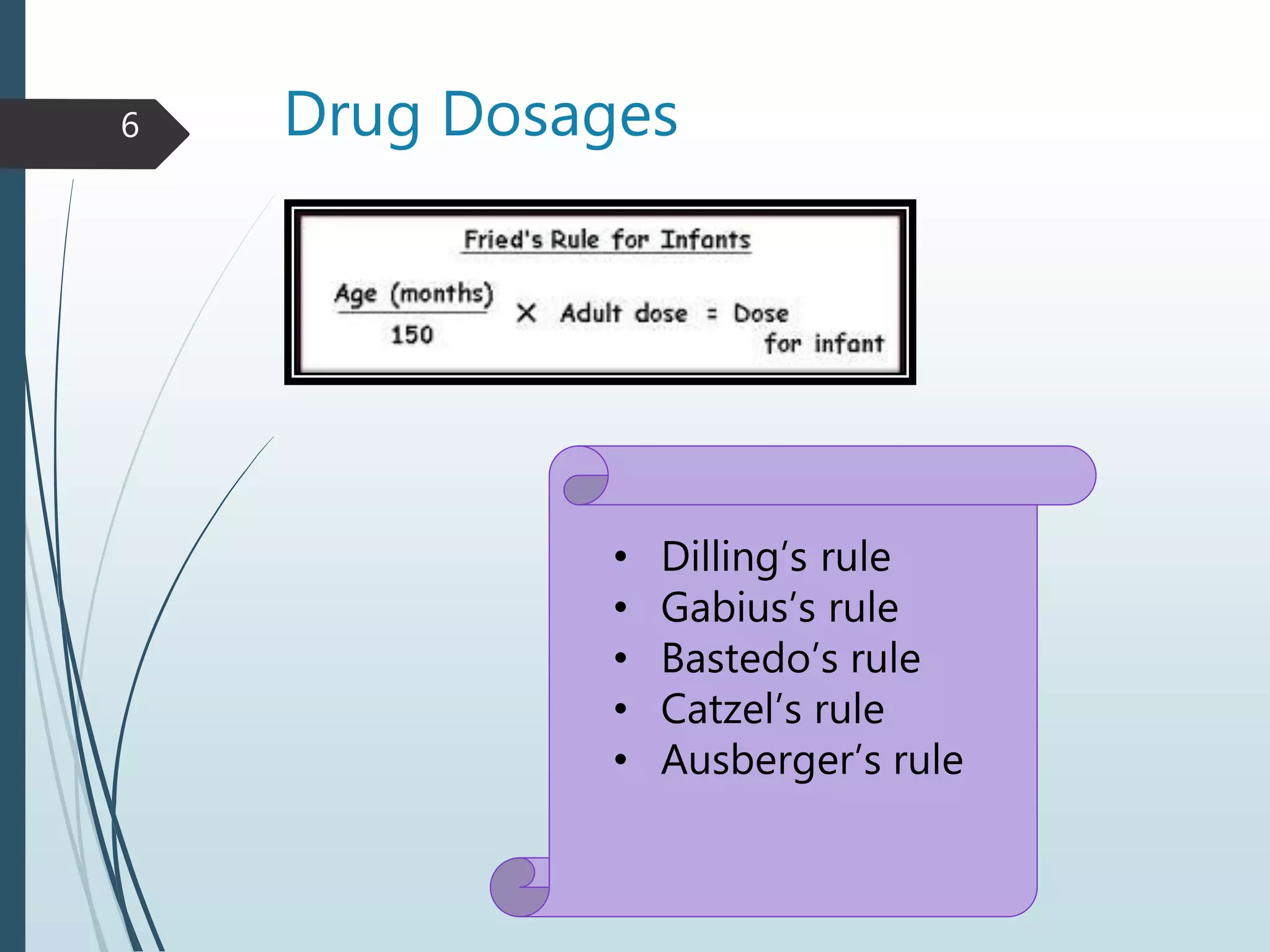
2) Several rules guide pediatric drug dosing calculations based on age and weight.
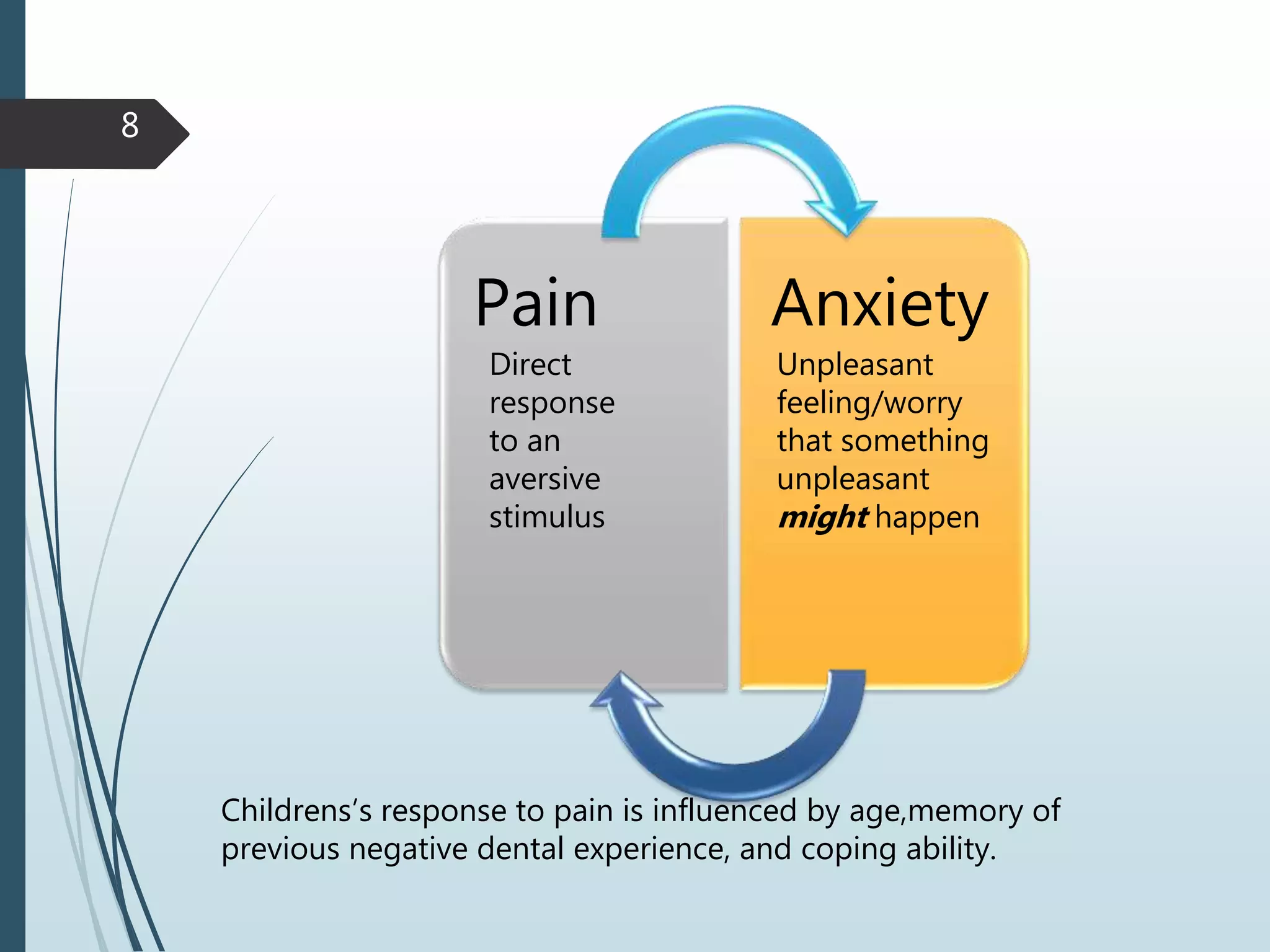
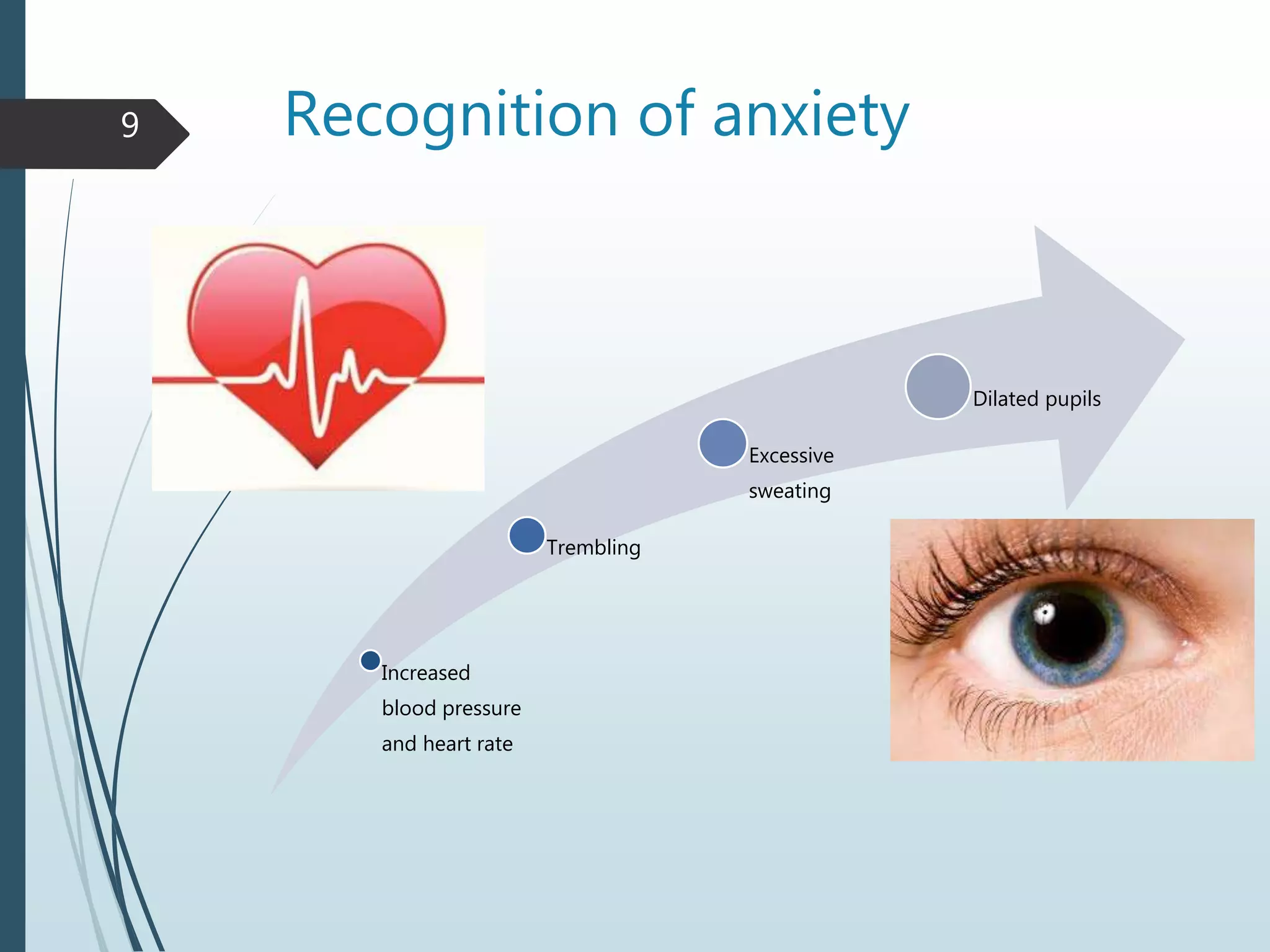
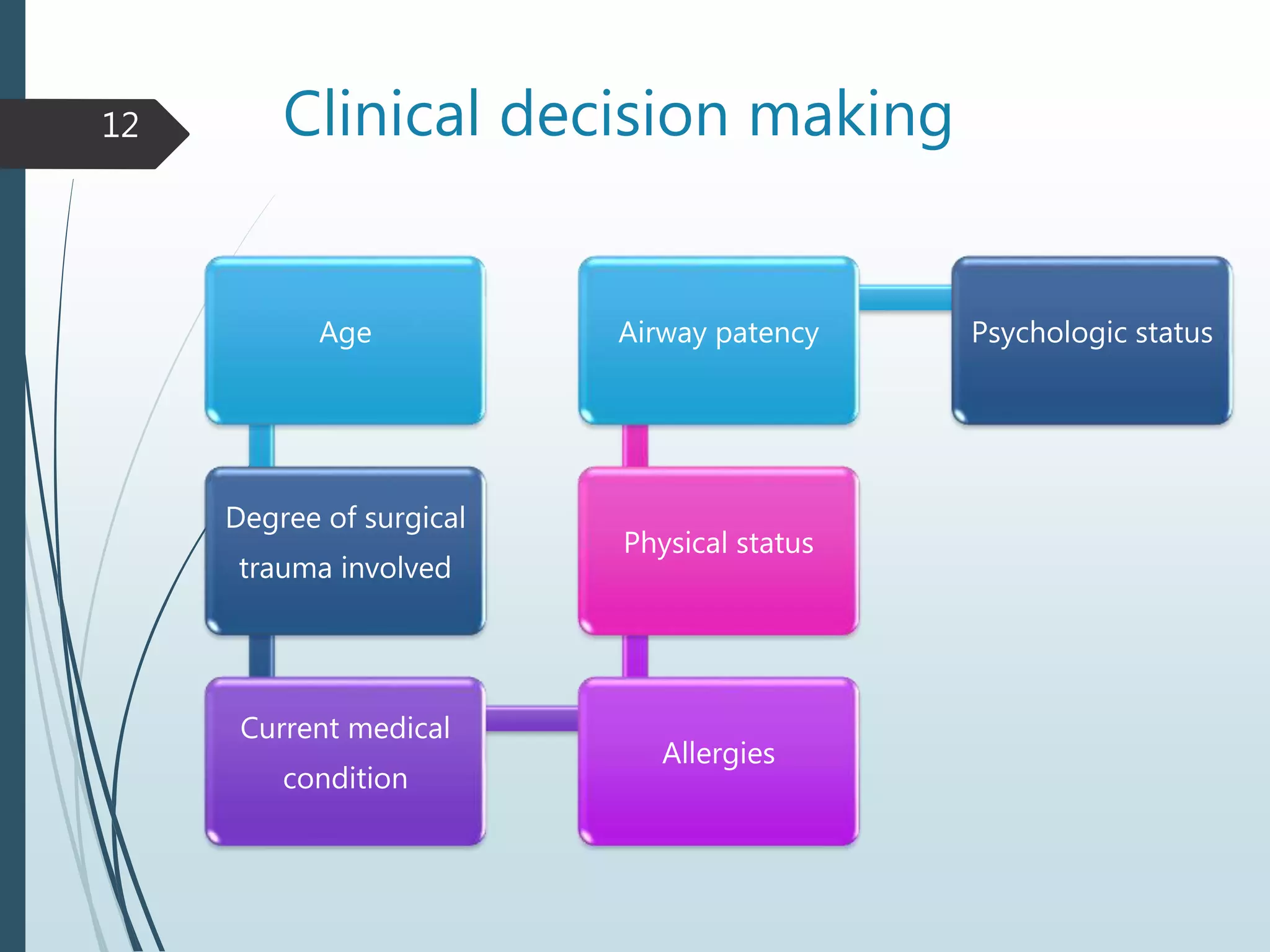
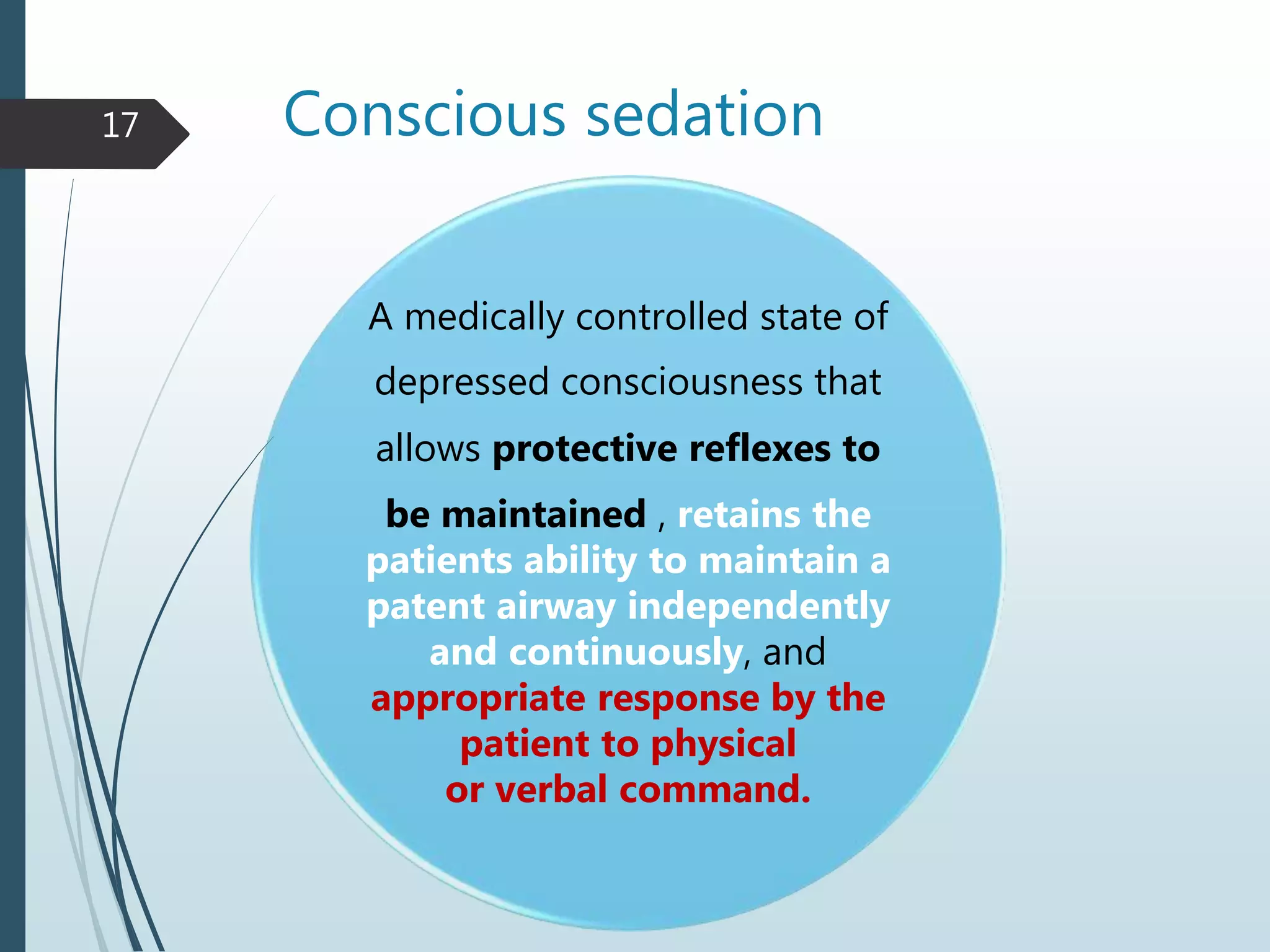
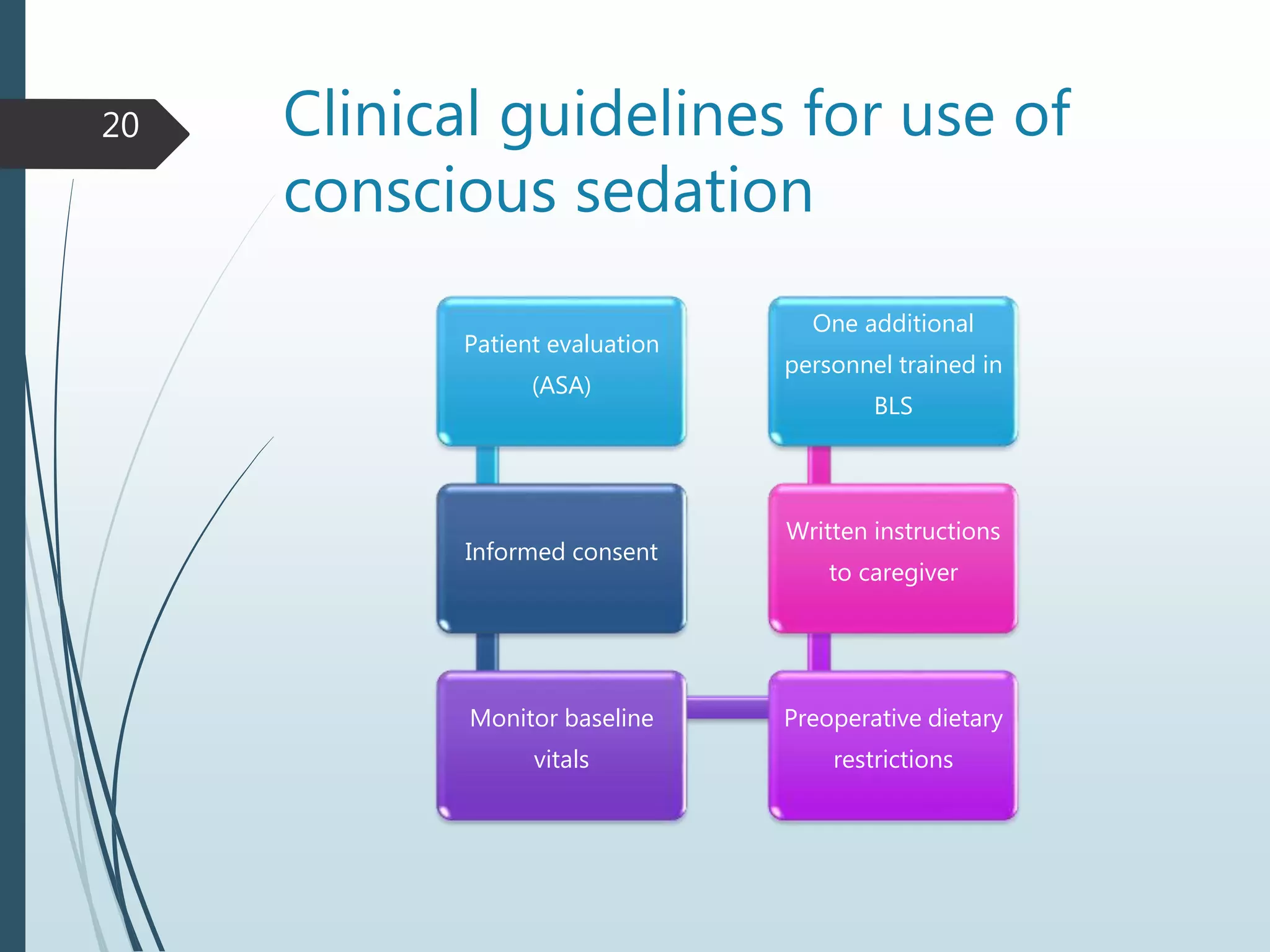
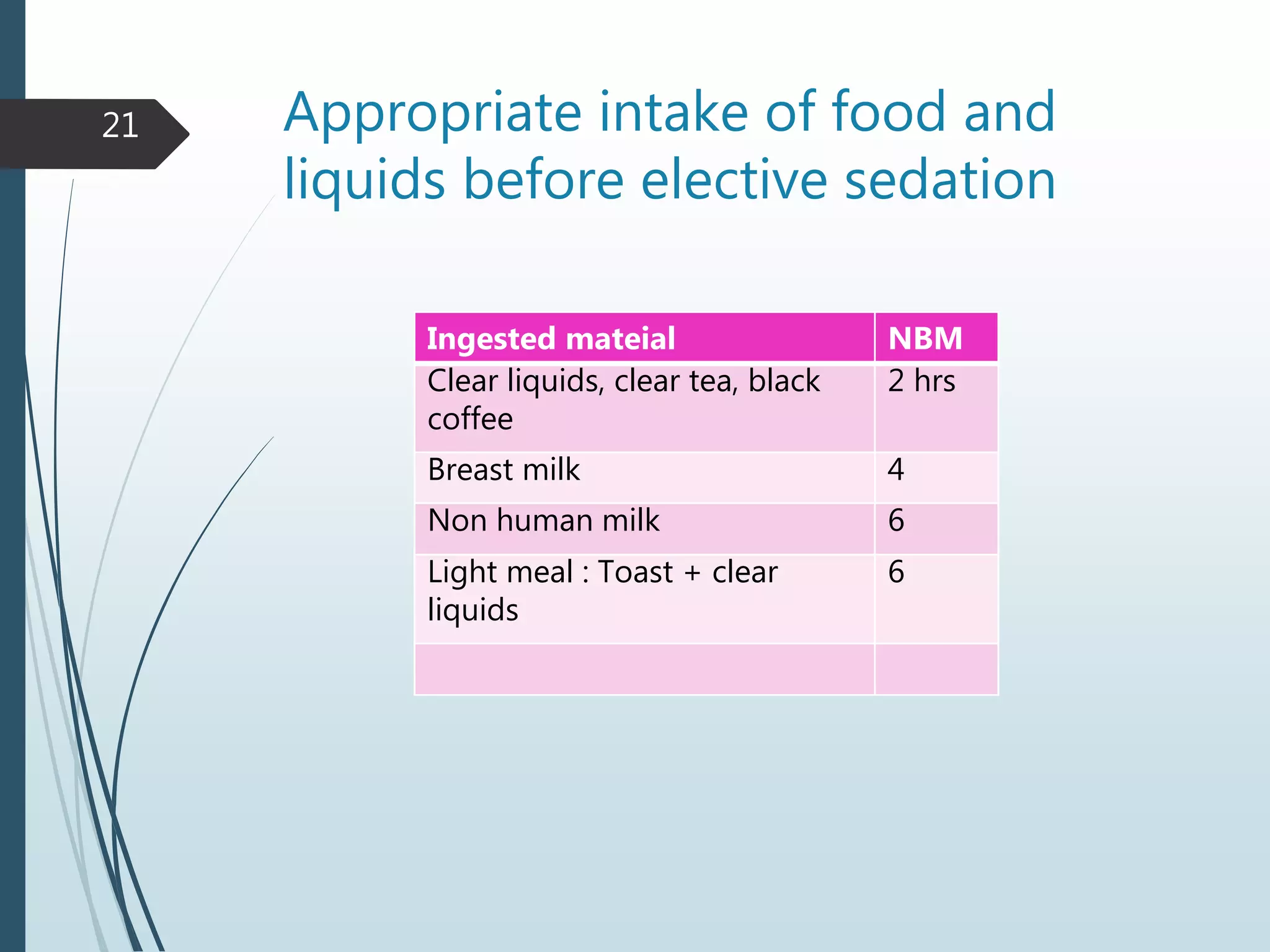
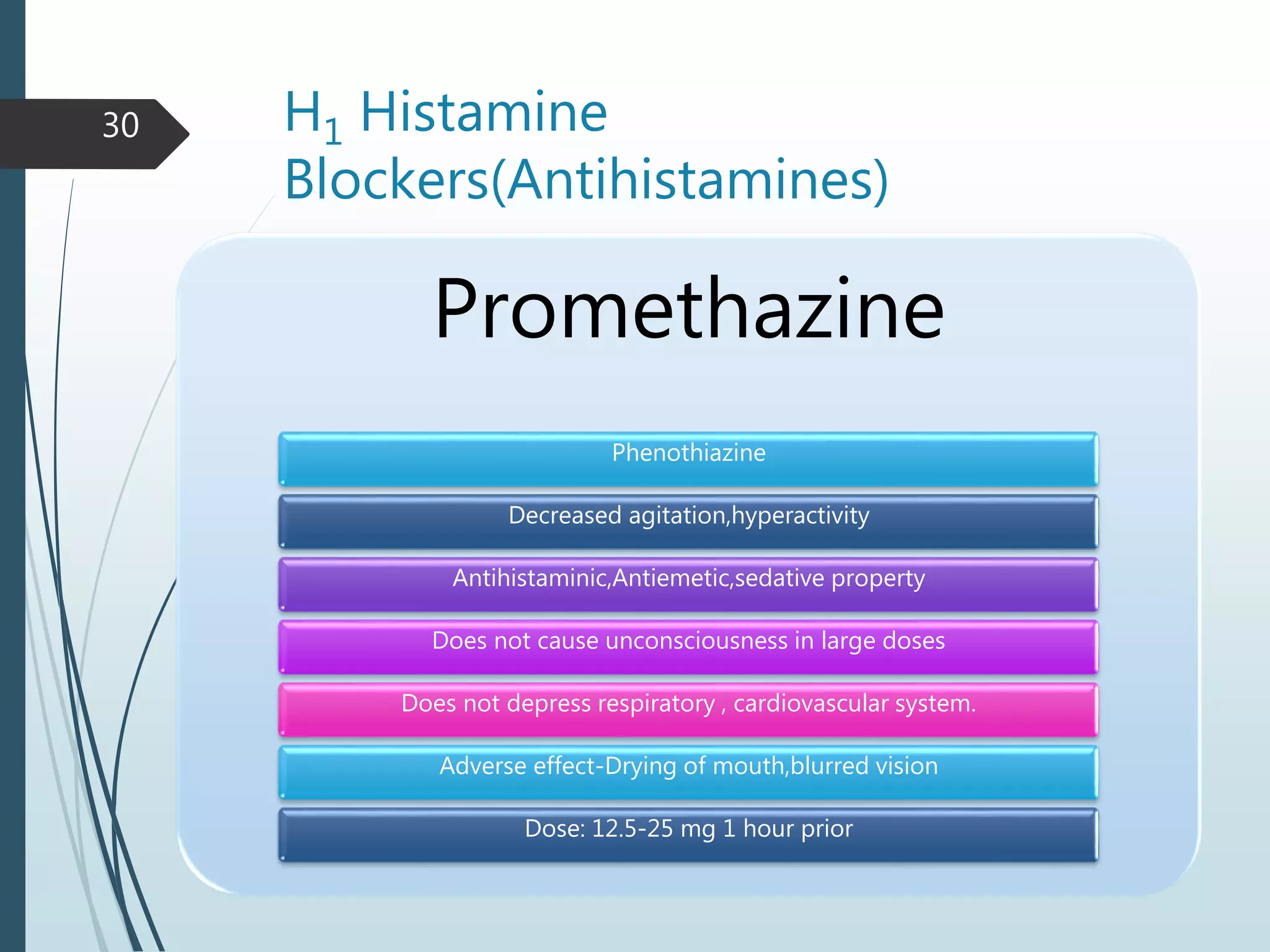
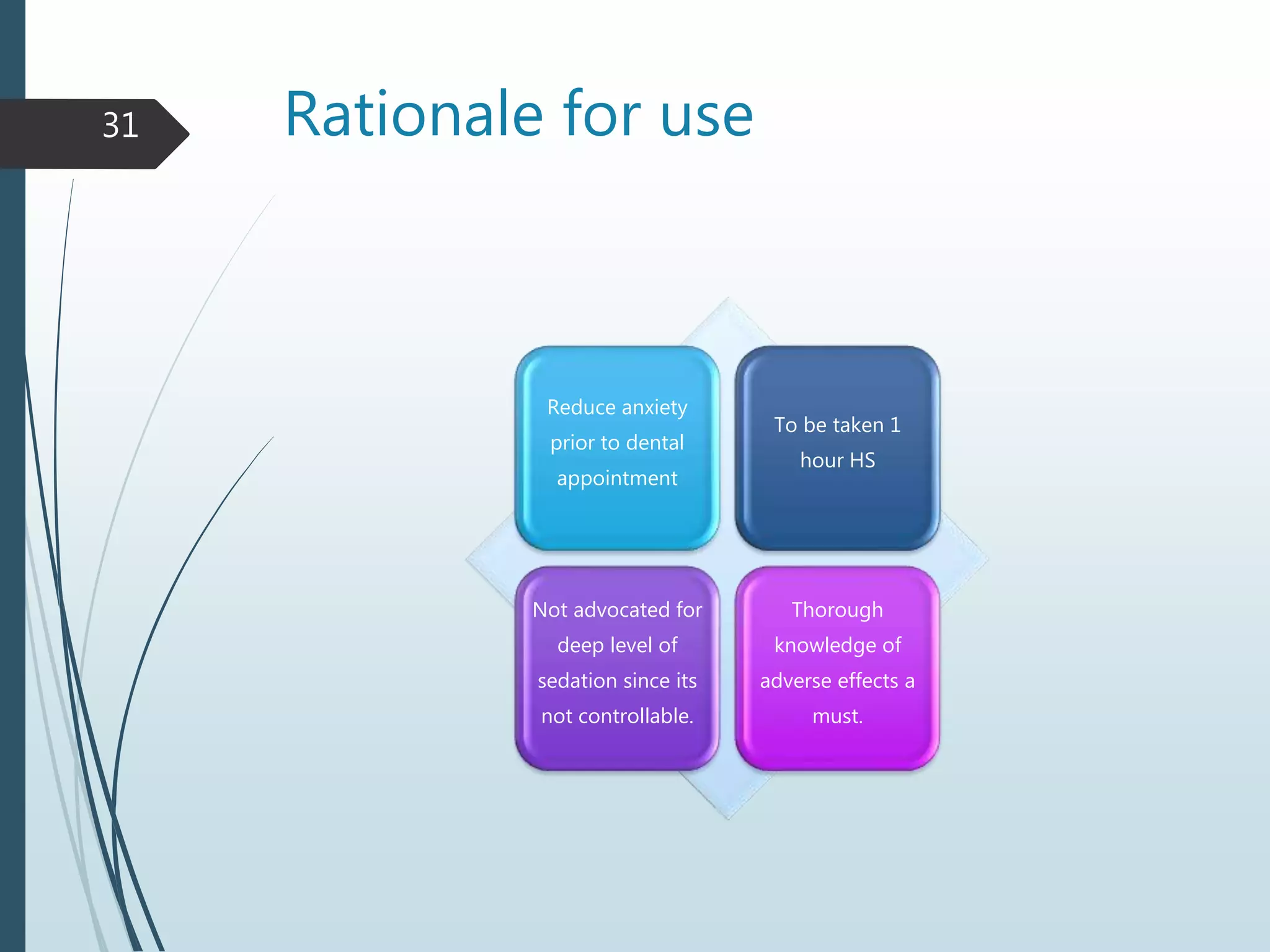
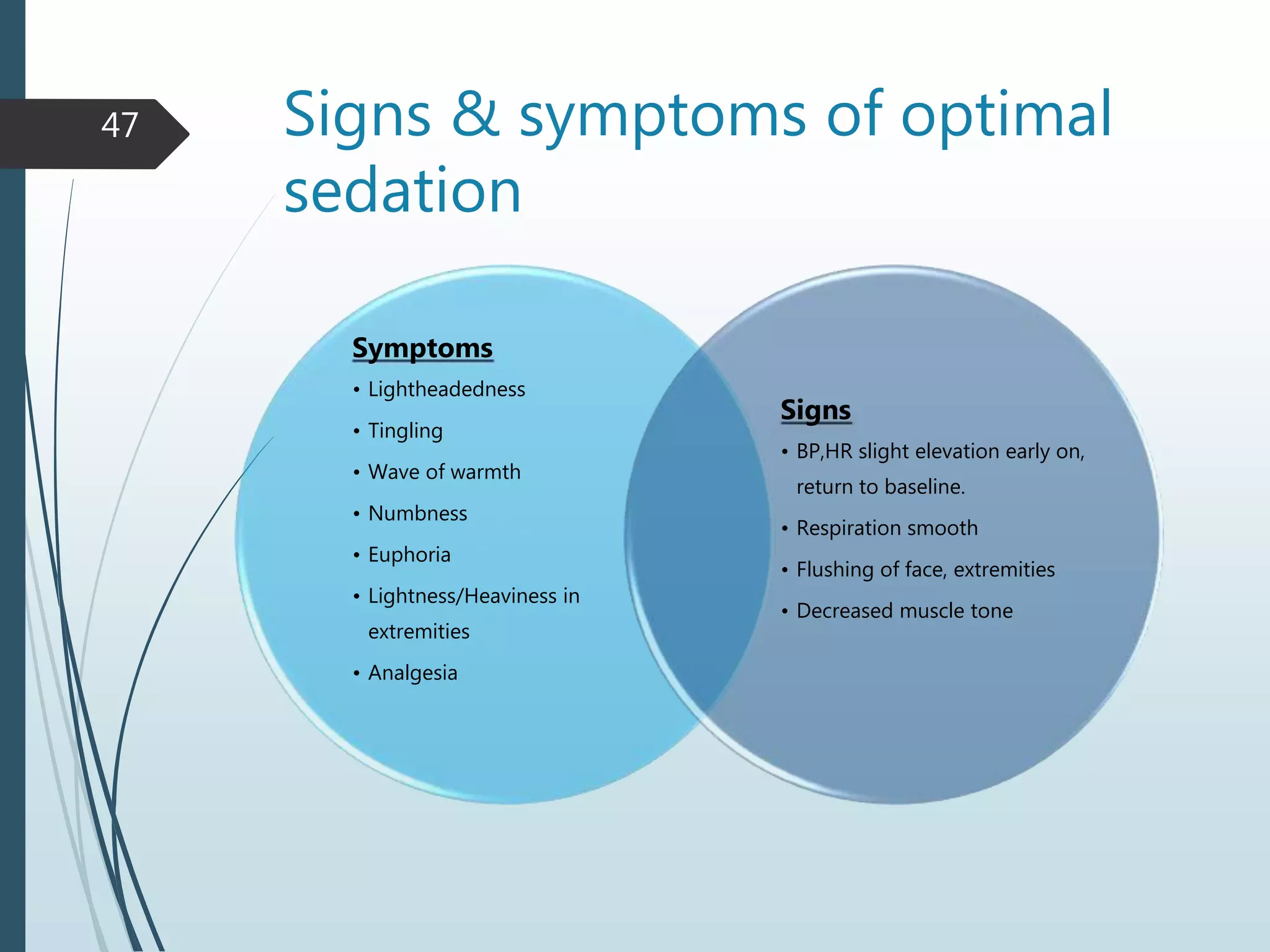
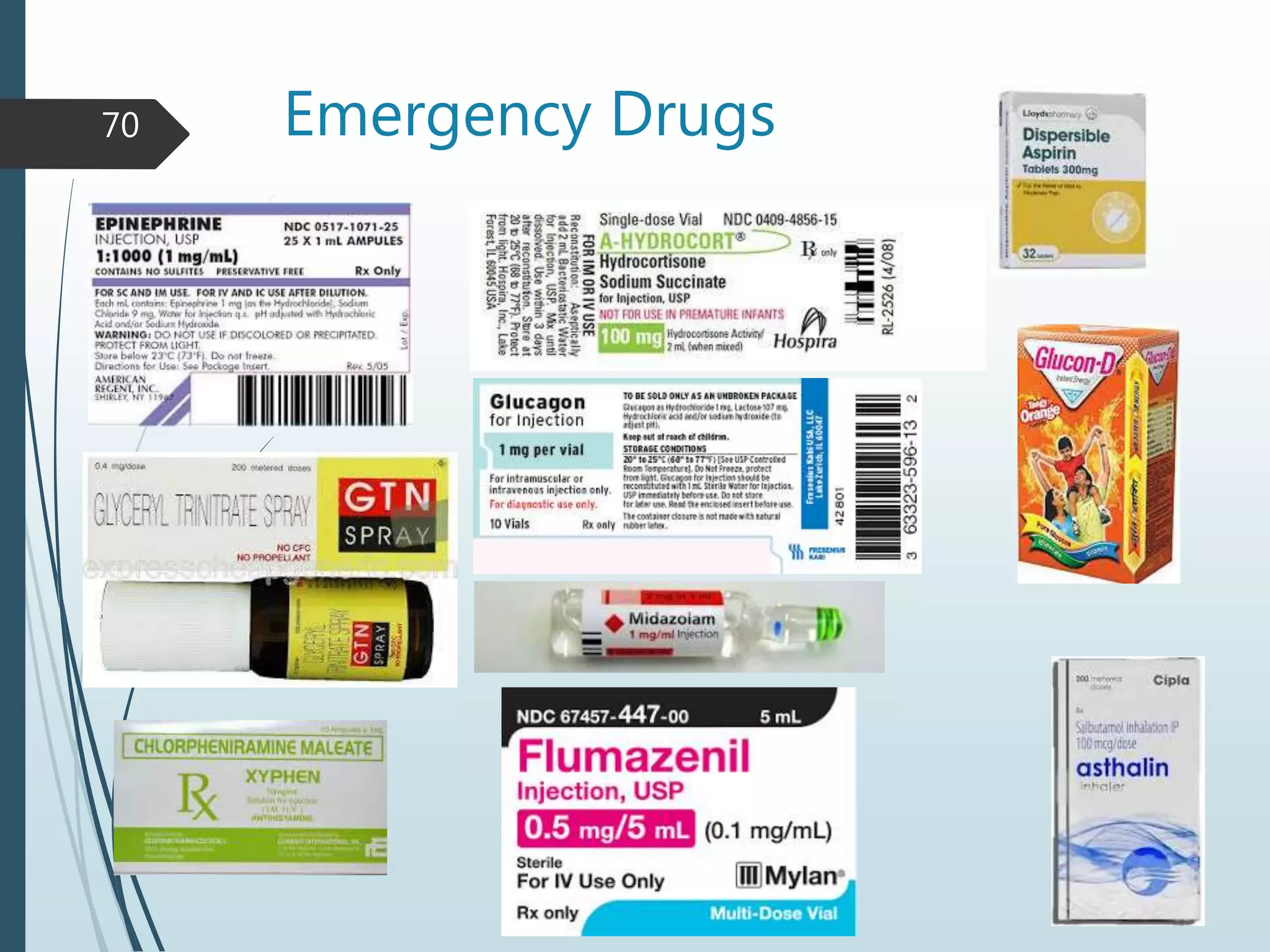
3) Common reasons for drug use in children include pain, anxiety, and infections. Guidelines for conscious sedation are outlined.
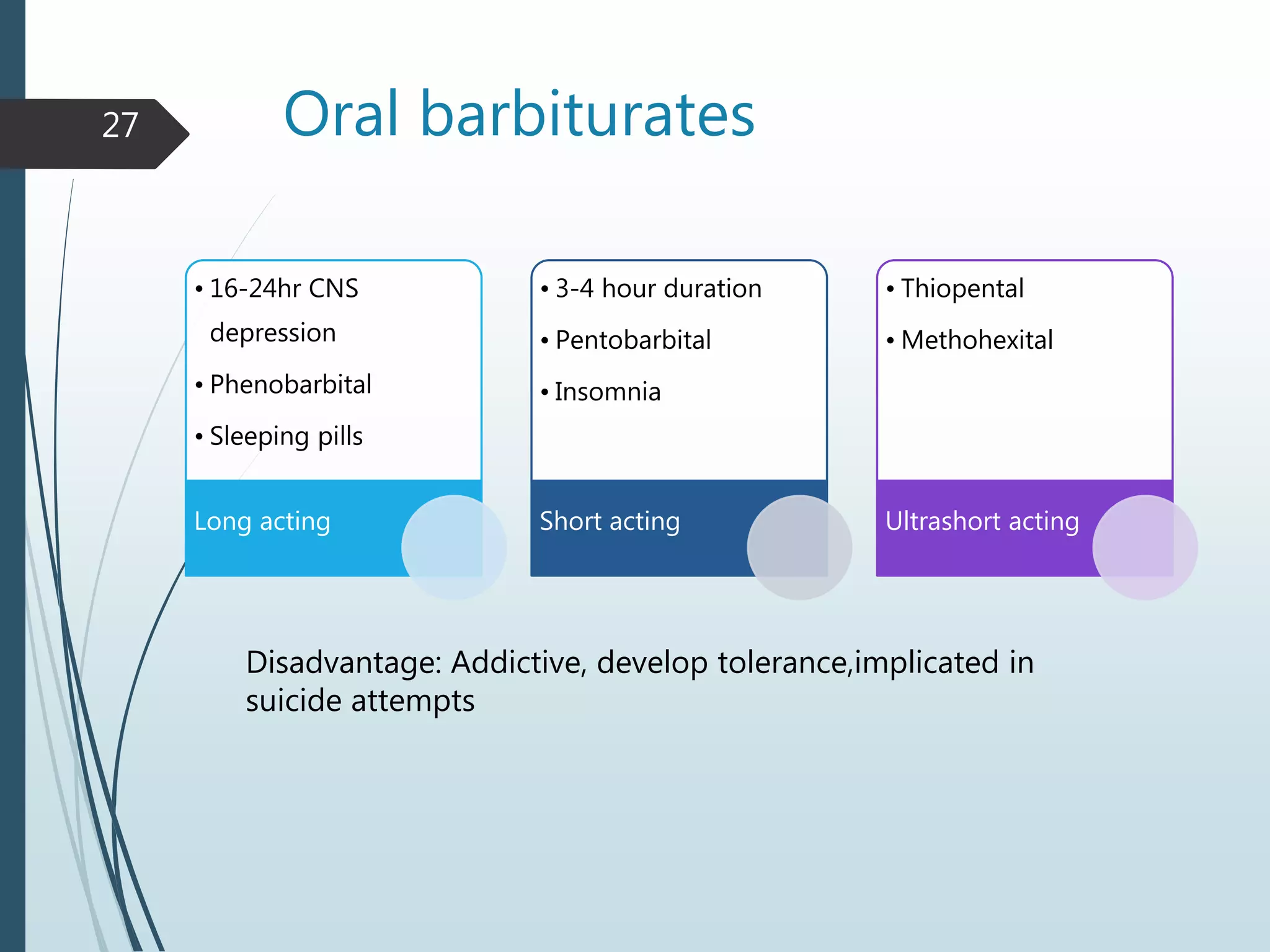
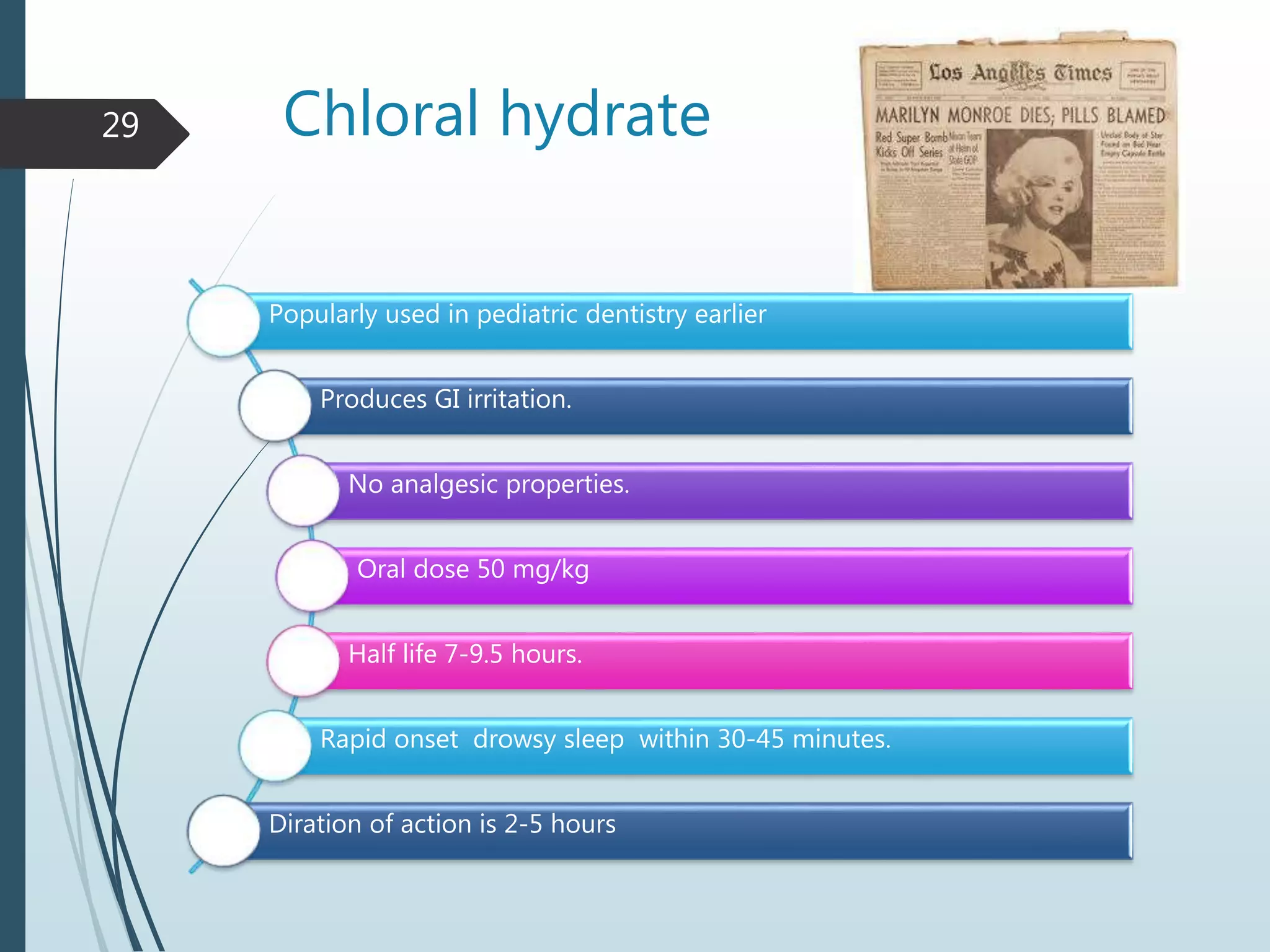
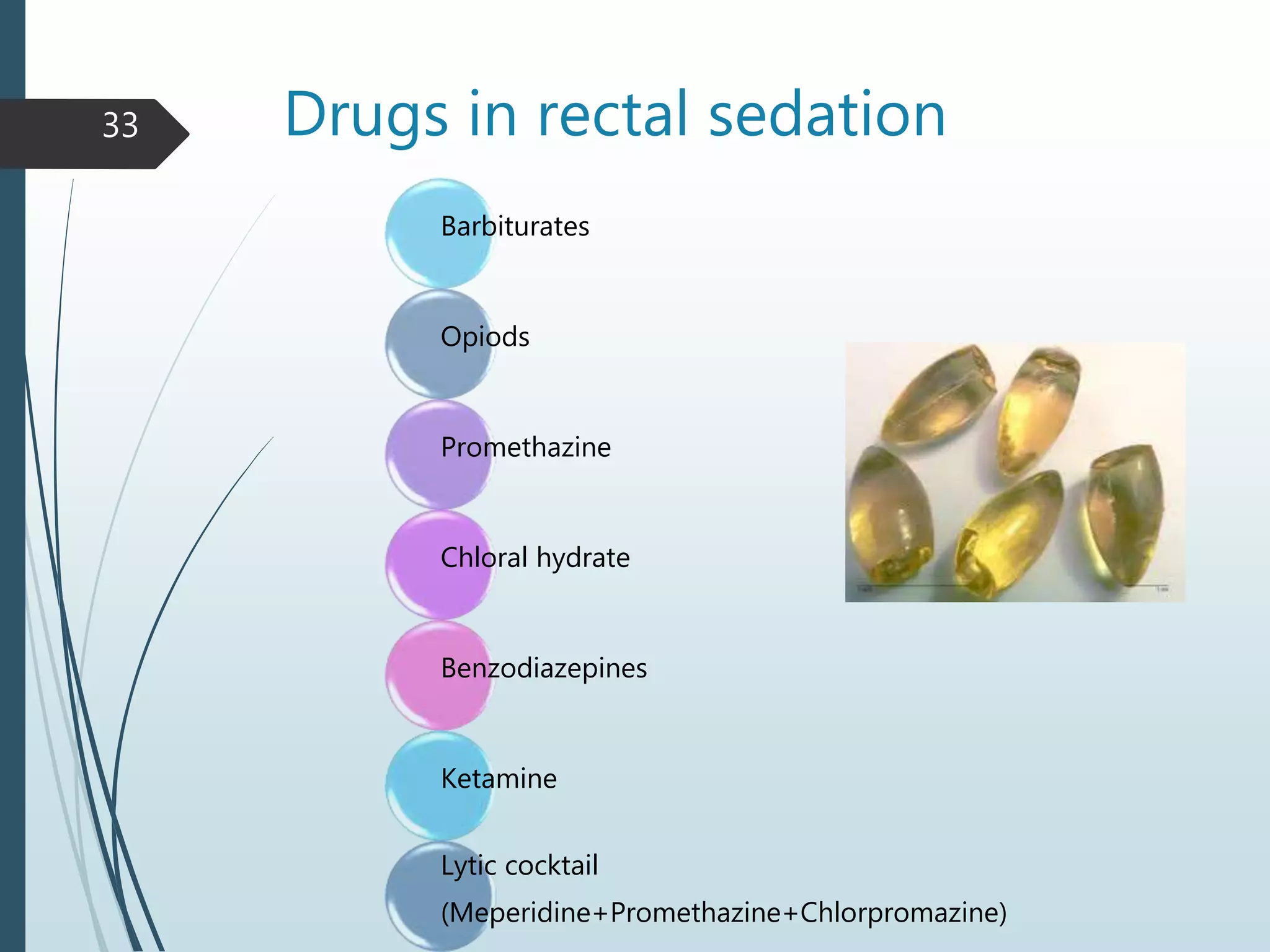
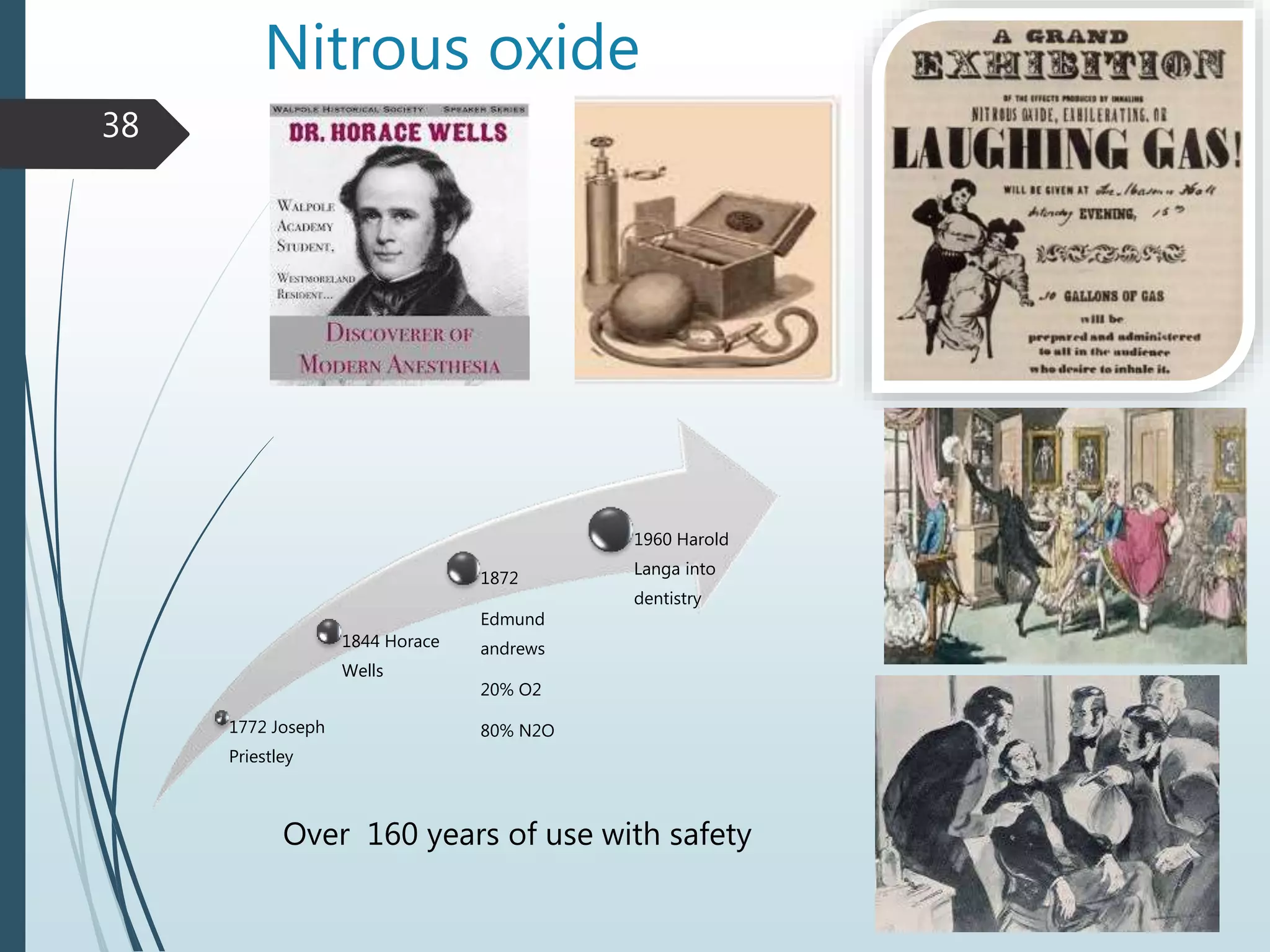
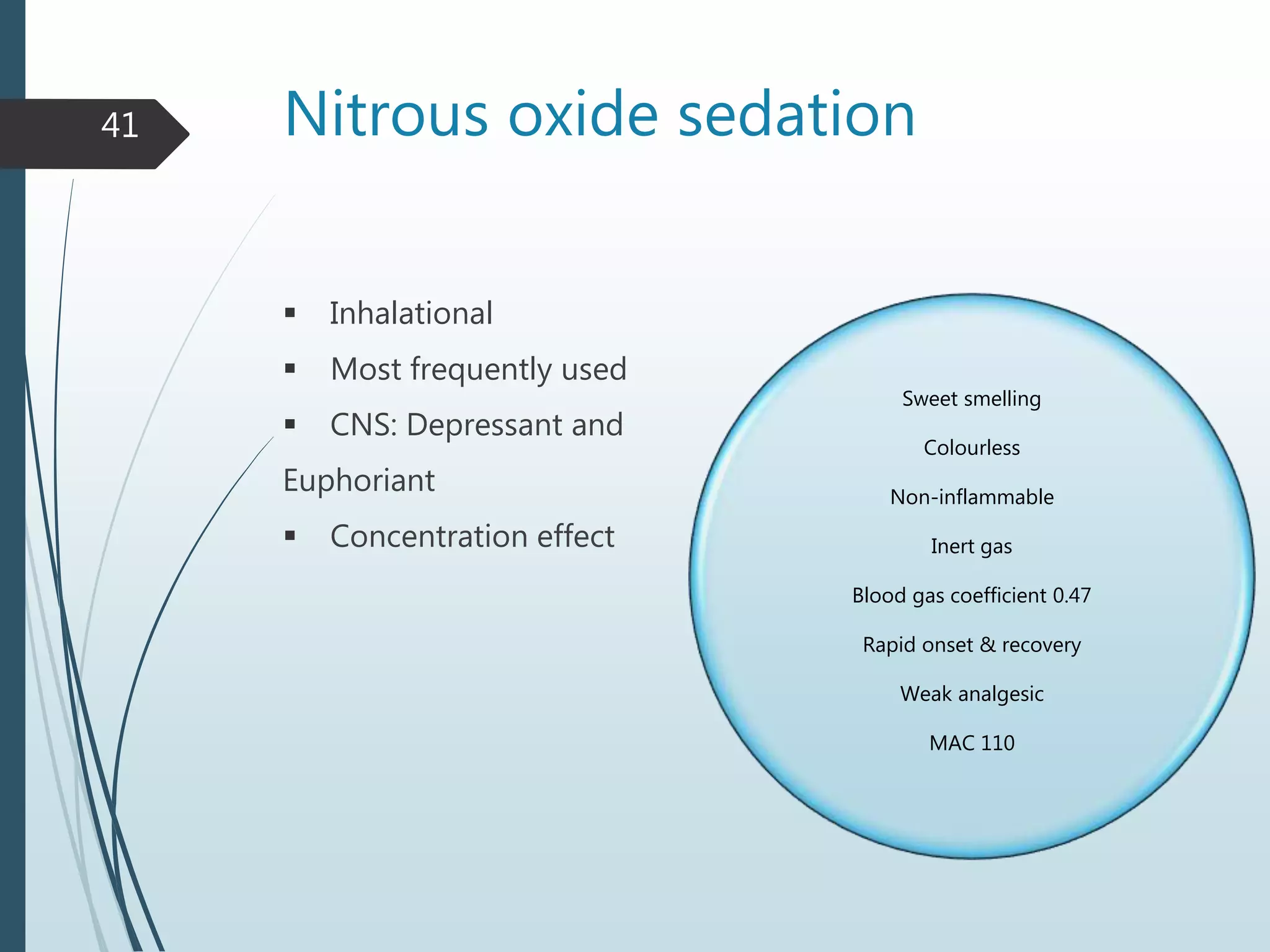
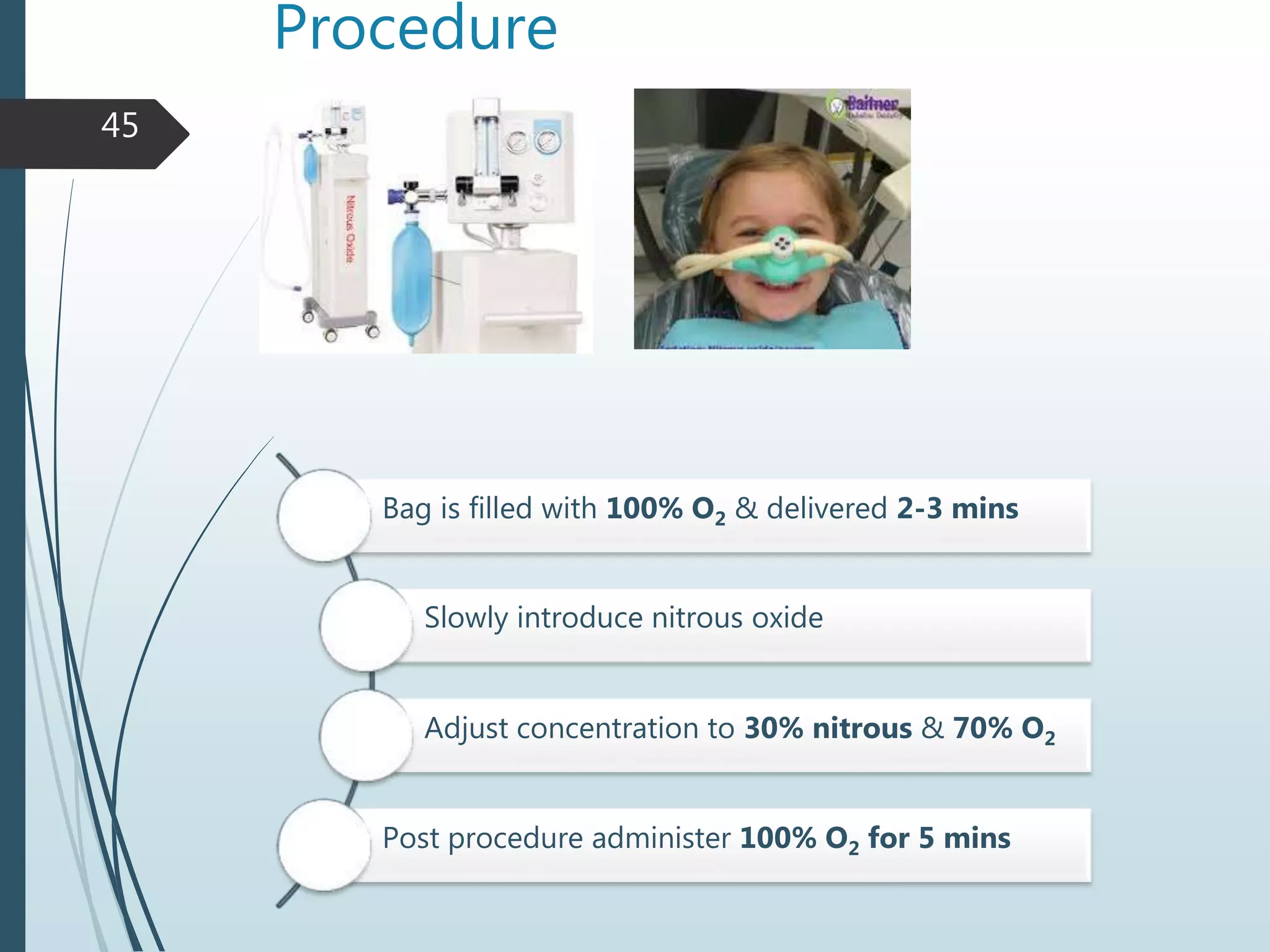
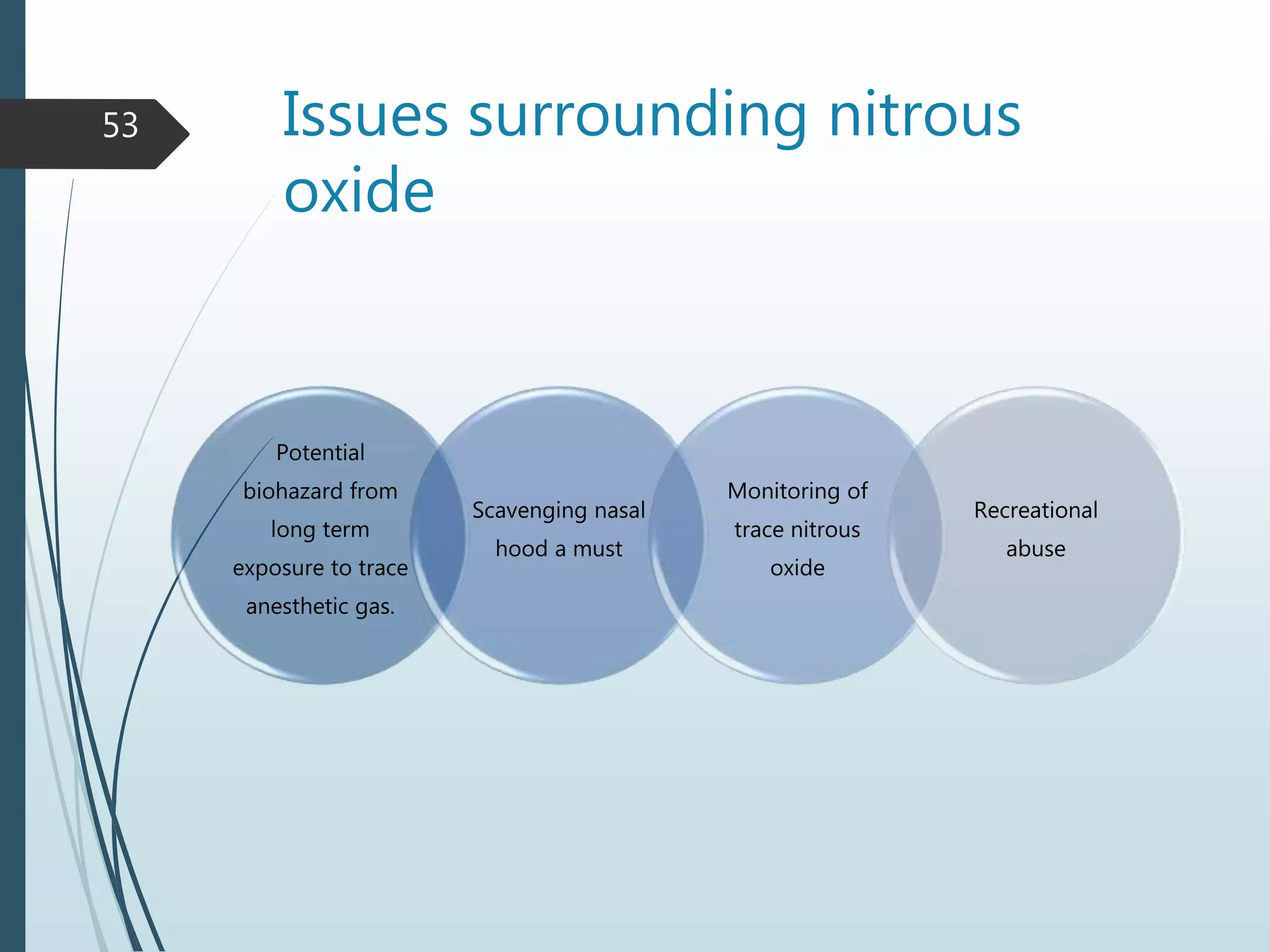
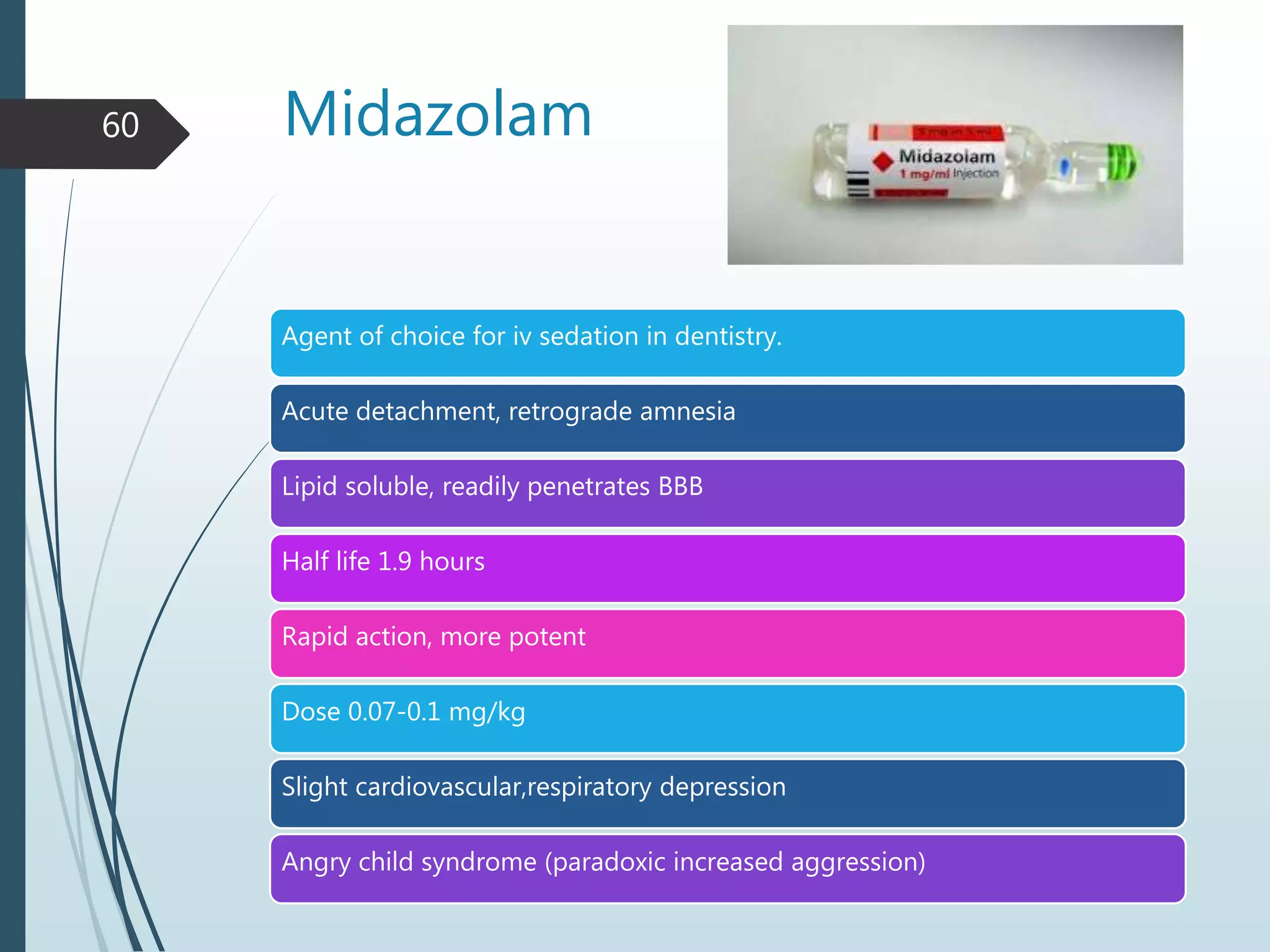
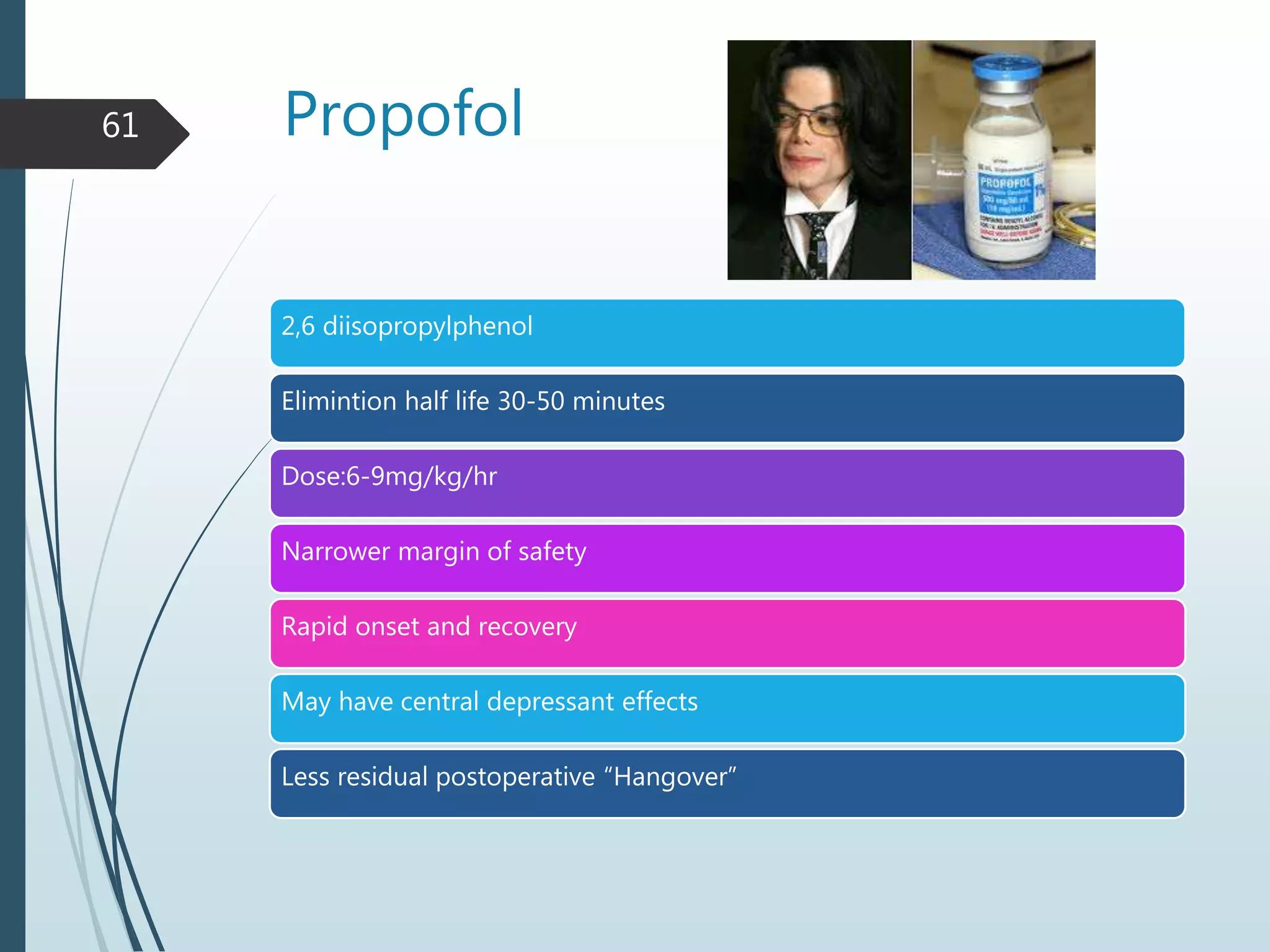
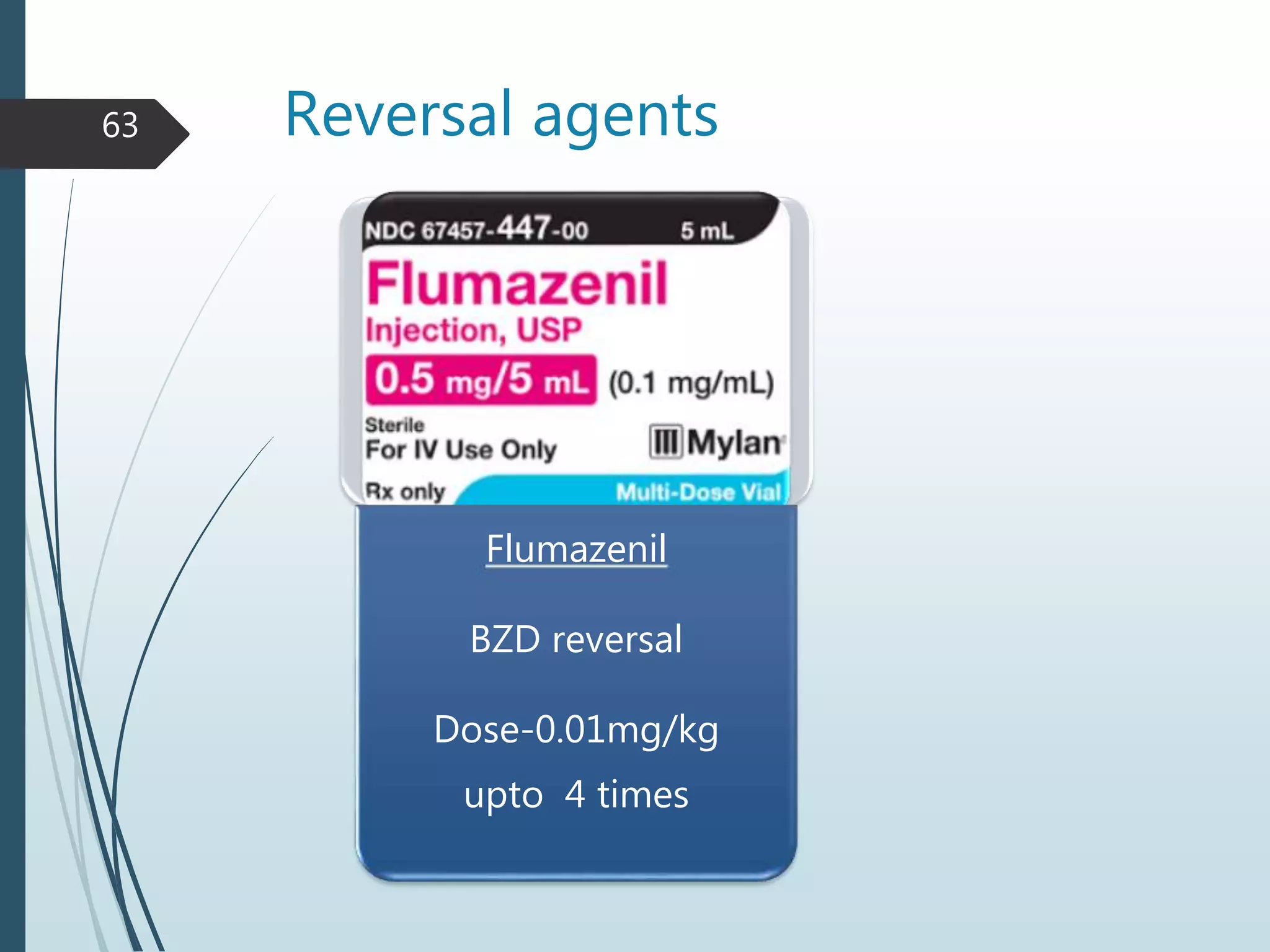
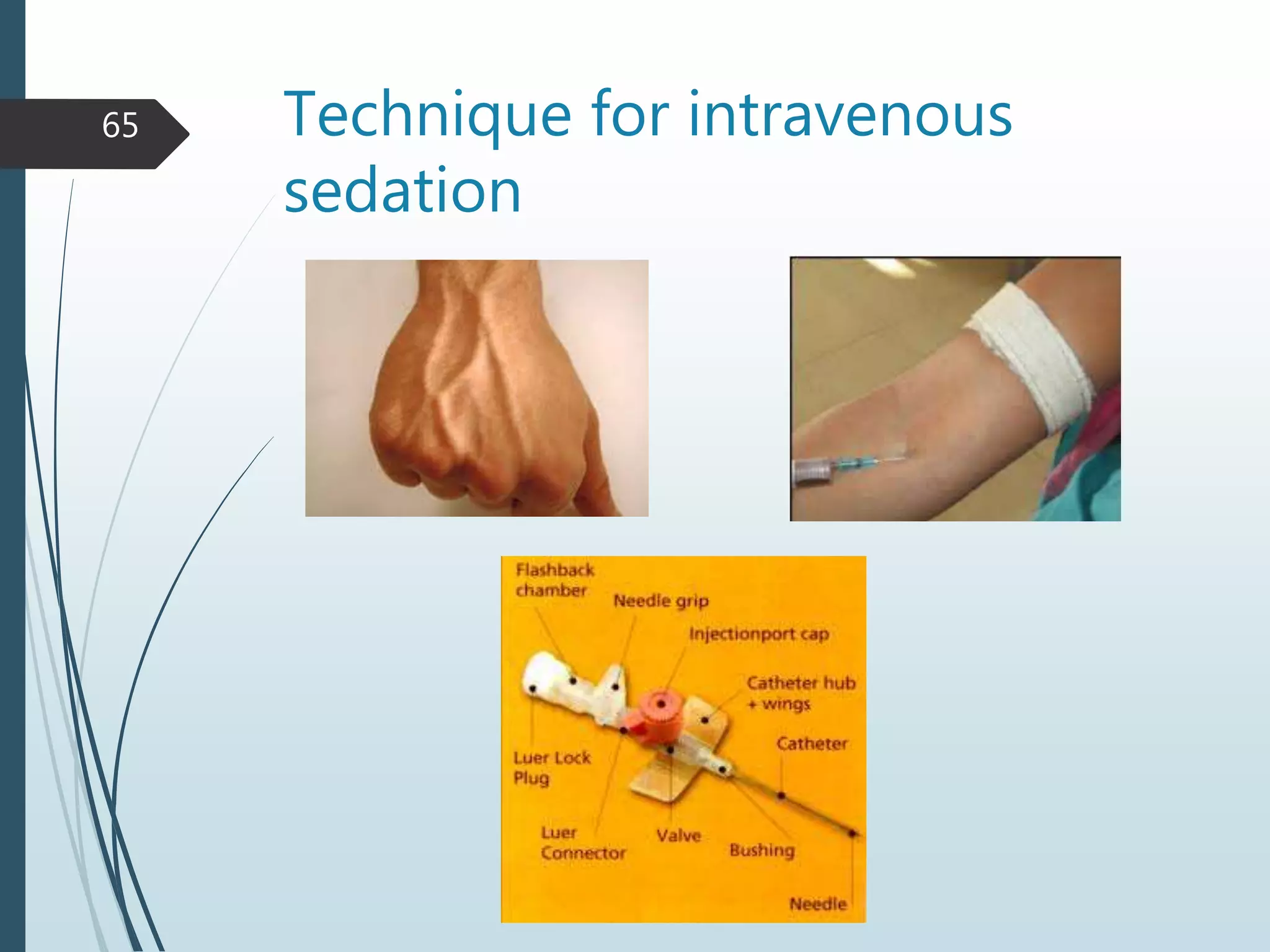
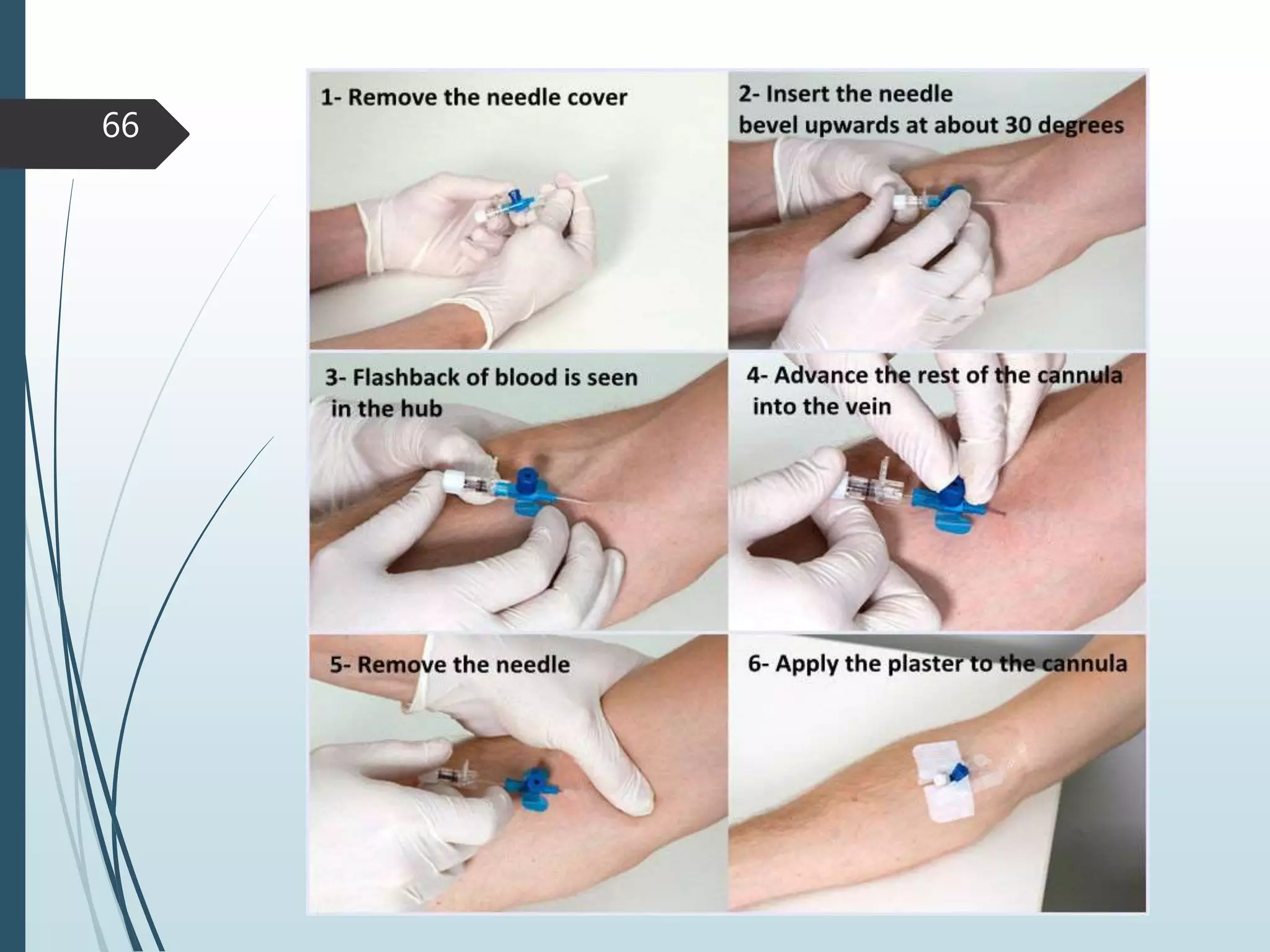
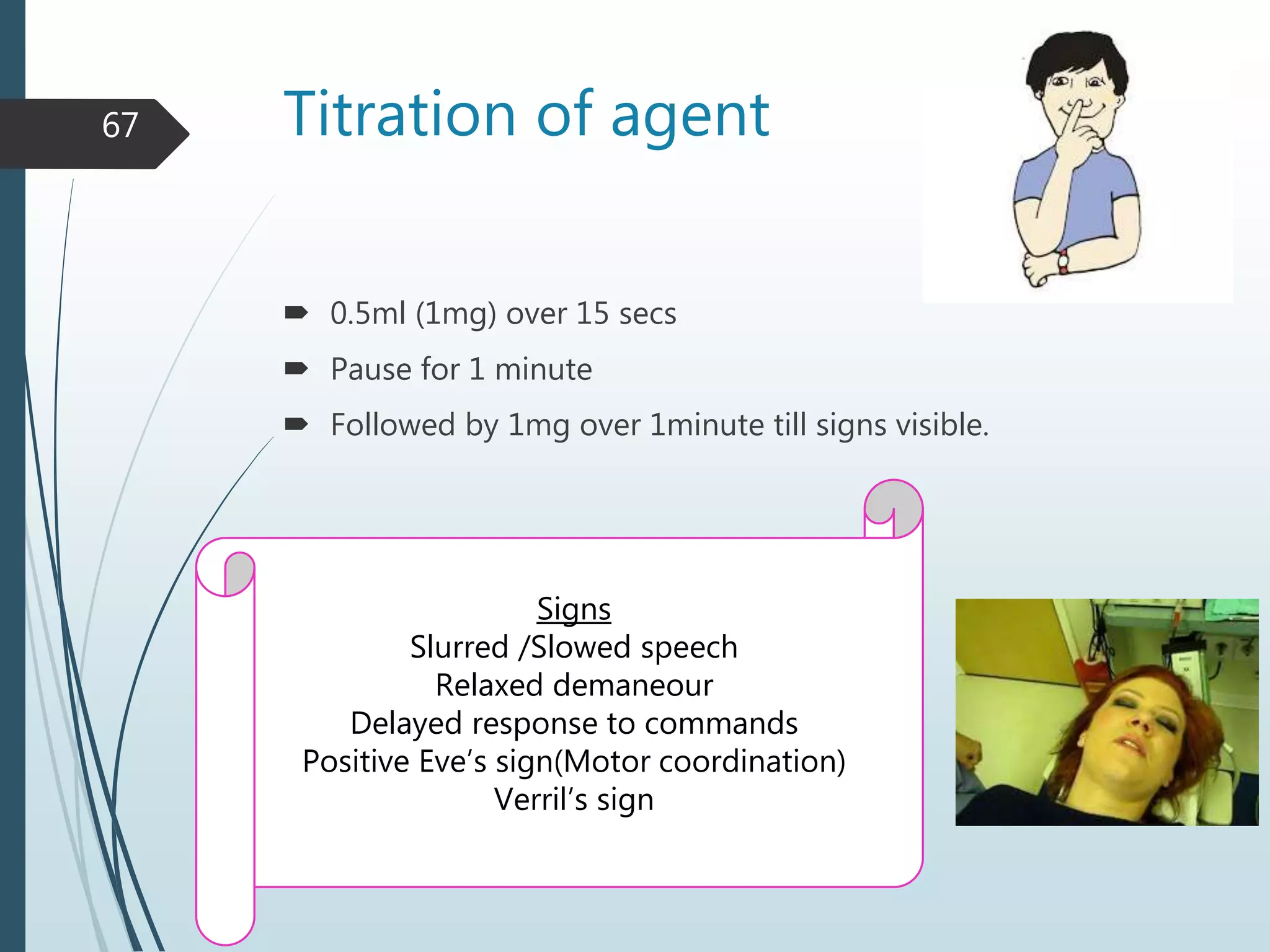
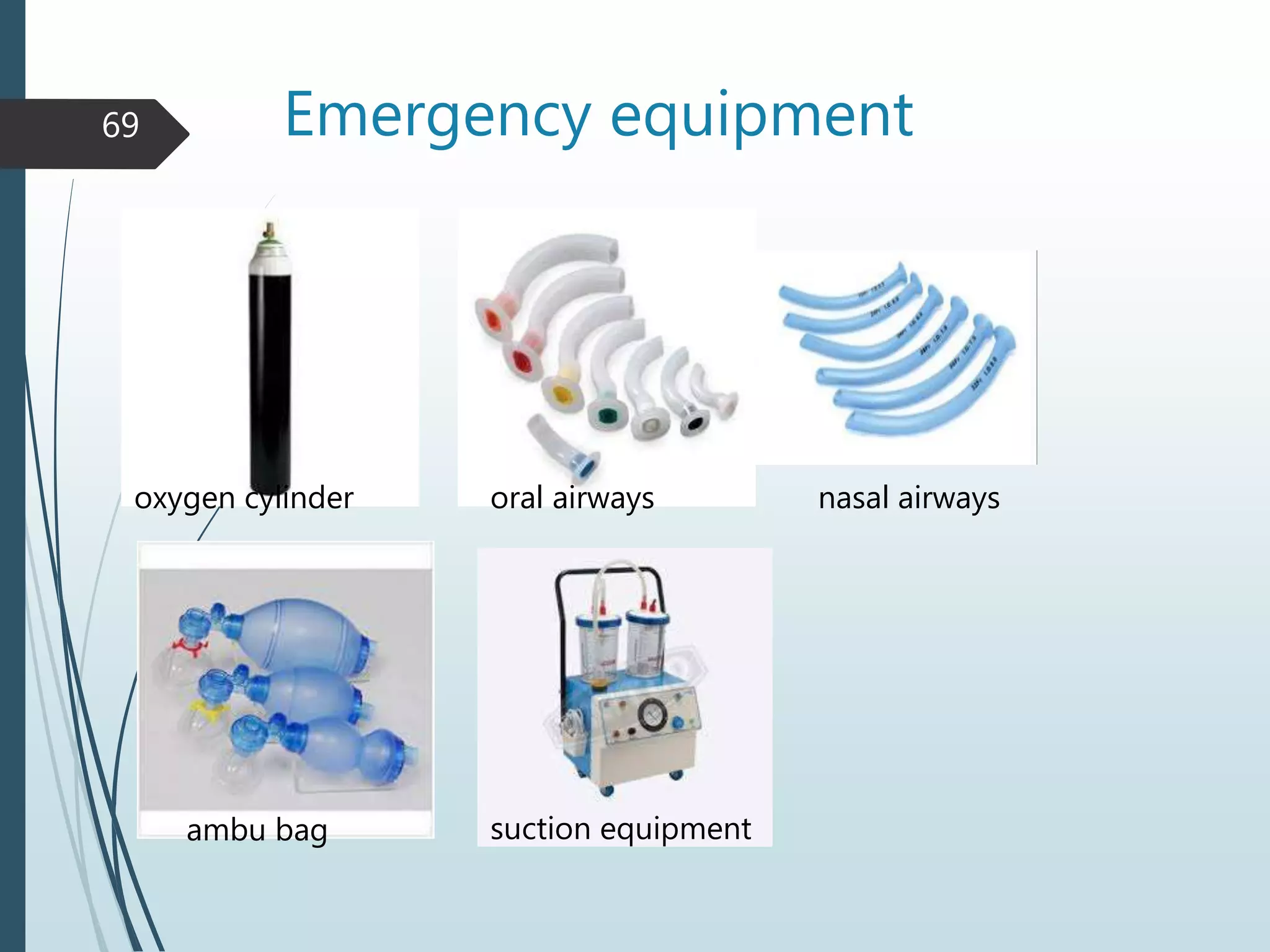
4) Various drugs, routes of administration, and equipment for conscious sedation are described including oral, rectal, inhalational and intramuscular options. Nitrous oxide is a commonly used inhalational agent.