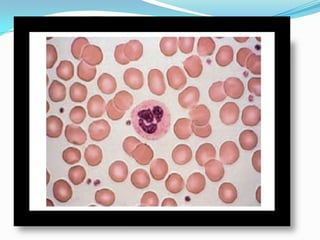
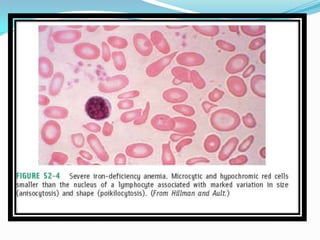
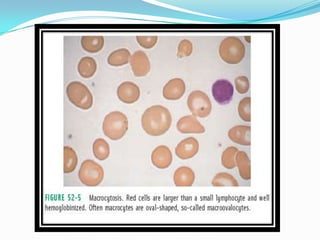
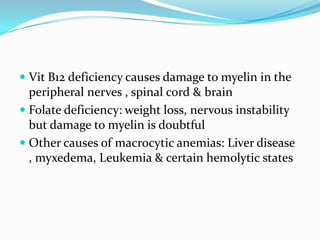
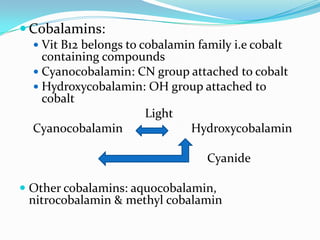
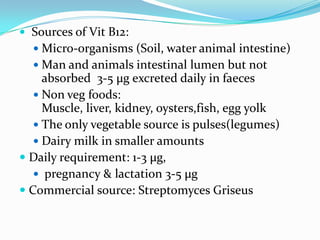
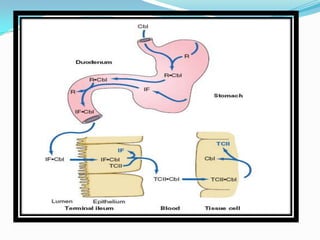
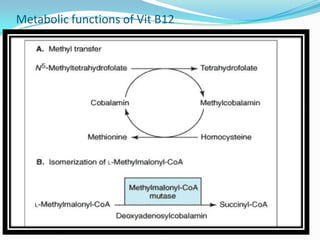
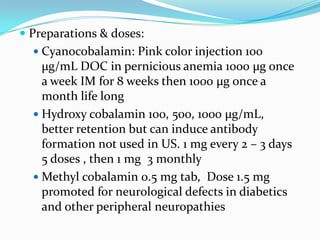
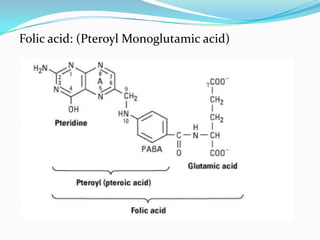
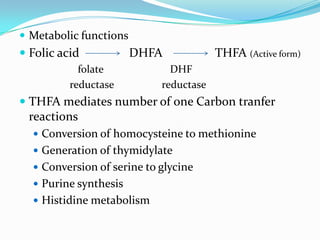
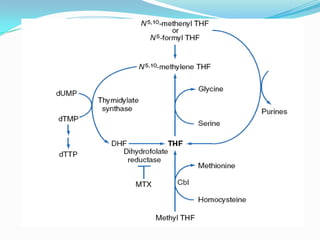
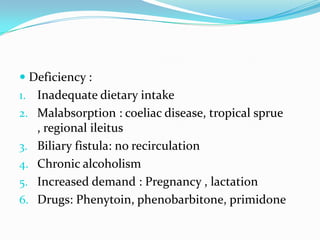
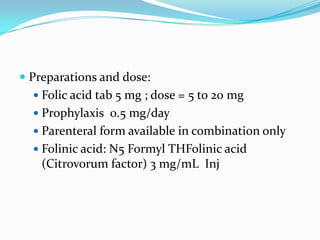
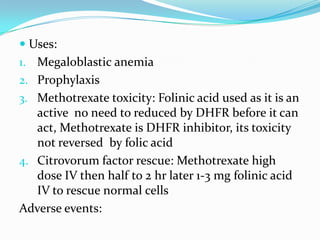
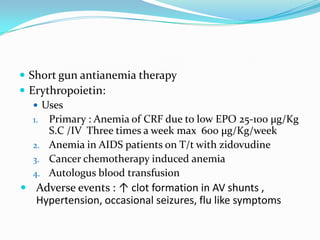
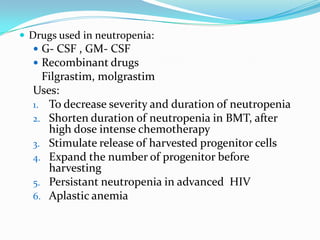
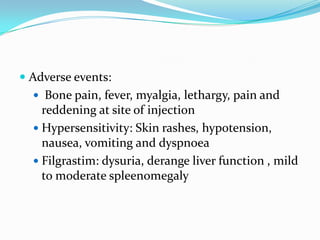
This document discusses megaloblastic anemia, its causes, symptoms, and treatments. It is characterized by abnormally large red blood cells due to a deficiency in vitamin B12 or folic acid, which is needed for DNA synthesis. The deficiencies can result from inadequate intake, malabsorption, or increased demand. Treatments include injections or supplements of vitamin B12, folic acid, or erythropoietin to stimulate red blood cell production. Adverse reactions are also discussed.