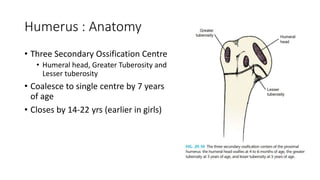
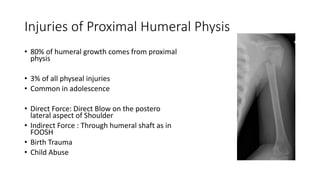
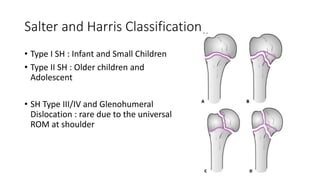
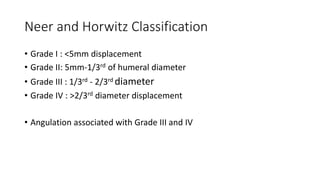
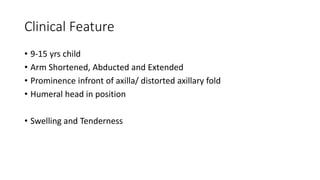
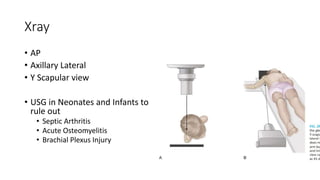
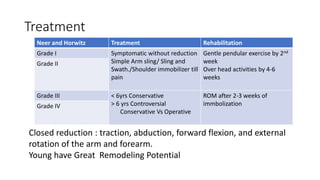
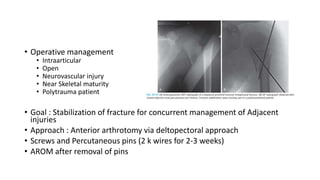
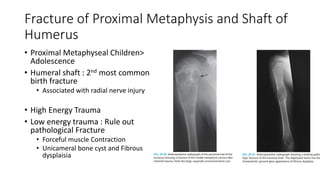
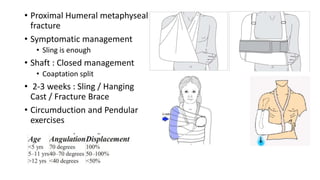
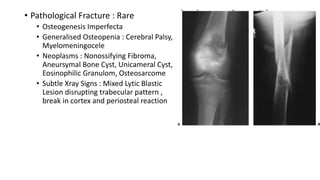
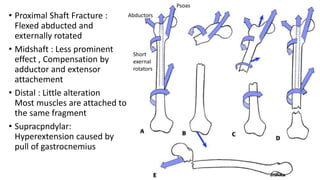
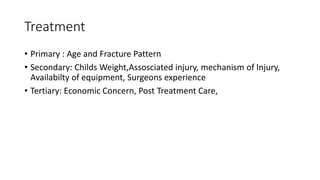
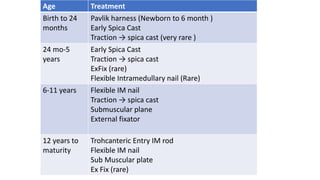
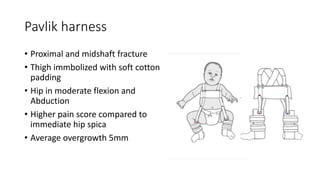
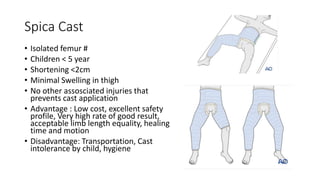
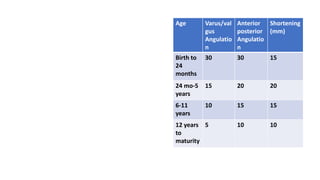
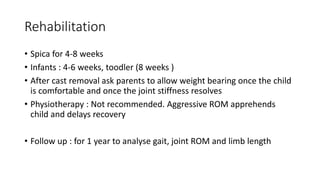
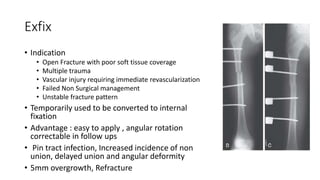
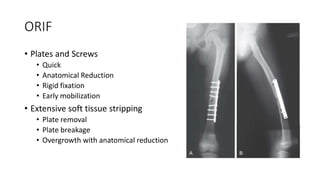
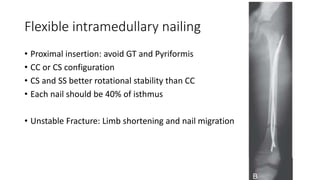
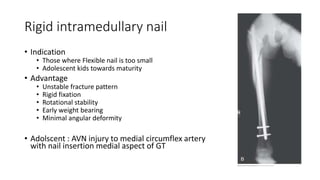
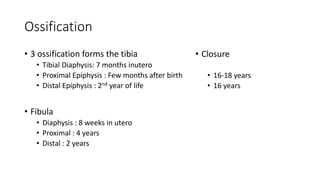
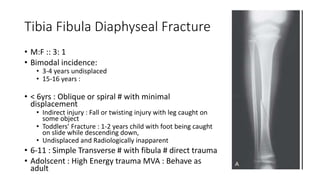
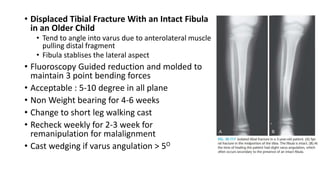
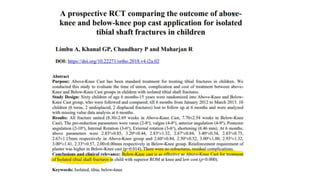
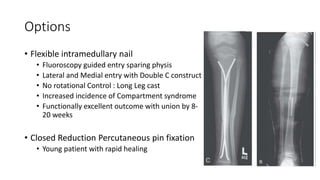
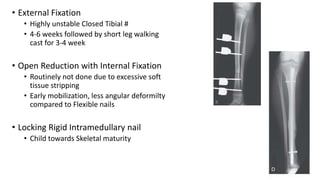
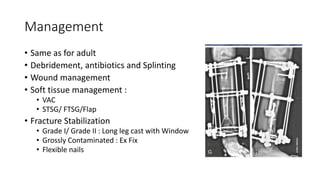
The document presents a comprehensive overview of pediatric long bone fractures, emphasizing humeral, femoral, and tibial injuries, their classifications, mechanisms of injury, diagnostic methods, and treatment options. It highlights the importance of age and fracture patterns in treatment decisions and discusses the potential for remodeling in younger patients. Various management strategies, including conservative and operative approaches, are outlined, along with complications and outcomes associated with these fractures.