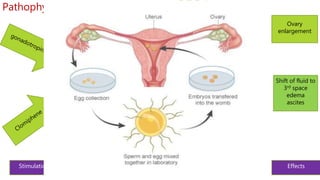
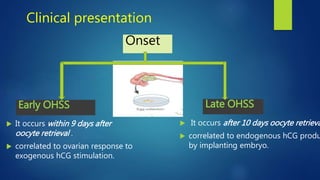
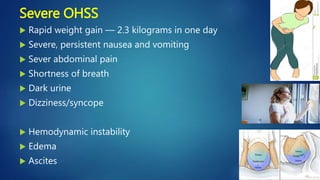
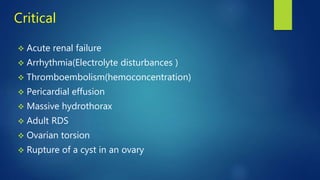
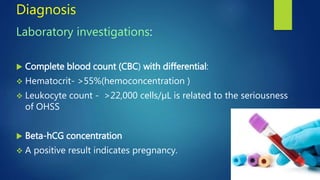
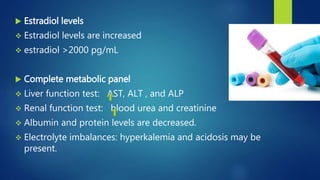
Ovarian hyperstimulation syndrome (OHSS) is an exaggerated response to ovulation induction therapy. It has multiple causes including fertility drugs like gonadotropins and hCG, as well as spontaneous cases linked to conditions like hypothyroidism. OHSS results from increased vascular permeability and third spacing of fluid due to high VEGF levels stimulated by hCG. Symptoms range from mild abdominal discomfort to life-threatening complications involving multiple organ systems. Treatment involves hospitalization, aggressive IV hydration, albumin supplementation, and sometimes paracentesis or pleural drainage for severe cases. Prevention relies on individualizing drug regimens and monitoring ovarian response closely.