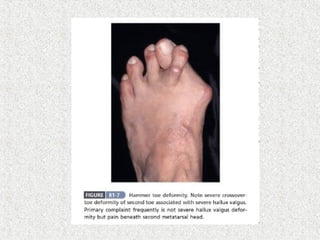
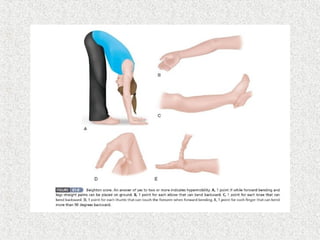
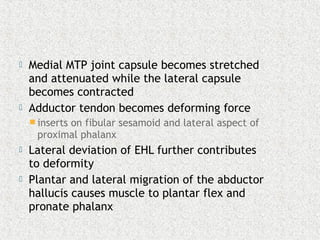
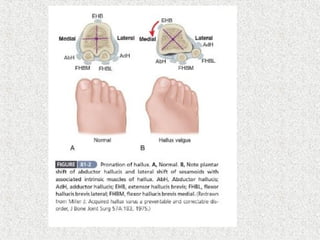
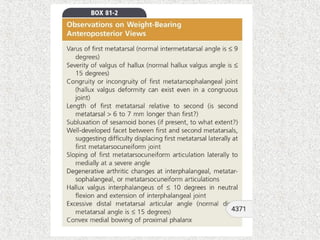
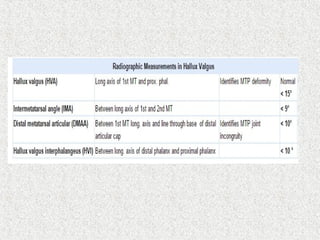
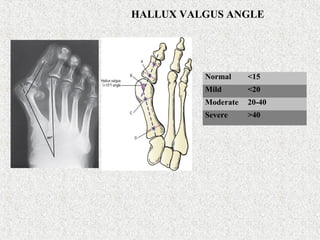
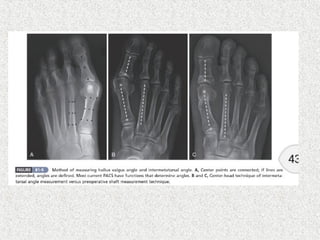
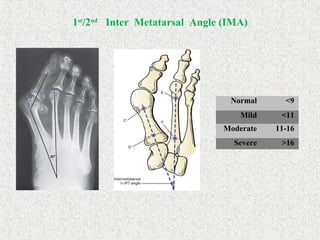
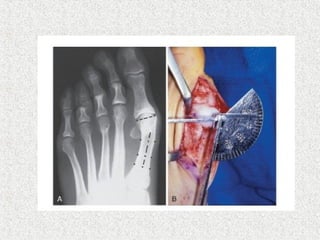
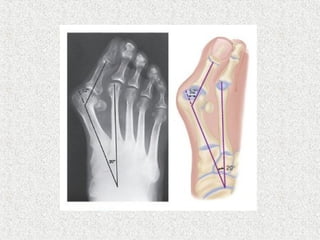
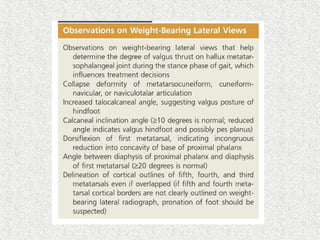
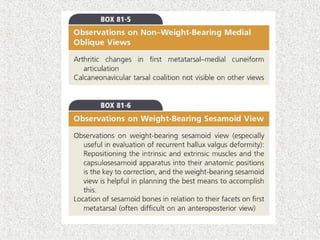
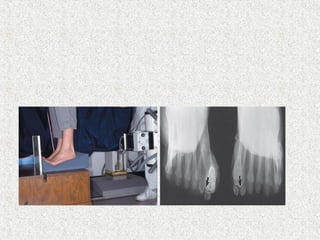
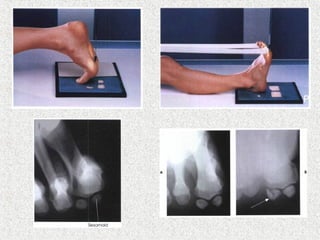
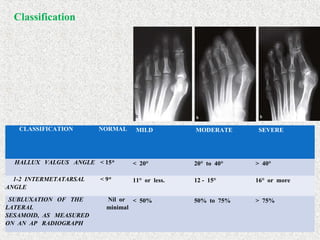
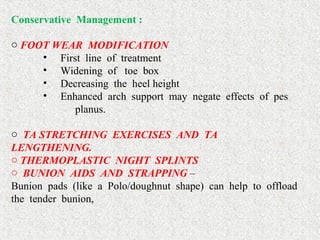
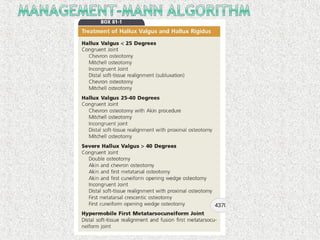
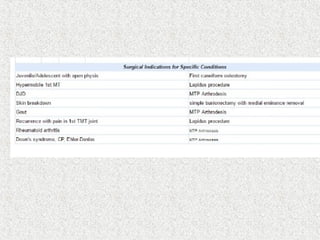
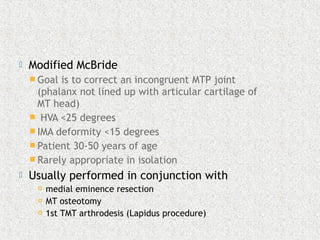
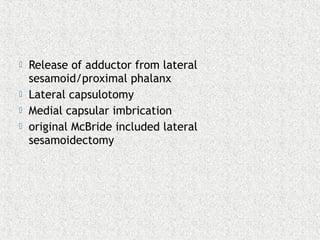
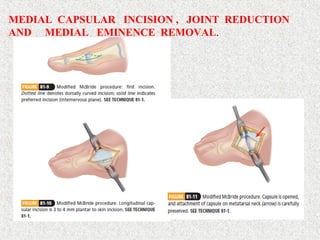
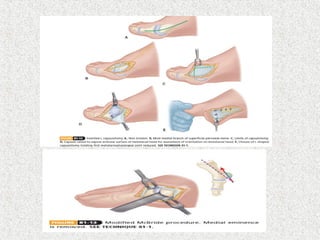
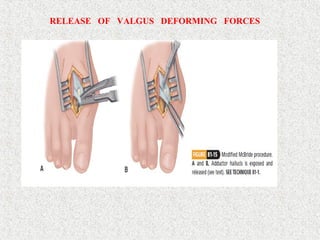
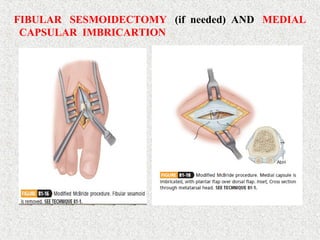
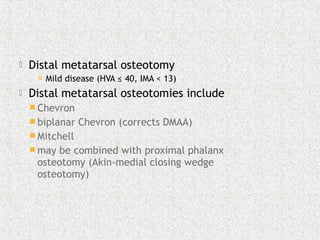
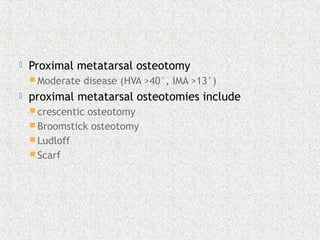
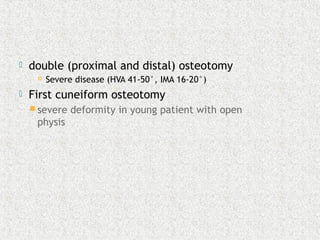
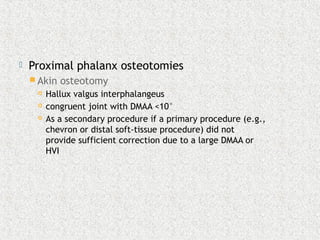
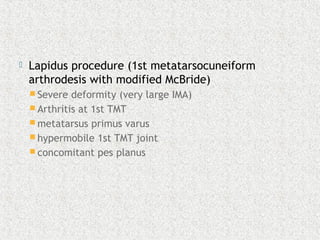
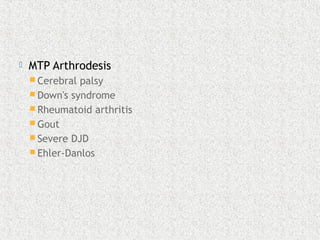
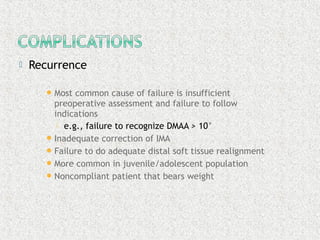
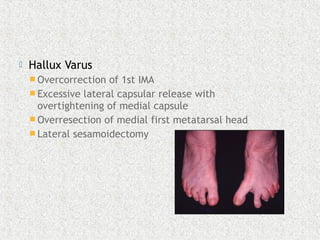
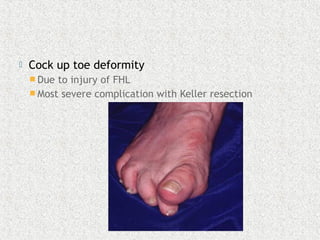
This document discusses hallux valgus, also known as a bunion. It begins by defining the deformity and listing associated symptoms. It then discusses causes, classifications based on x-ray measurements, conservative and surgical treatment options. For surgery, it explains various procedures that can be used to correct deformities ranging from mild to severe, including soft tissue releases, osteotomies of the metatarsal and phalanx bones, and arthrodesis or fusion procedures. Potential complications of surgery are also outlined.