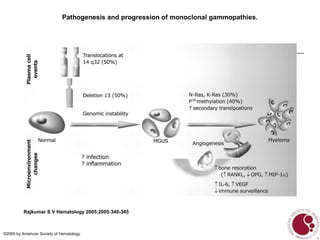
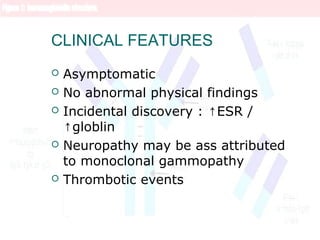
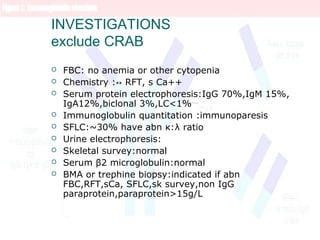
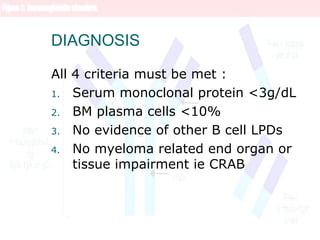
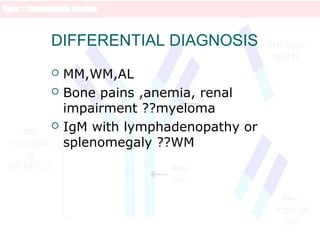
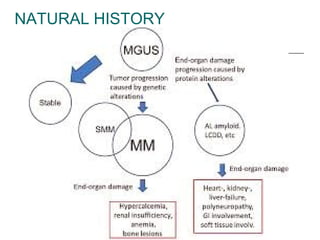
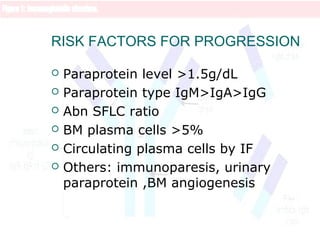
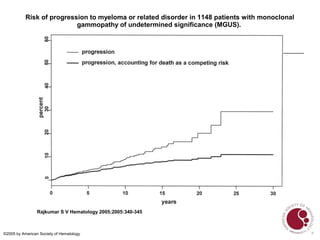
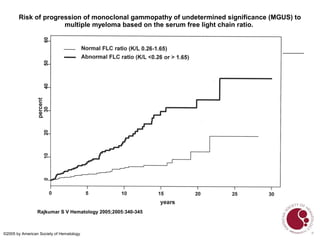
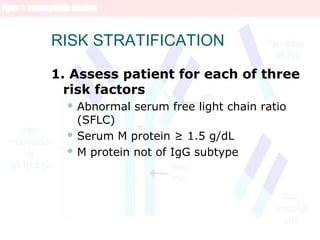
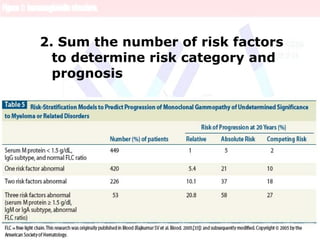
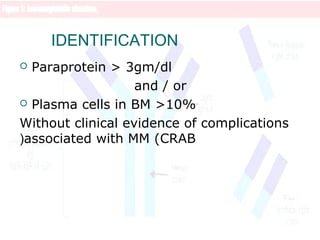
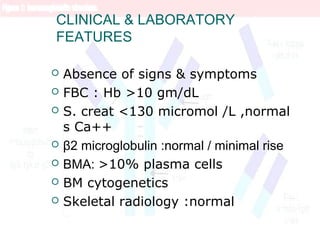
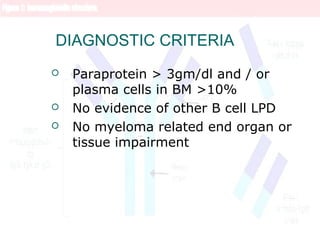
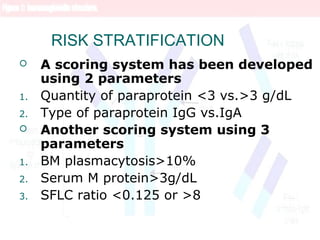
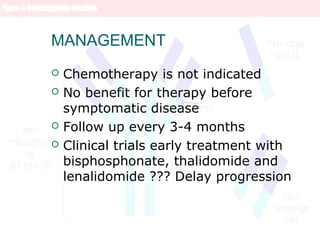
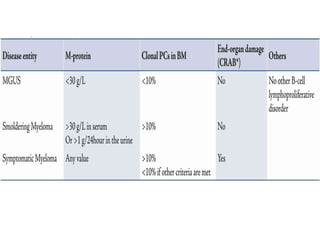
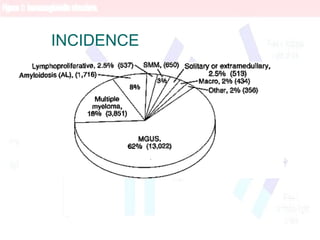
This document discusses monoclonal gammopathy of undetermined significance (MGUS), a premalignant condition characterized by a monoclonal plasma cell proliferation and monoclonal paraprotein in the blood. It describes the incidence, risk factors, pathophysiology, clinical features, investigations, diagnosis, differential diagnosis, natural history, risk factors for progression, risk stratification, and management of MGUS. It also discusses smoldering multiple myeloma, a related condition with a monoclonal paraprotein level >3g/dL and/or >10% plasma cells in the bone marrow without symptoms of multiple myeloma.
![Pathogenesis
Approximately 50% of patients with MGUS and SMM have
primary translocations in the clonal plasma cells
involving the immunoglobulin heavy chain (IgH)
locus on chromosome 14q32 (IgH translocated
MGUS/SMM
The most common partner chromosome loci and genes
dysregulated in these translocations are: [cyclin D1
gene]), [cyclin D3 gene])
Deletion of chromosome 13, a major prognostic factor
in multiple myeloma, is seen in up to 50% of patients
with MGUS by interphase fluorescent in situ
hybridization; hence, the presence of this abnormality
cannot be used to differentiate MGUS from multiple
myeloma](https://image.slidesharecdn.com/paraprotienemia-180316184144/85/Paraprotienemia-7-320.jpg)