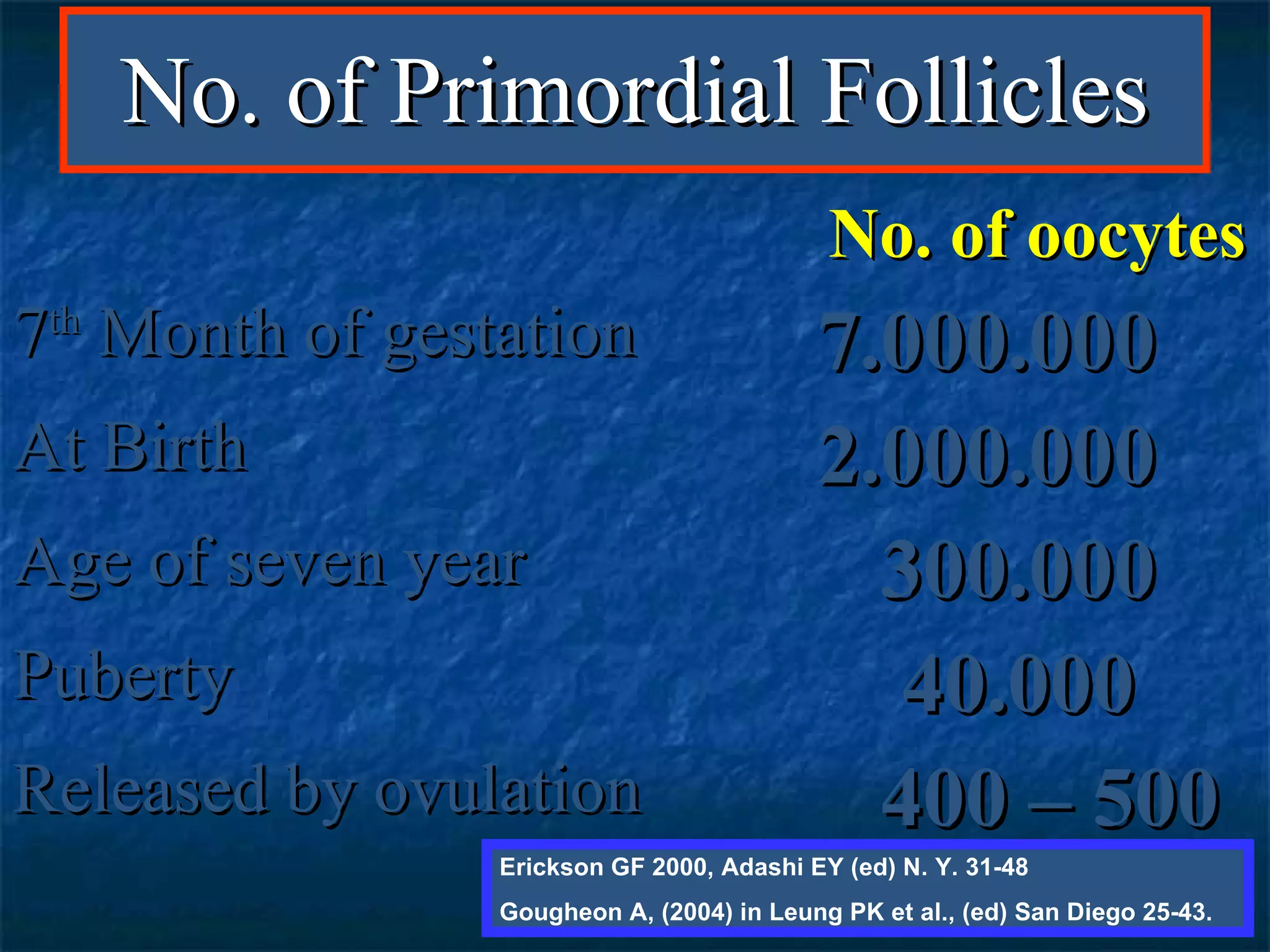
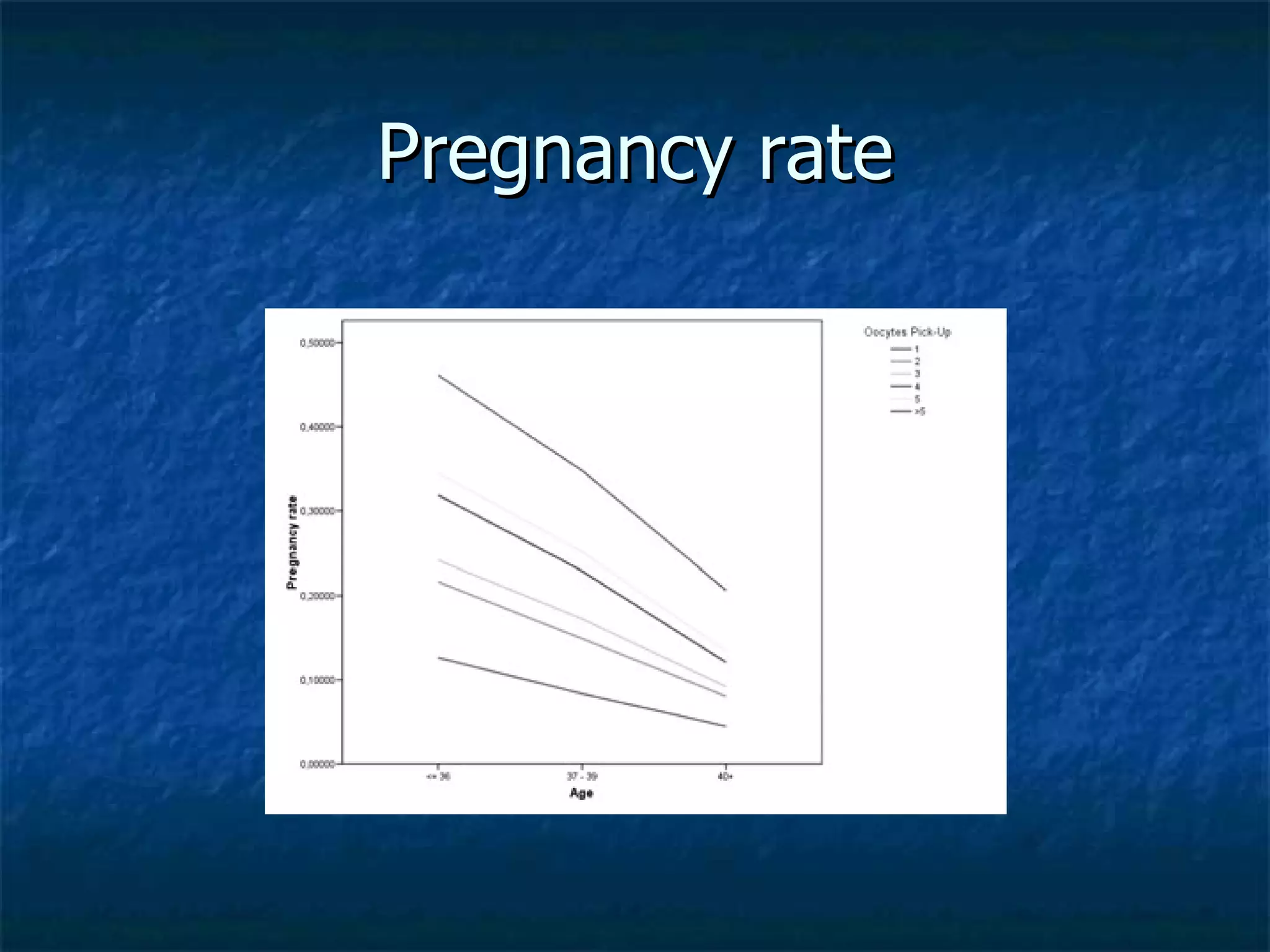
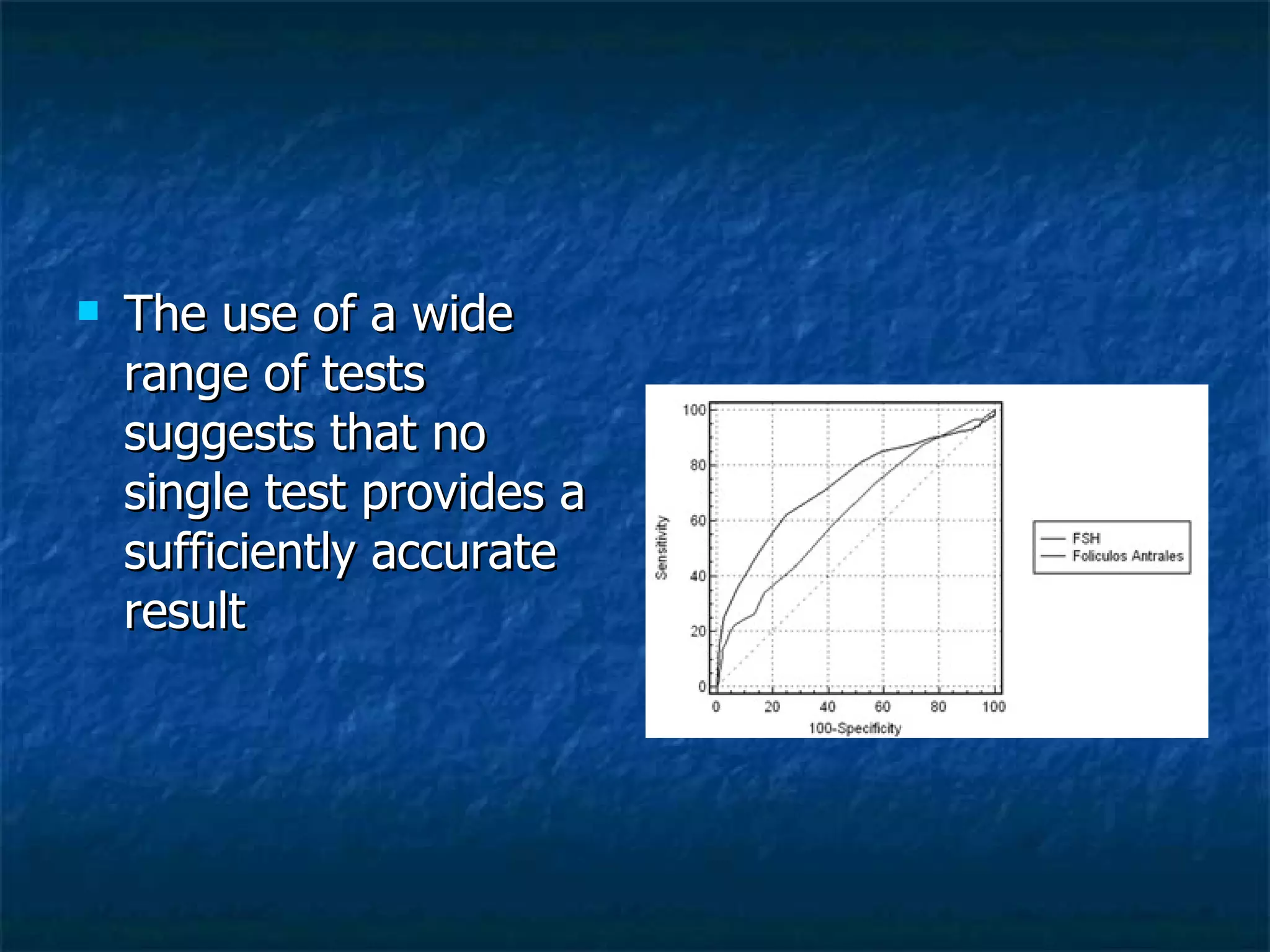
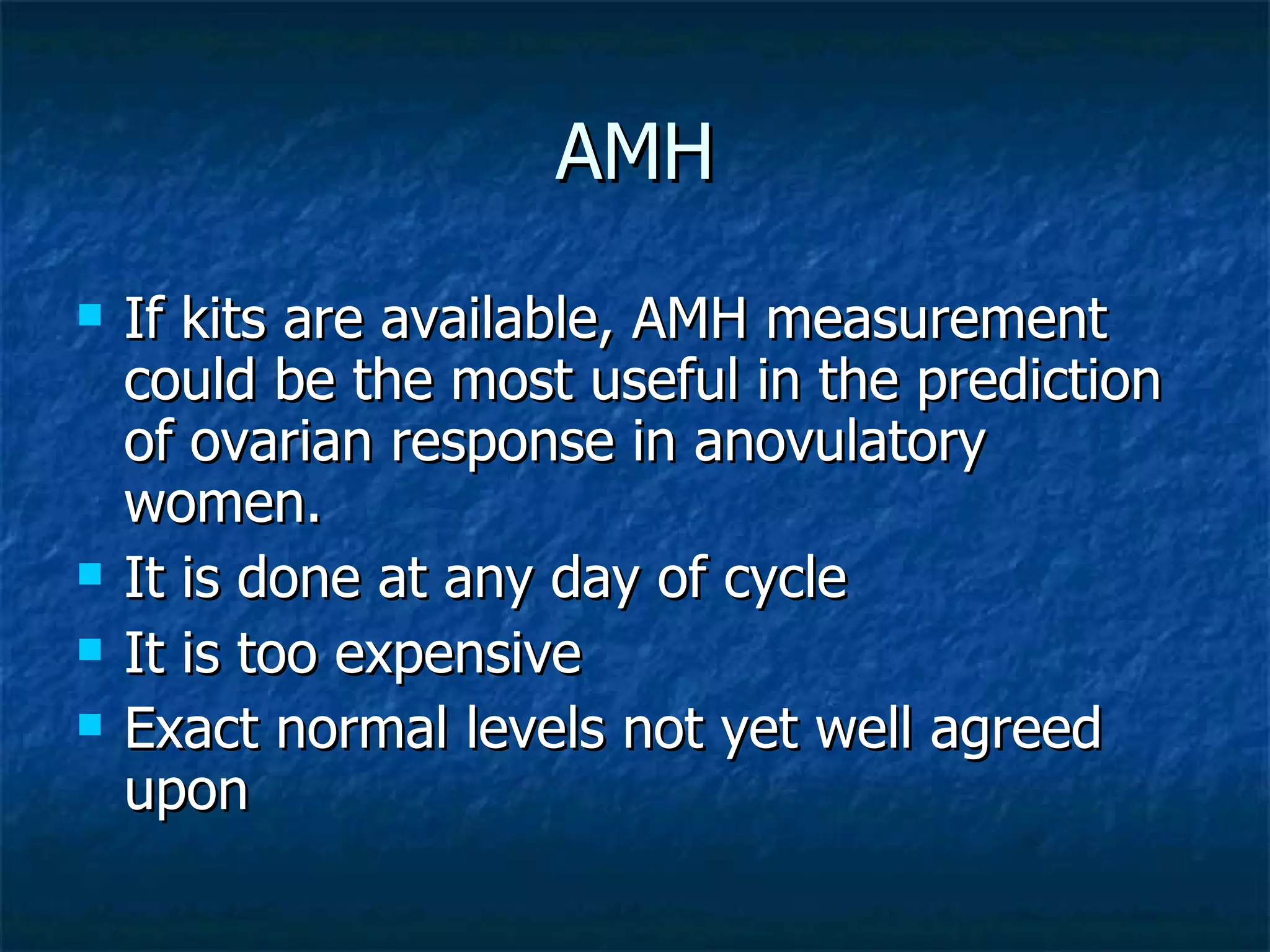
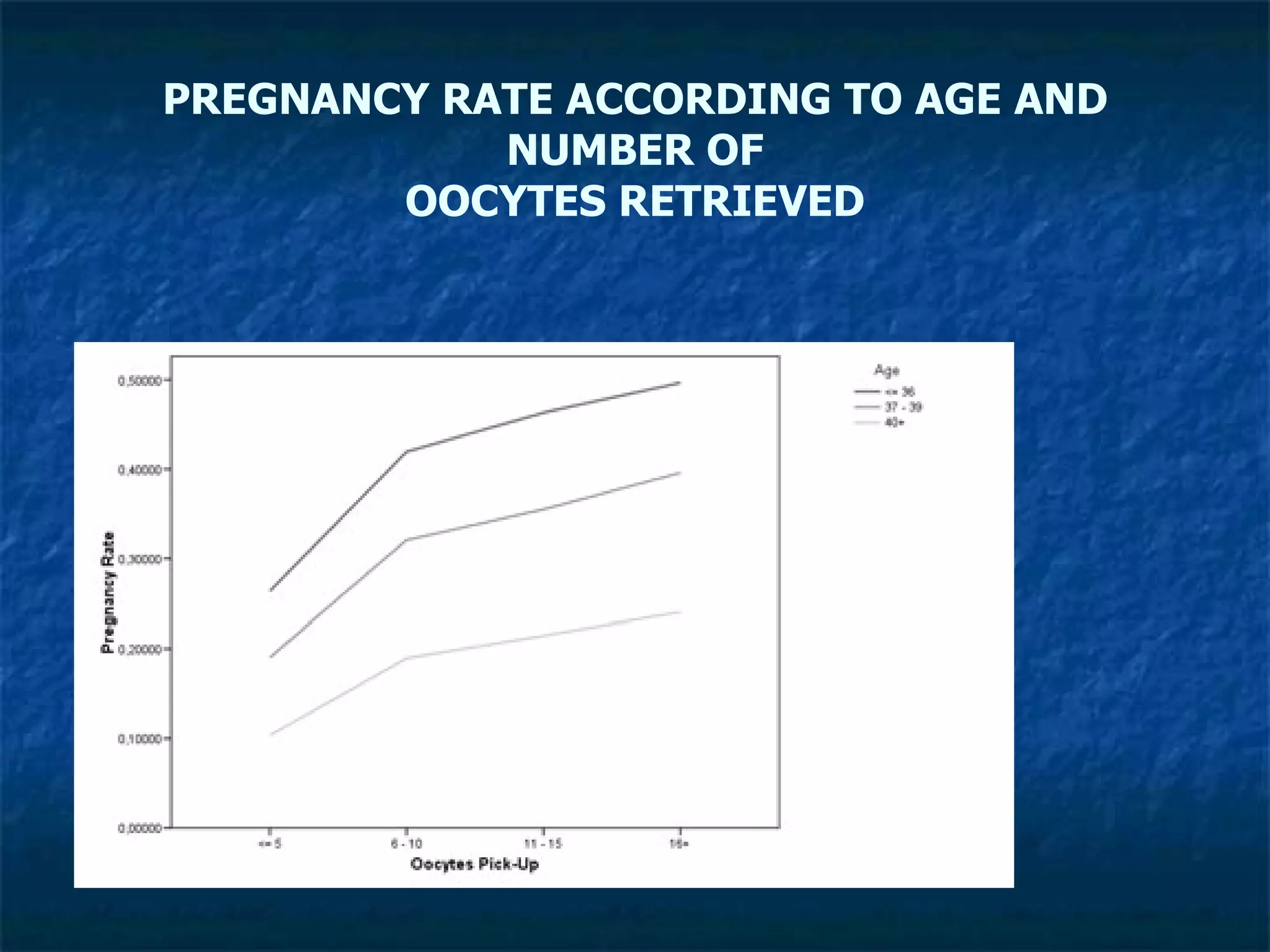
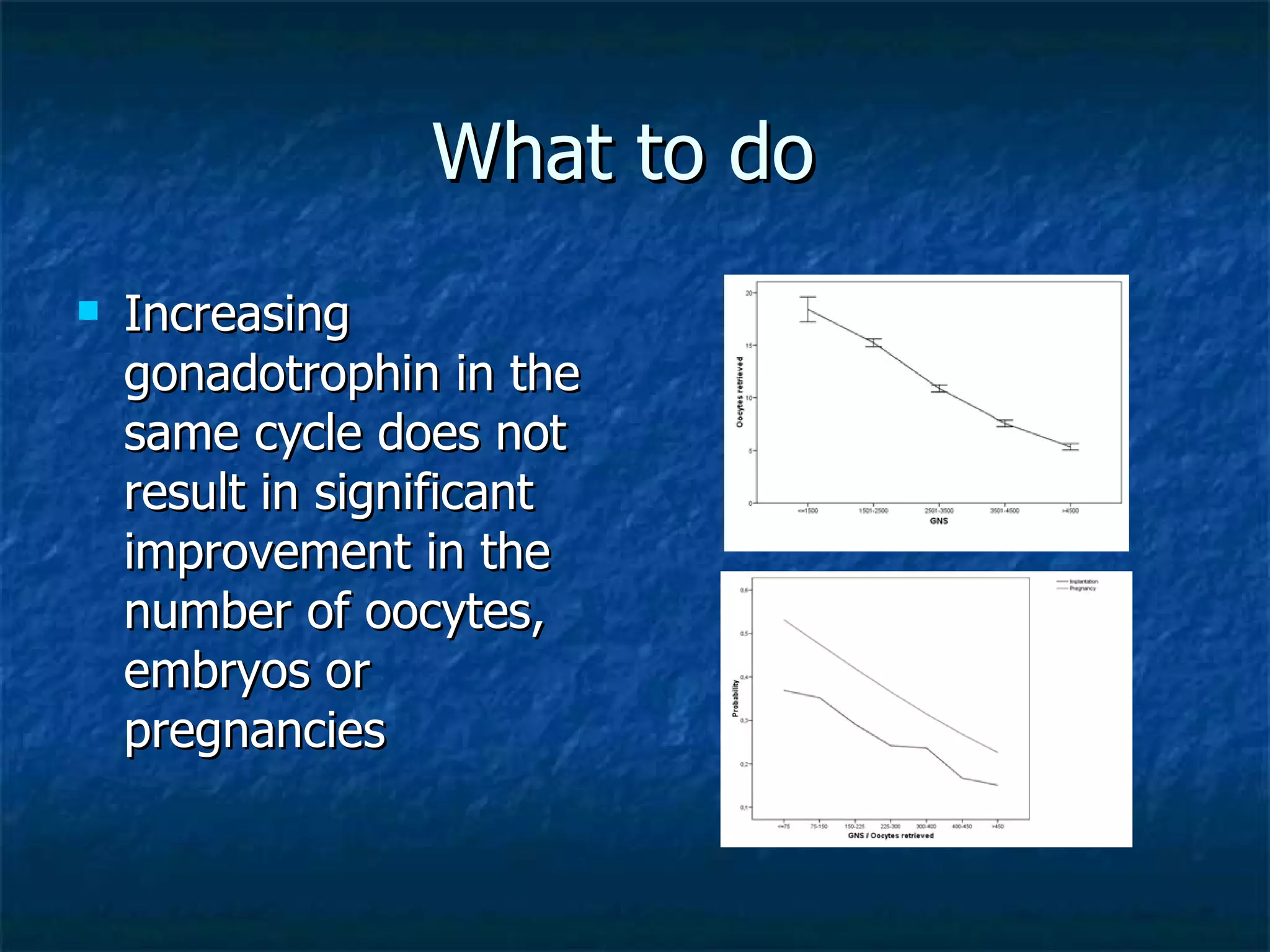
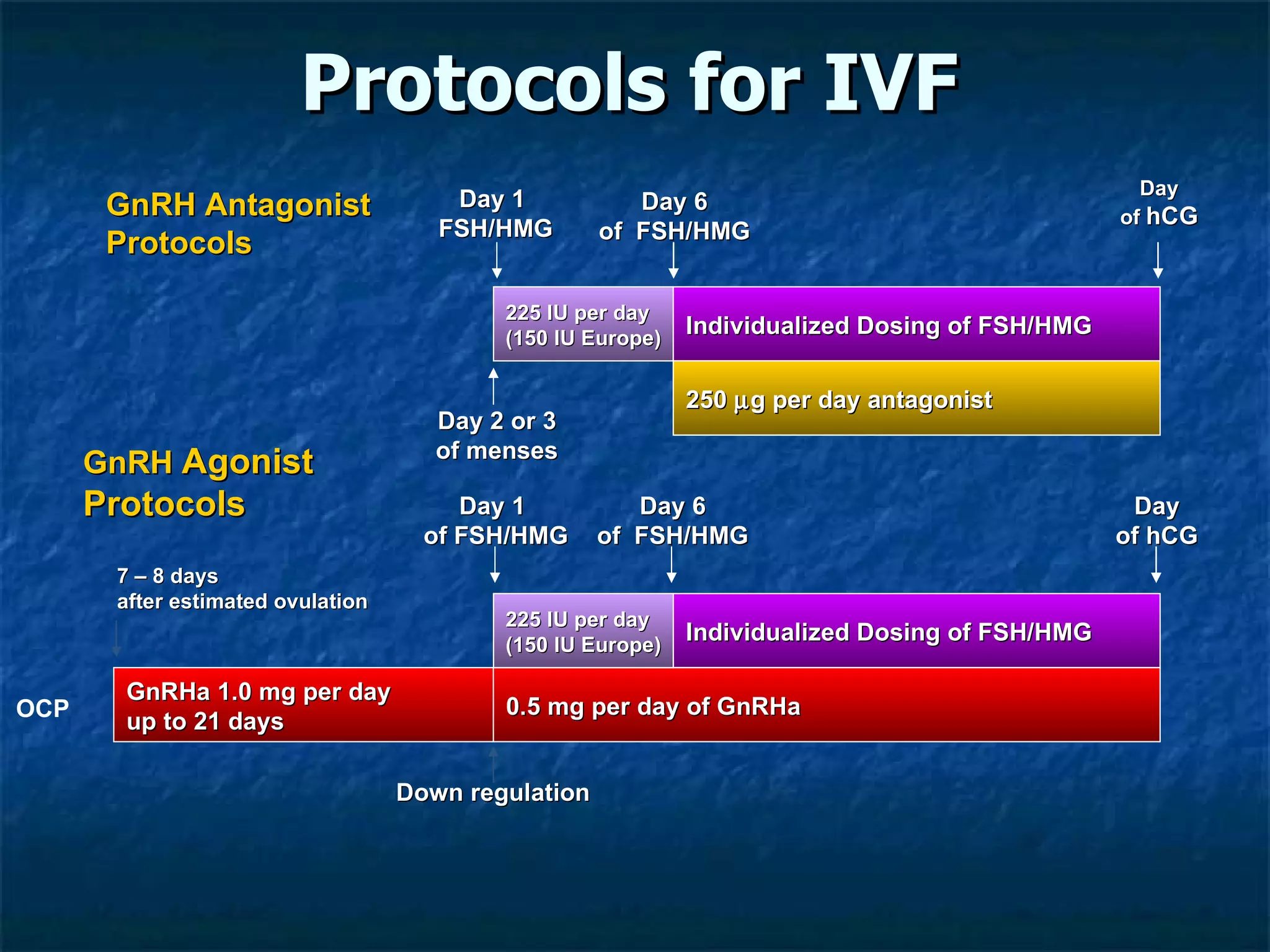
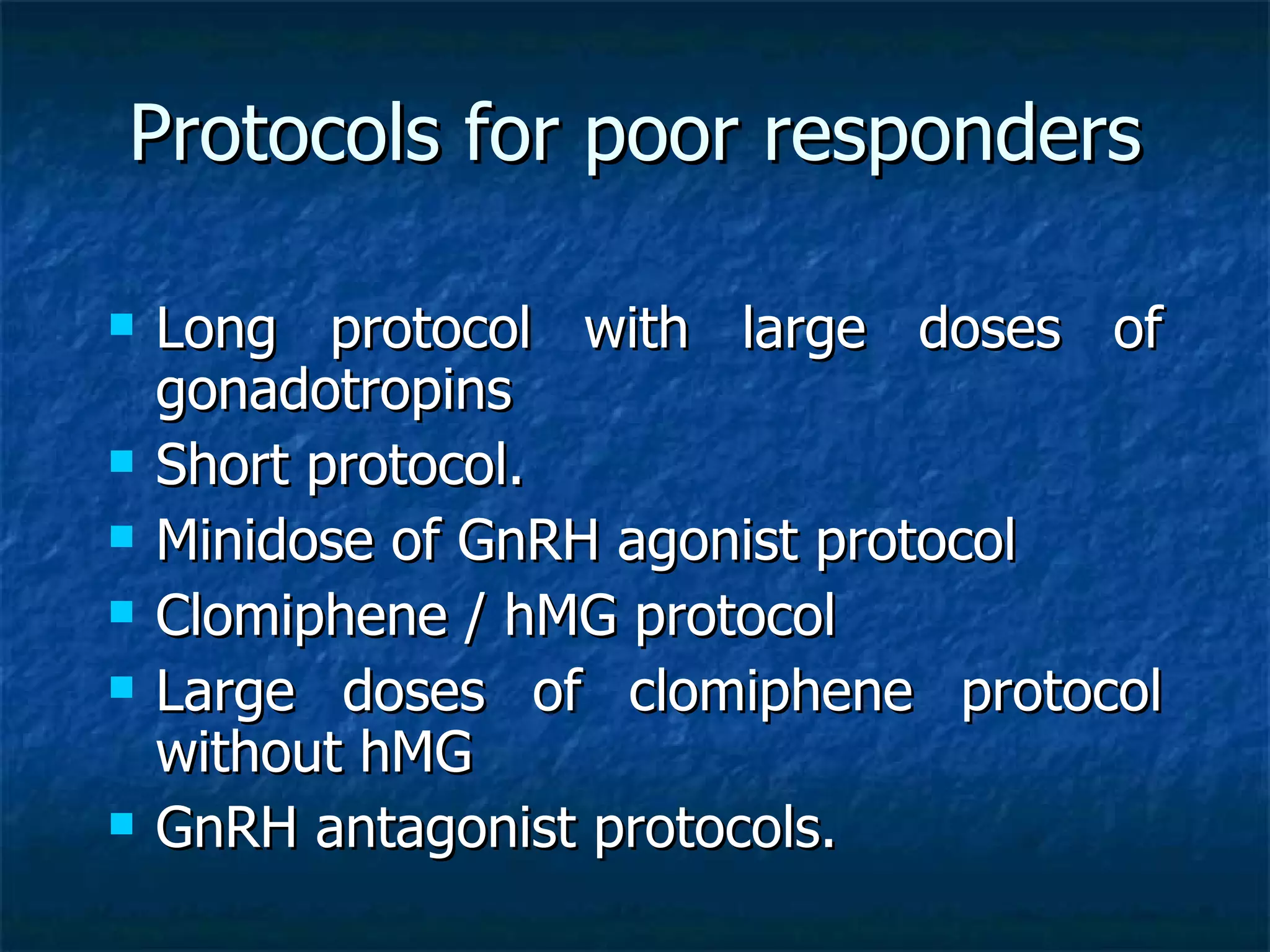
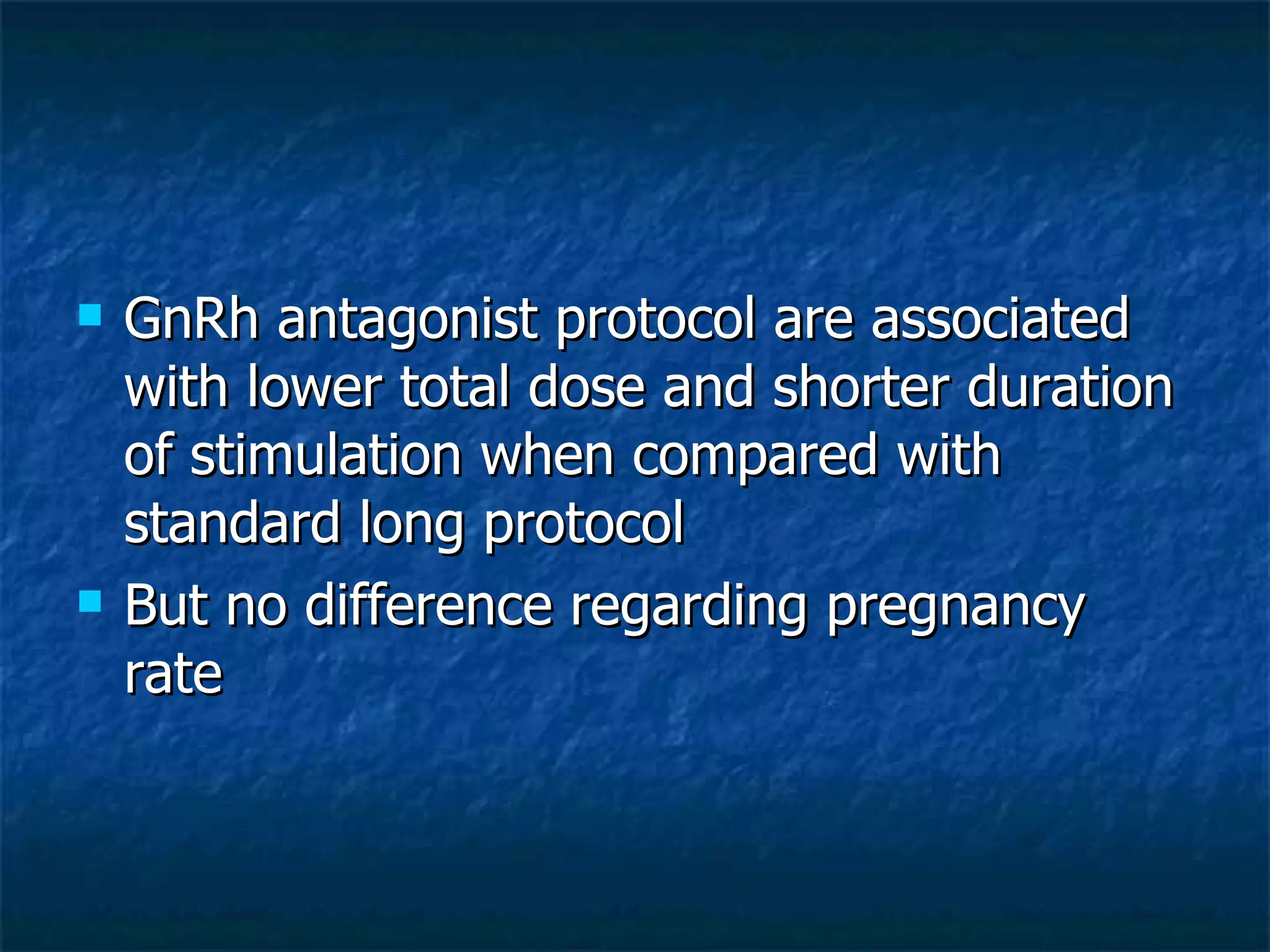
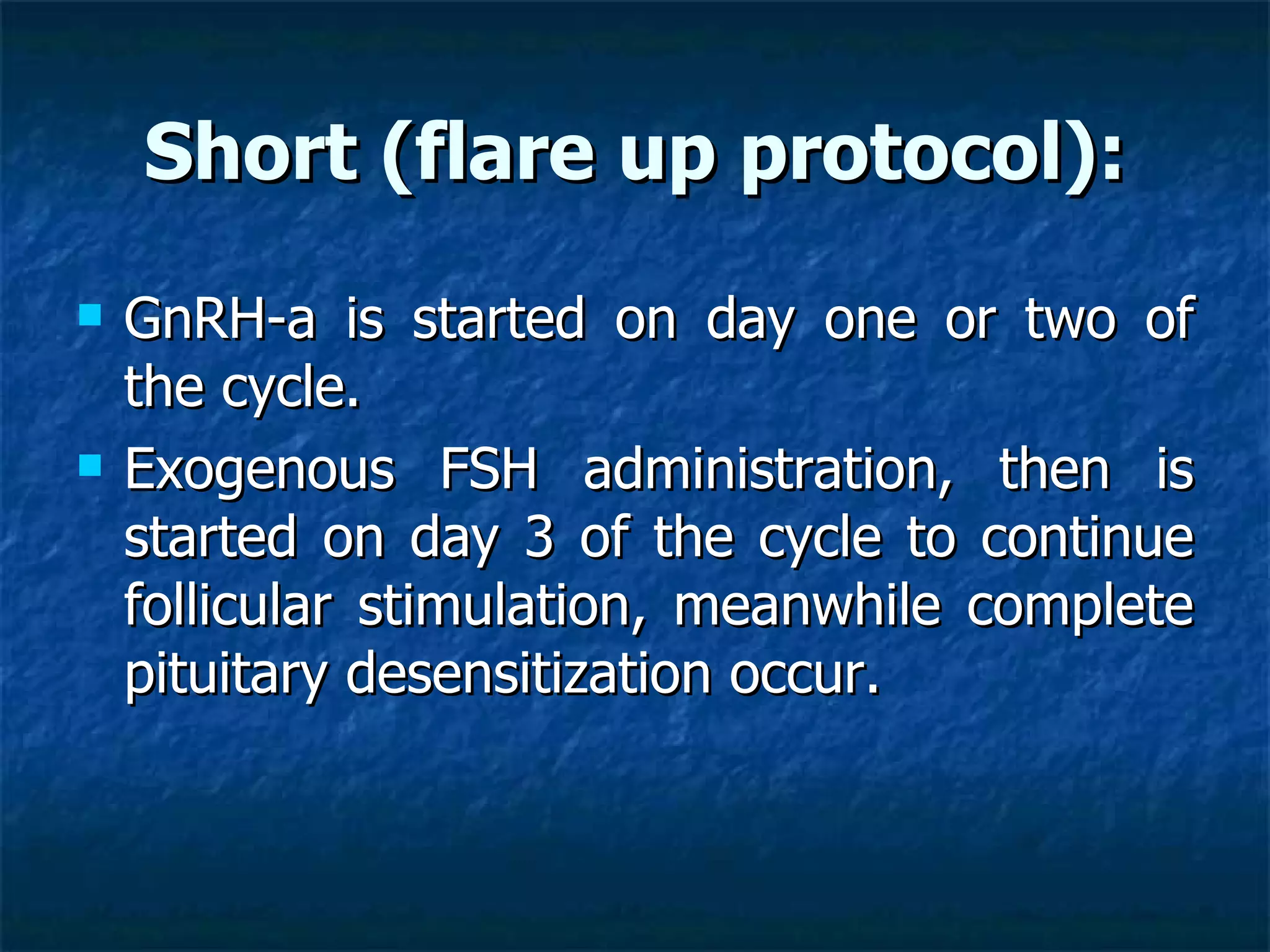
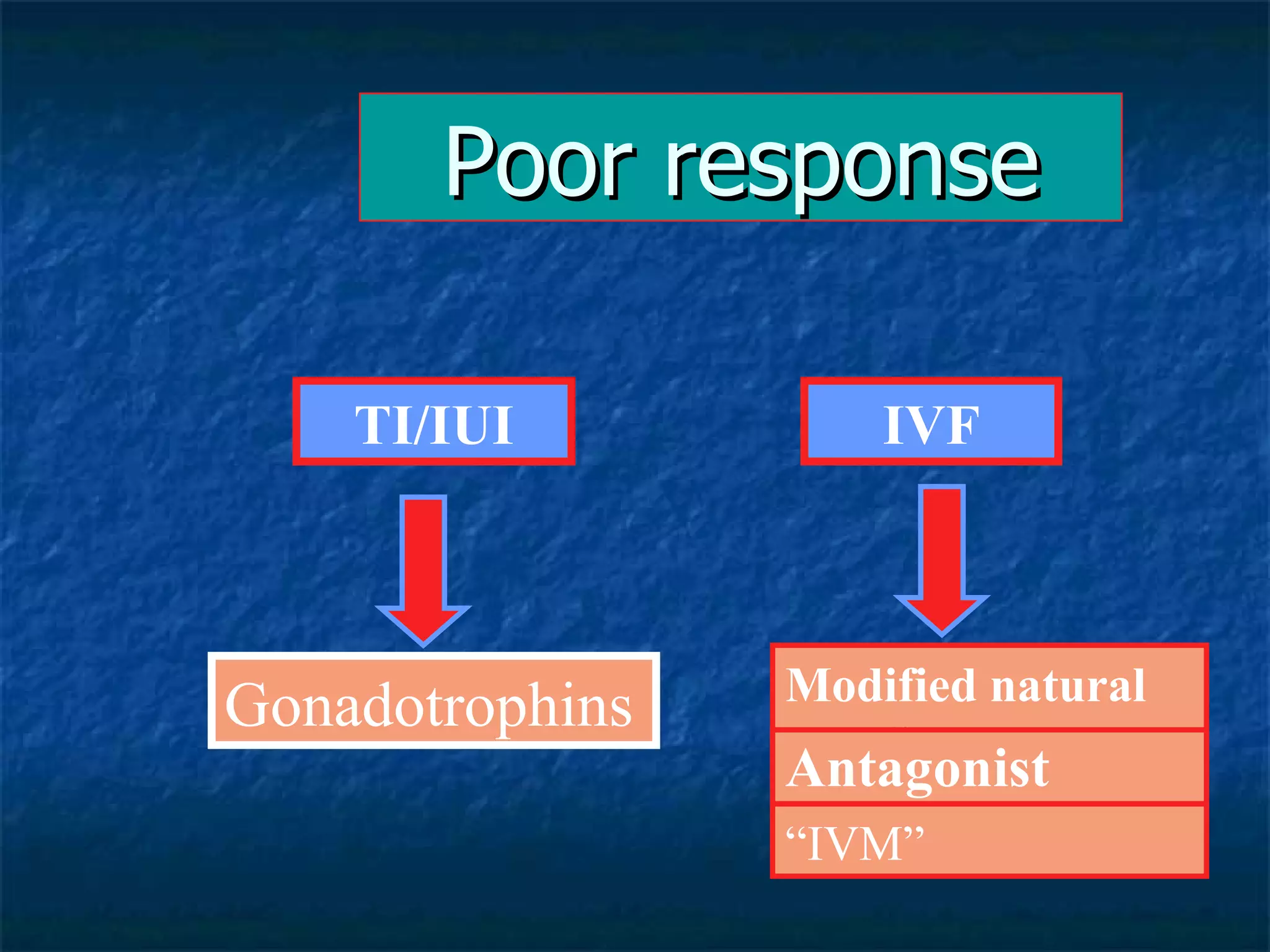
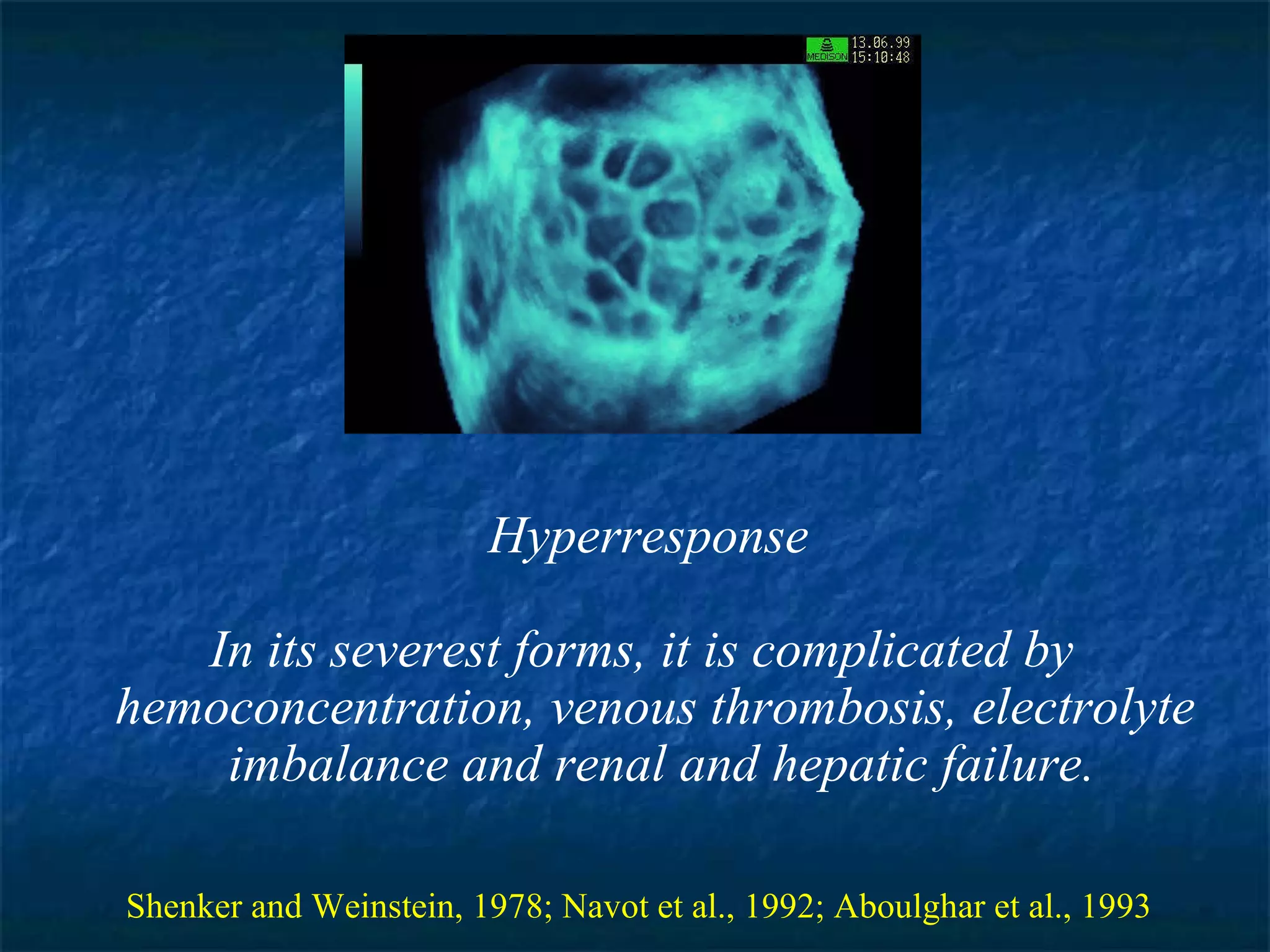
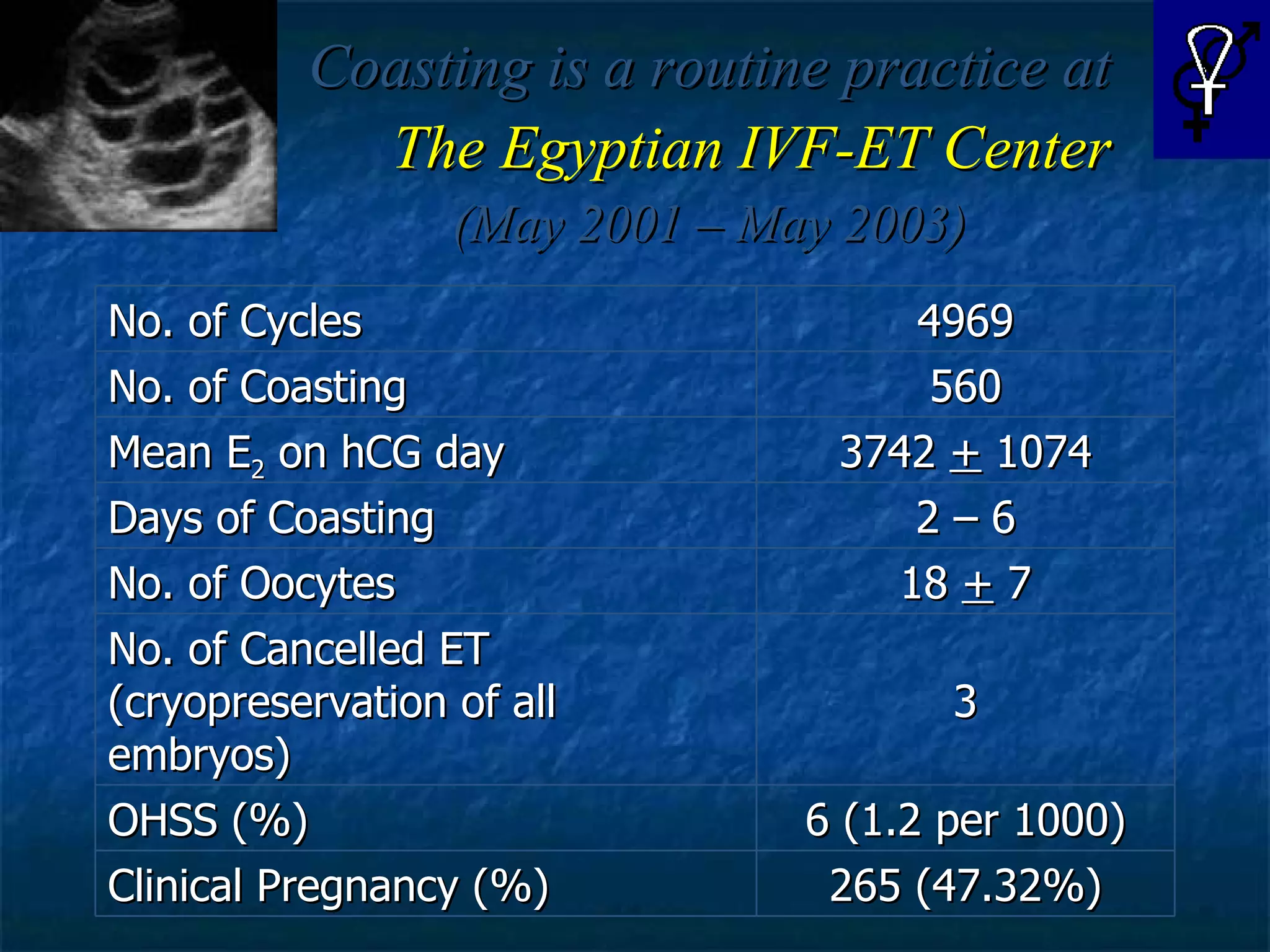
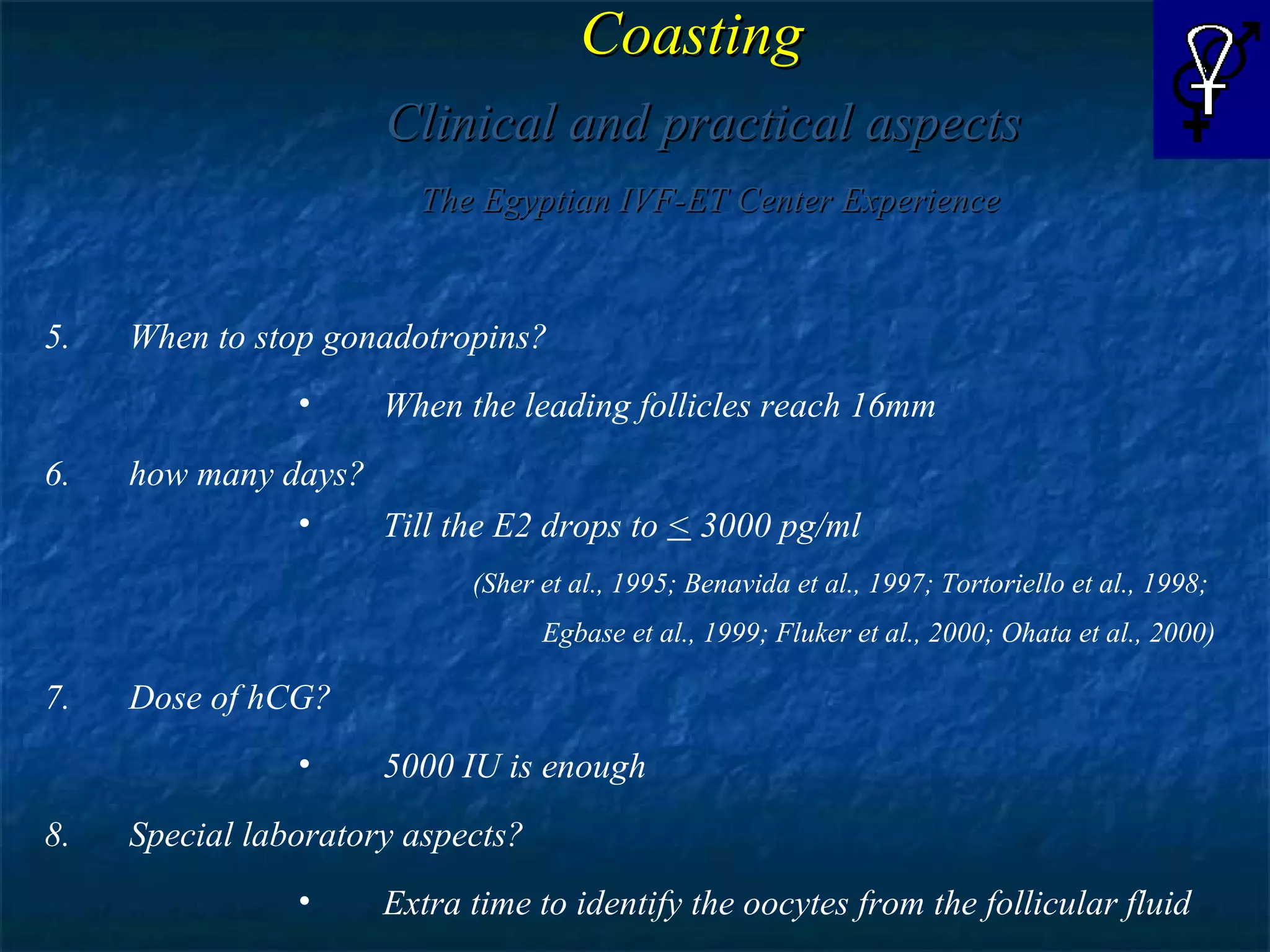
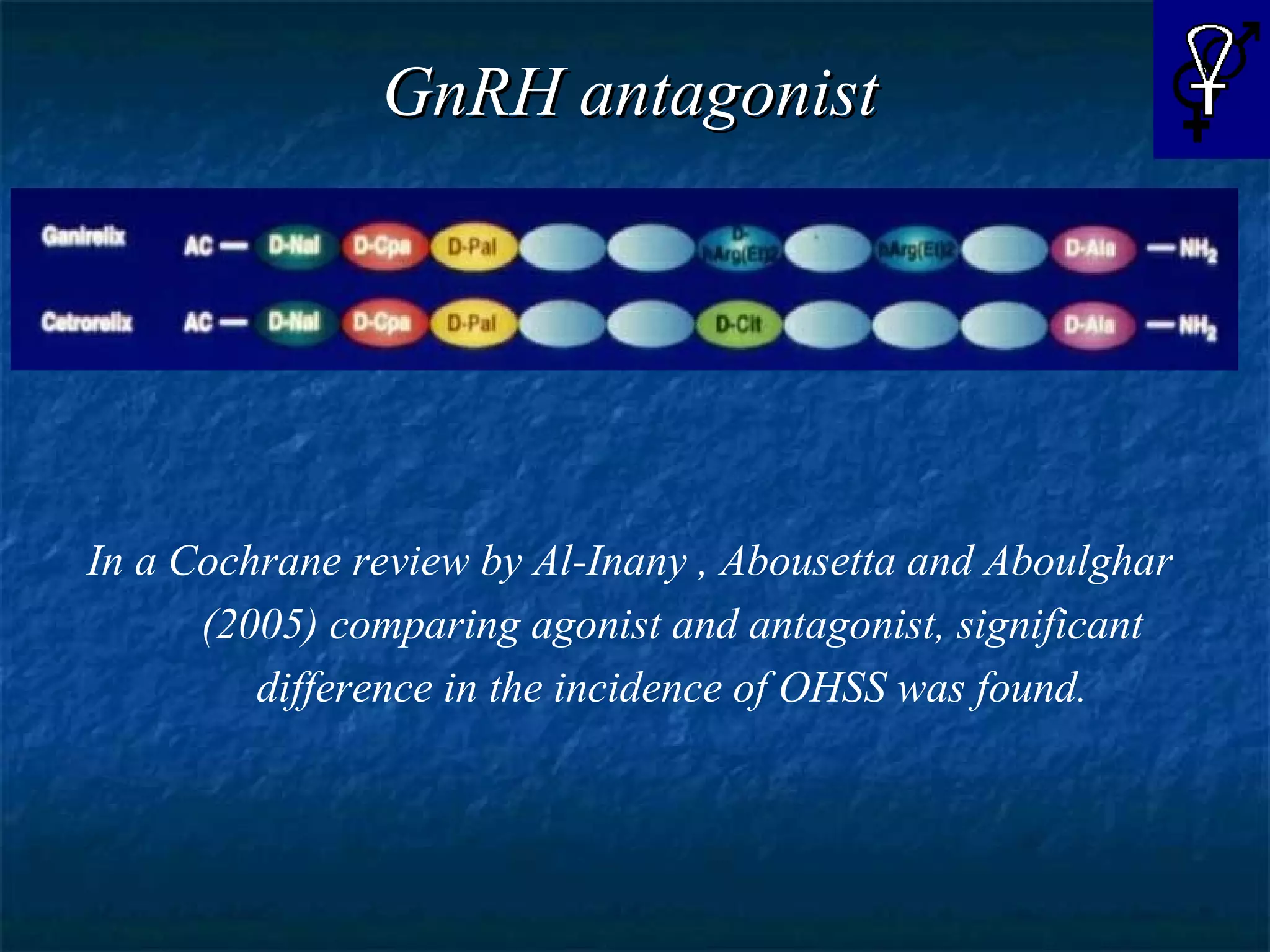
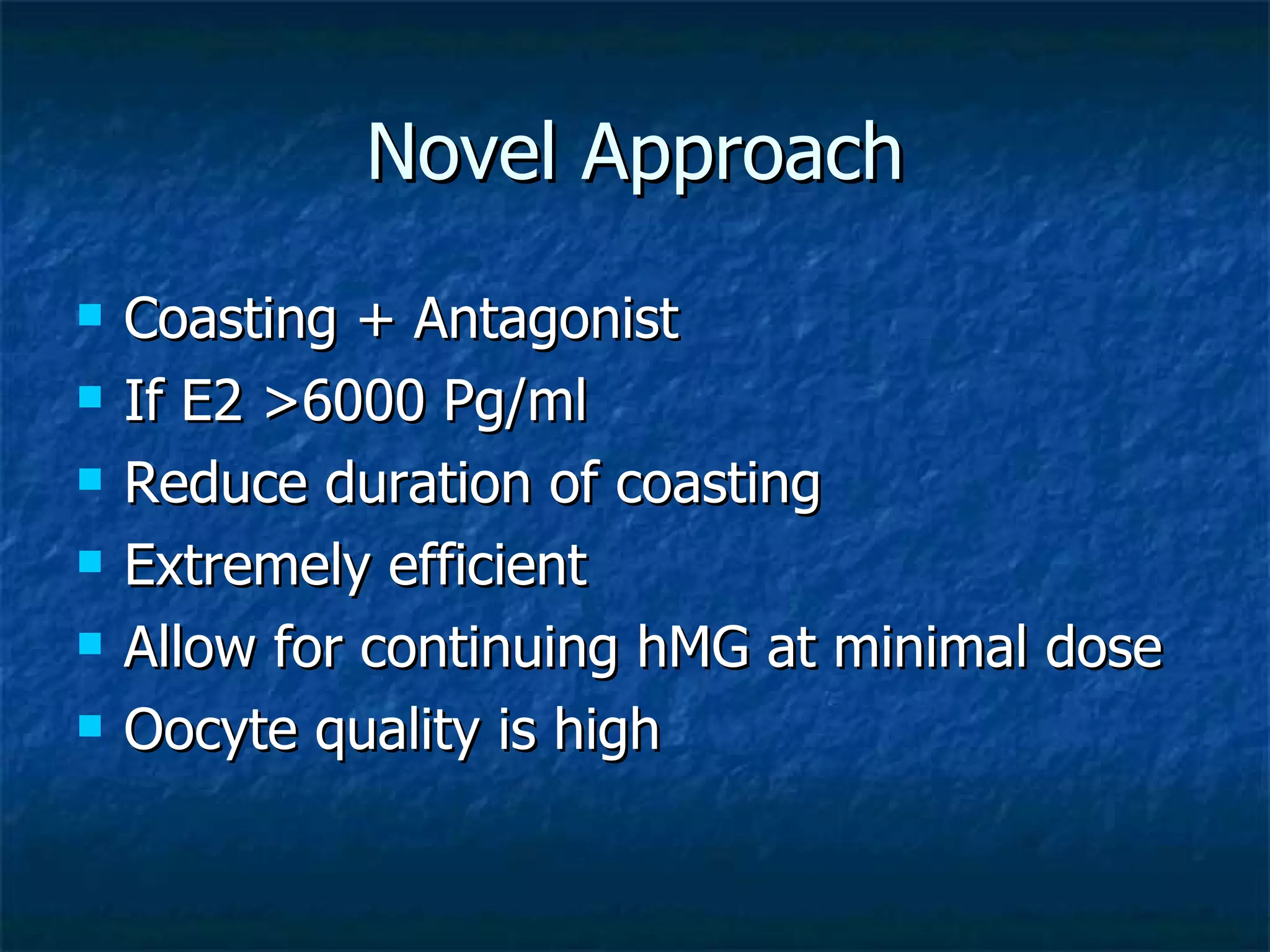
This document discusses the management of poor or hyper ovarian response in IVF treatment. It covers topics such as predicting ovarian reserve, definitions of poor response, protocols for poor and hyper responders, and techniques like coasting to help prevent ovarian hyperstimulation syndrome. Coasting, where gonadotropin administration is stopped but down regulation continued, is an effective way to prevent OHSS while still allowing for embryo retrieval and transfer. GnRH antagonist protocols may also help lower the risk of OHSS compared to long agonist protocols. There is no single best protocol, and treatments should be individualized based on patient factors and expectations.