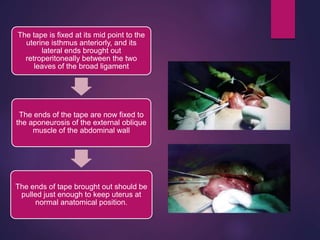
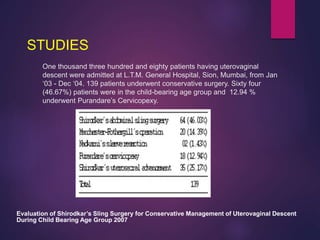
The document discusses Purandare's cervicopexy, a surgical procedure developed by Dr. B. N. Purandare for treating uterine prolapse, which has significantly influenced conservative surgery methods. The text outlines the prevalence, etiology, management options, surgical techniques, postoperative care, and potential complications related to the procedure. It also highlights studies and outcomes associated with cervicopexy surgeries performed at various hospitals in India.












![RESTORATIVE SURGERIES
• COLPORRHAPHY ( ANTERIOR/ POSTERIOR)
• FOTHERGILL’S REPAIR (MANCHESTER OPERATION)
• SHIRODKAR’S PROCEDURE
• ABDOMINAL SLING OPERATION
• A) ABDOMINOCERVICOPEXY
PURANDARE’S CERVICOPEXY
• B) SHIRODKAR’S ABDOMINAL SLING OPERATION
• C) KHANNA’S ABDOMINAL SLING OPERATION
D) VIRKUD’S COMPOSITE SLING
E)OTHERS [ SOONAWALA/ VIVEK JOSHI’S ]
• LAPAROSCOPIC SLING SURGERY](https://image.slidesharecdn.com/purandarescervicopexy-180119155546/85/Purandares-cervicopexy-14-320.jpg)