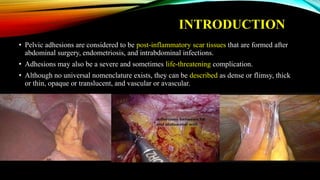
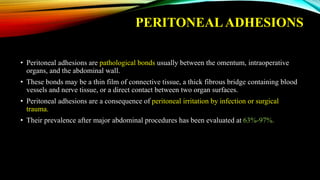
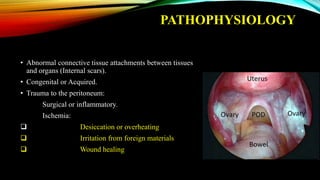
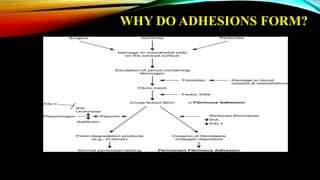
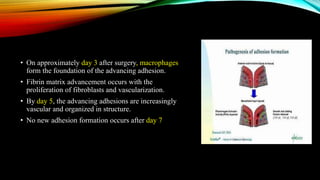
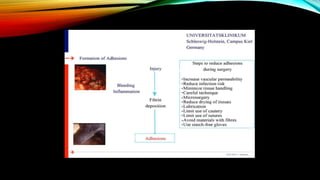
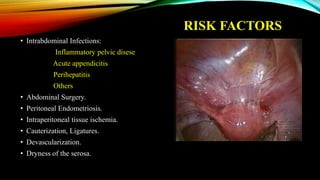
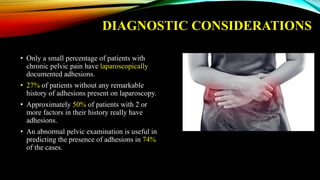
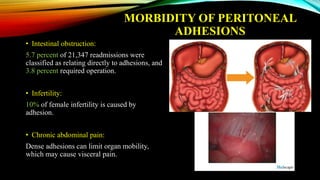
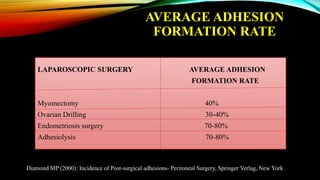
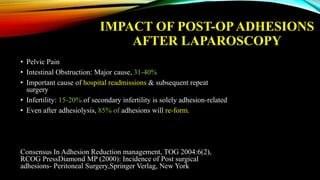
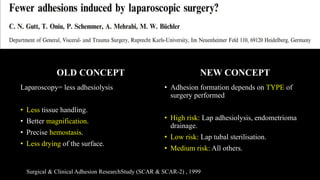
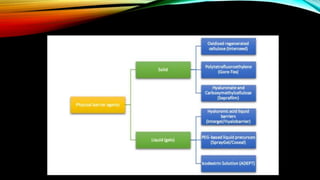
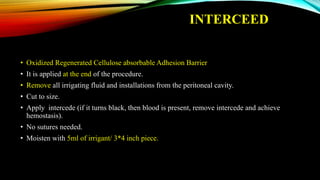
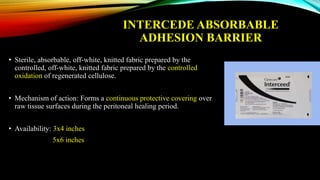
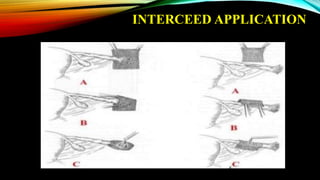
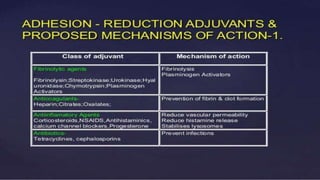
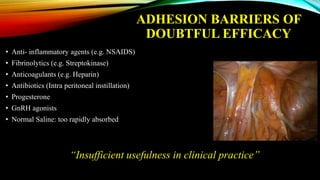
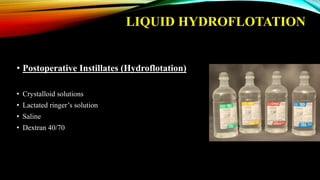
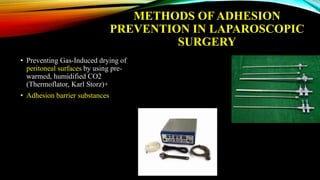
The document discusses recent advancements in preventing adhesions following laparoscopic surgery, highlighting the complications such as intestinal obstruction, infertility, and chronic pain that can arise from these adhesions. It emphasizes the importance of good surgical techniques and the efficacy of adhesion barriers, including a newly developed polymer-nanoparticle hydrogel that shows promise in significantly reducing adhesion severity. Additionally, it calls for ongoing research and awareness of the impact of postoperative adhesions on patient outcomes.