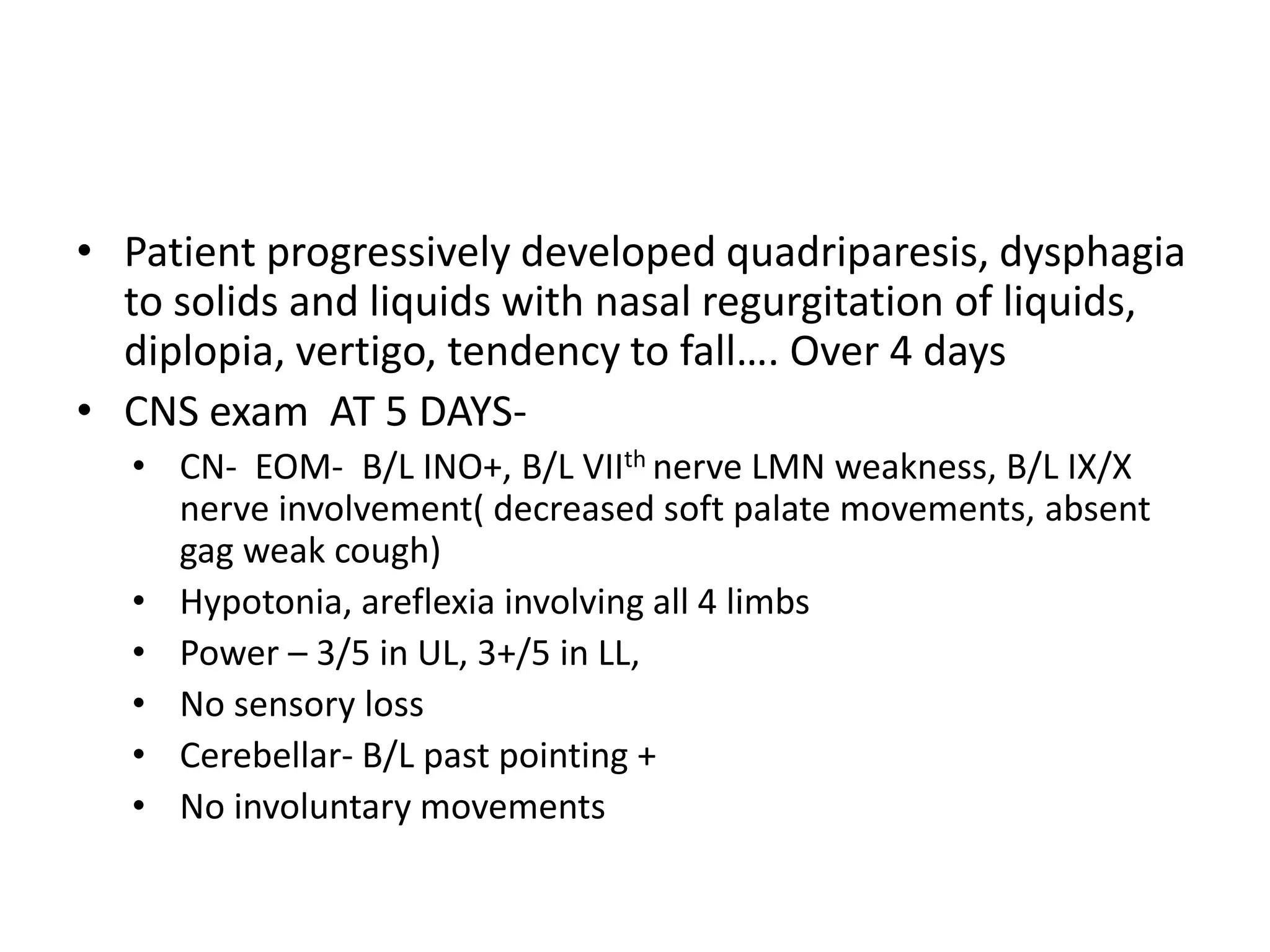
1. The document describes a case of a 26-year-old male presenting with progressive weakness in his right upper limb over 5 years and difficulty walking due to tightness in his right lower limb for 3 months. On examination, he showed signs of Horner's syndrome and LMN weakness in his right upper limb with UMN involvement in his right lower limb.
2. Imaging revealed basilar invagination and syringohydromyelia extending from C2-D9. He was diagnosed with a CV junction anomaly (basilar invagination) with dorsal syringohydromyelia.
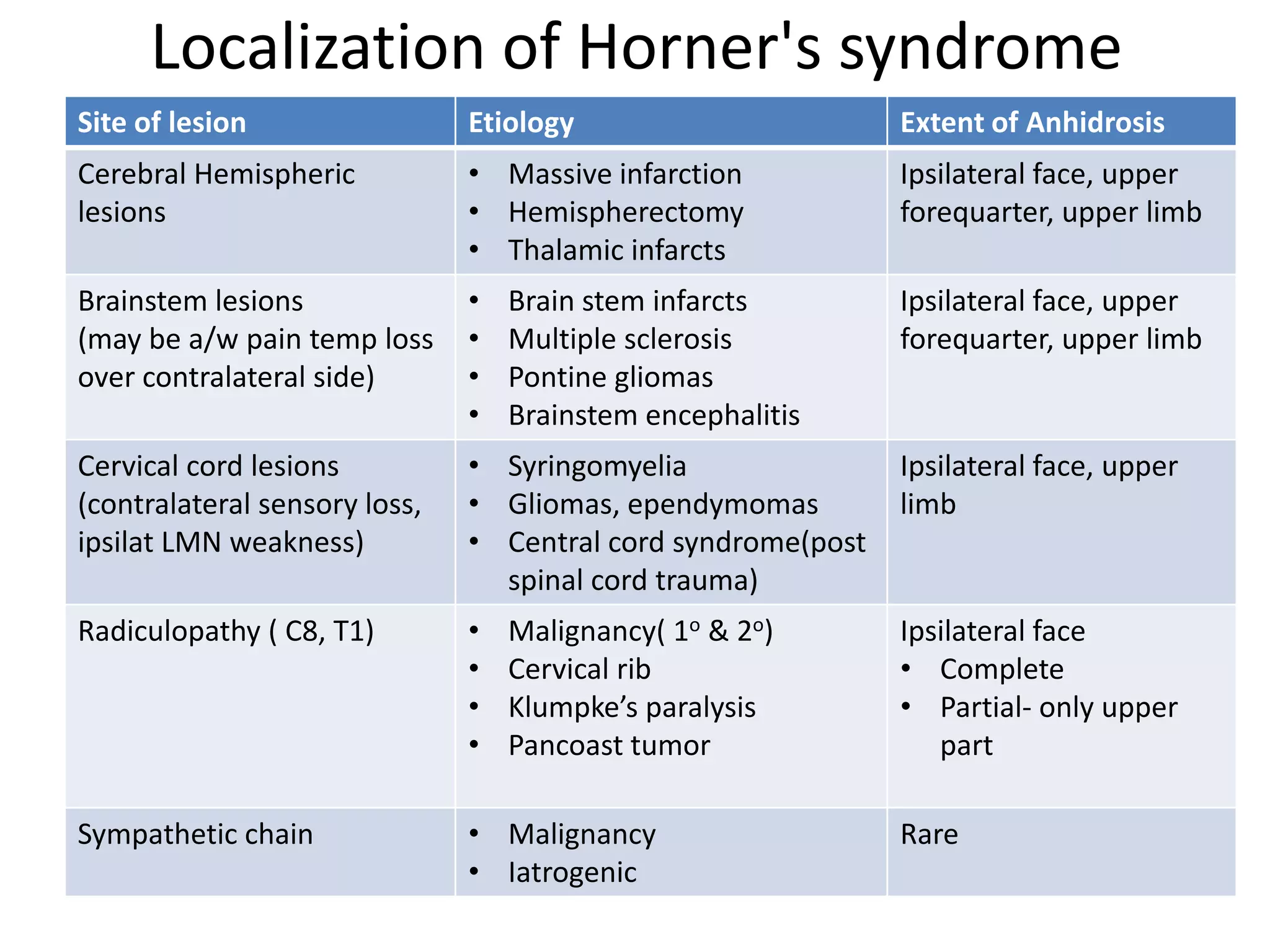
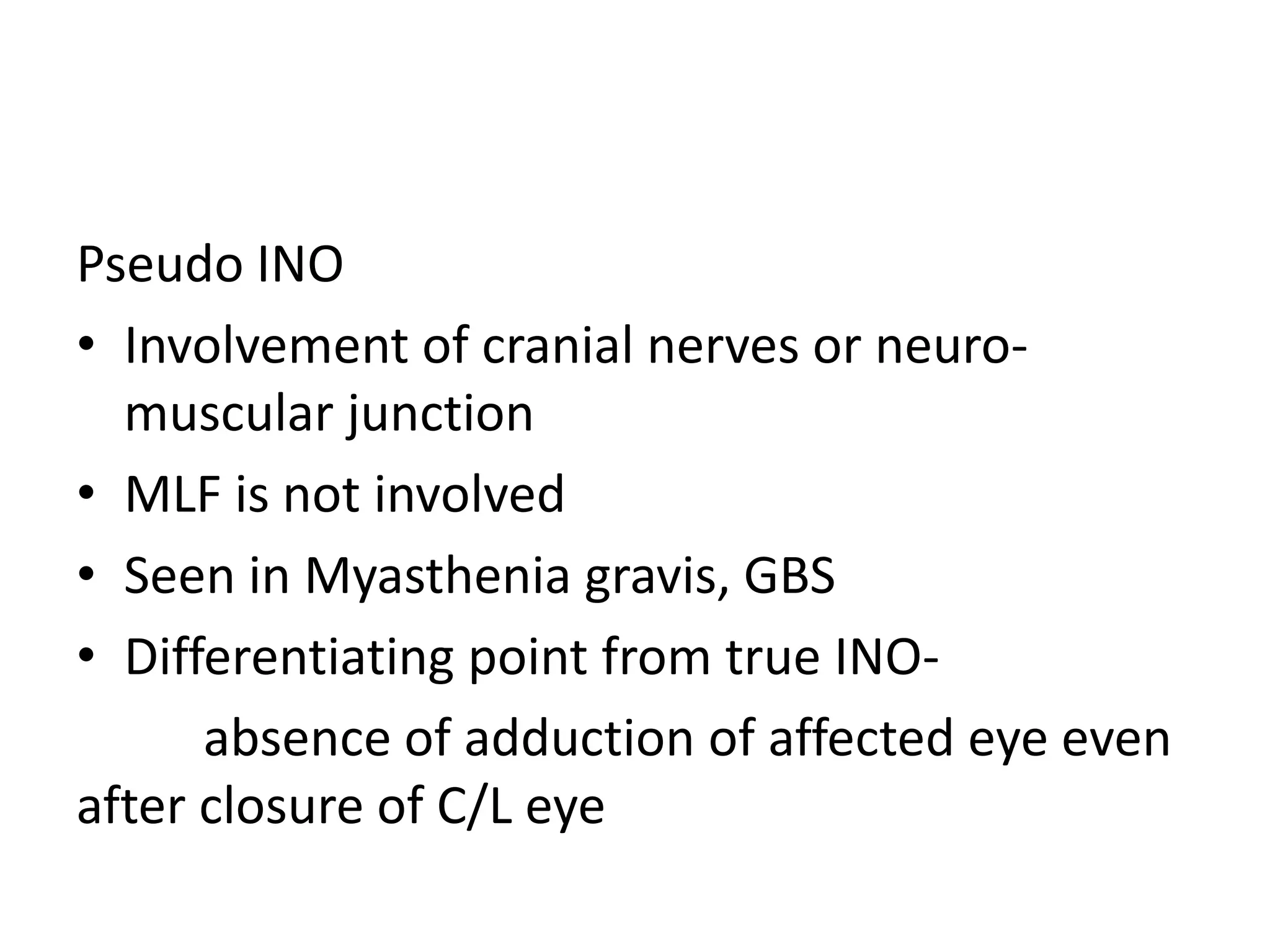
3. The document then discusses Horner's syndrome, its localization, and