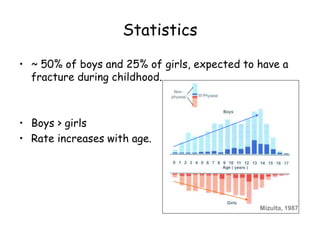
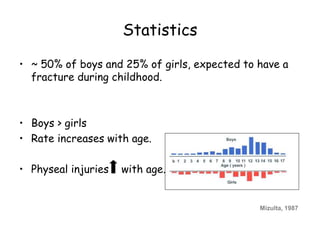
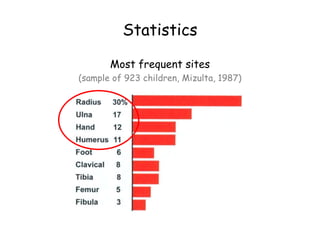
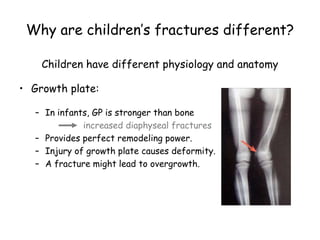
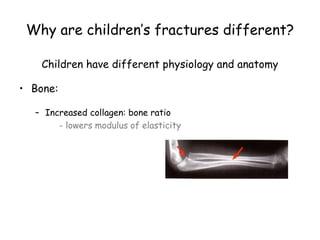
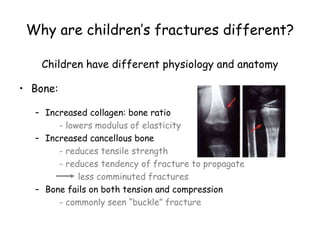
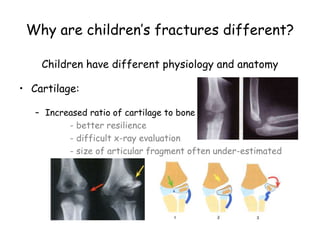
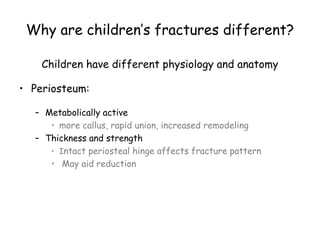
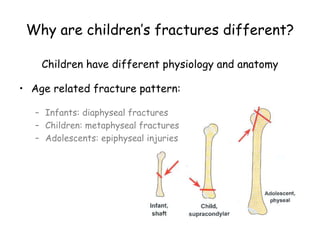
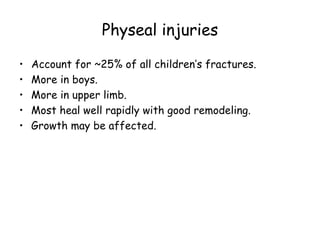
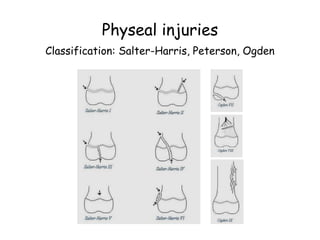
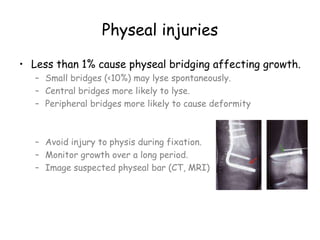
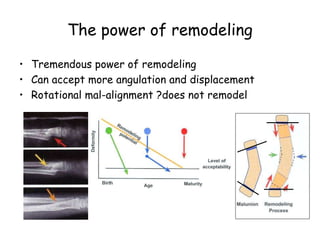
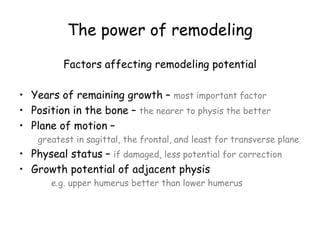
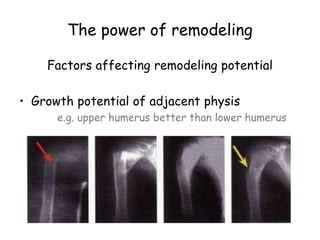
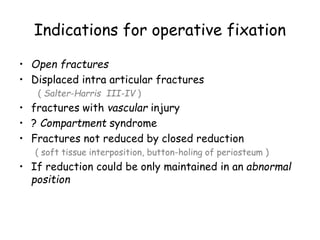
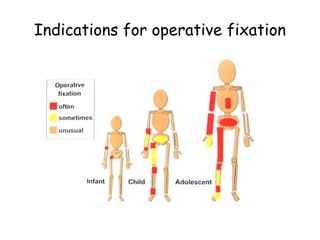
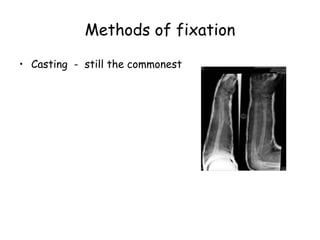
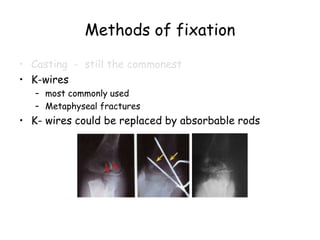
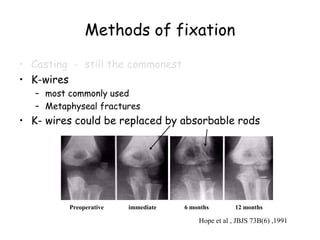
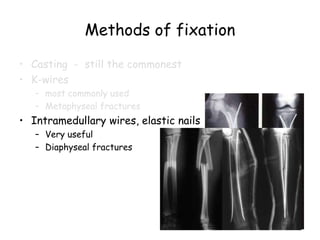
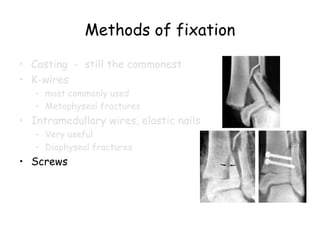
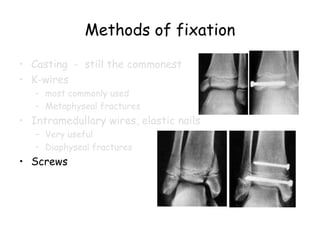
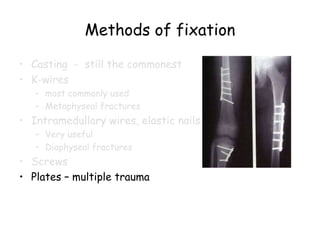
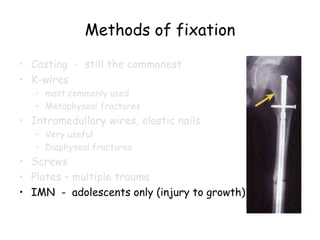
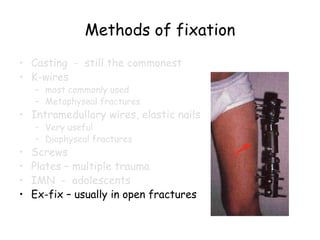
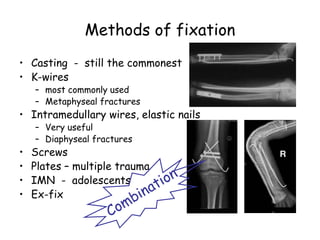
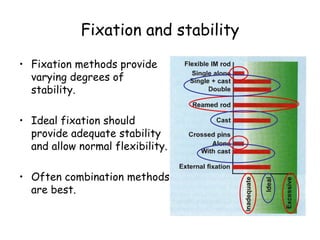
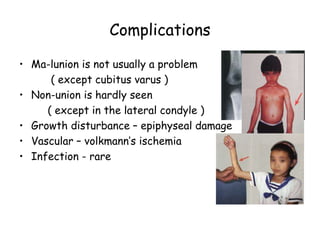
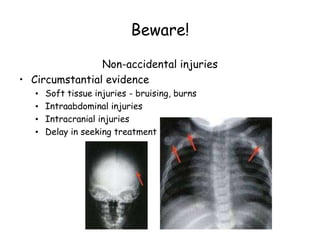
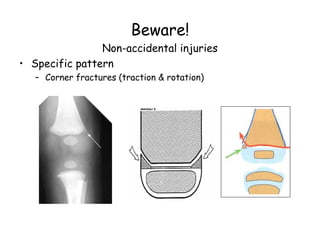
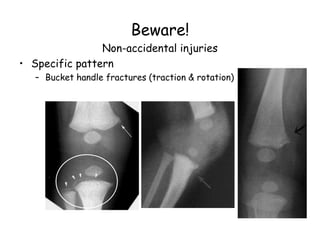
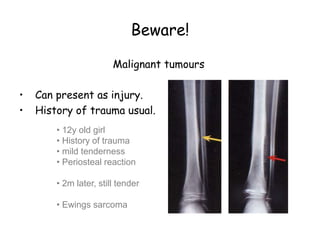
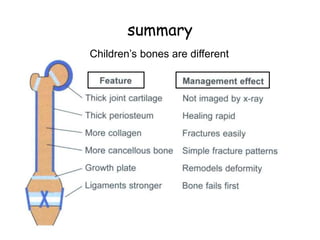
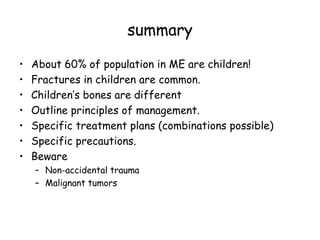
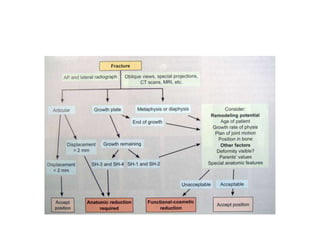
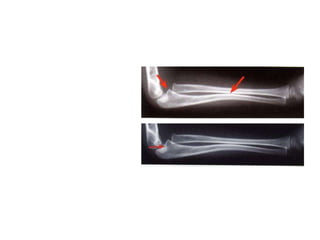
Fractures are common in children, accounting for about 15% of injuries. Children's bones differ from adults' due to factors like growth plates and increased remodeling potential. Principles of management include restoring alignment while allowing healing and growth. Common treatment plans involve casting, K-wires, elastic nails or screws. Precautions are needed for physeal injuries, non-accidental trauma, and rare tumors that can mimic fractures.