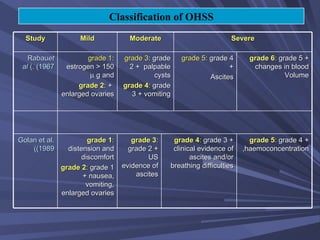
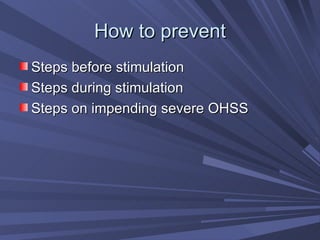
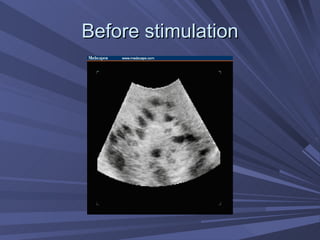
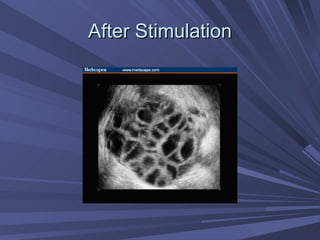
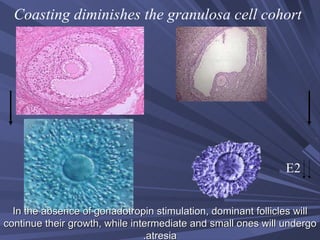
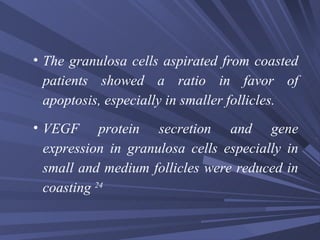
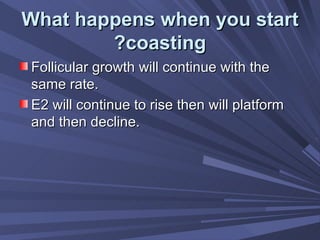
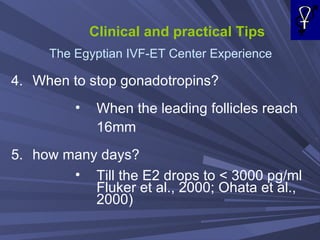
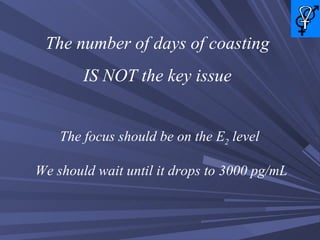
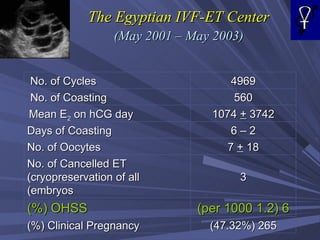
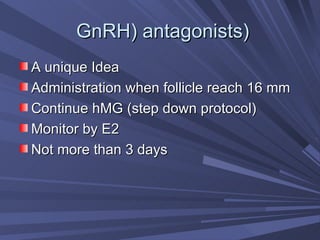
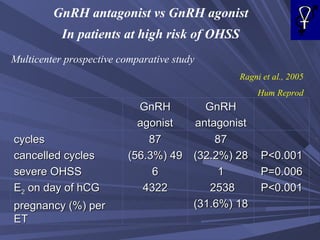
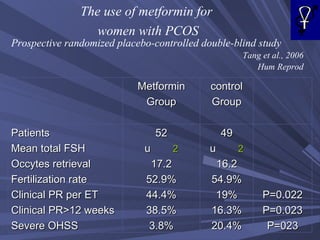
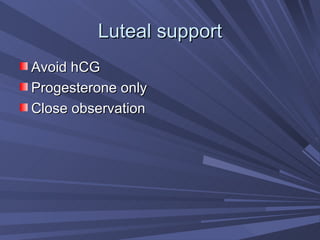
Ovarian hyperstimulation syndrome (OHSS) is an iatrogenic condition caused by fertility treatments. It can range from mild to life-threatening. Steps to prevent OHSS include identifying at-risk patients, using low gonadotropin doses, coasting by withholding gonadotropins to lower estrogen levels safely, using GnRH antagonists, and administering metformin. If OHSS occurs, management focuses on investigations, fluid monitoring, and paracentesis if needed.