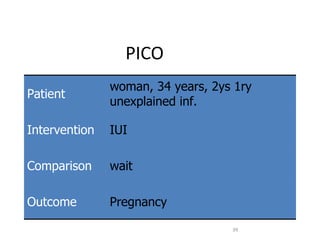
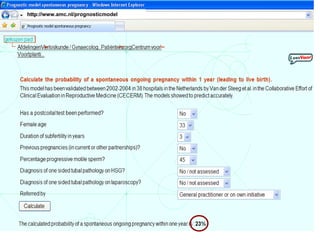
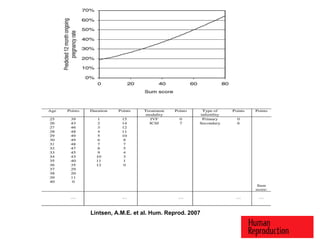
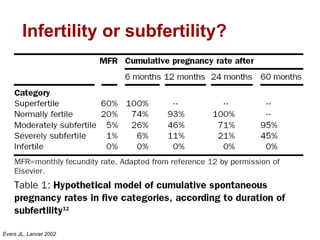
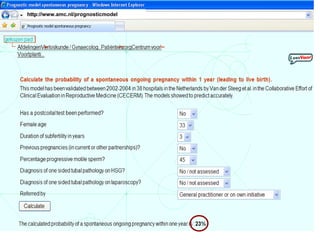
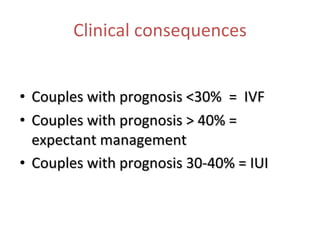
1. Prognostic models can help predict the chances of conceiving naturally, conceiving with interventions like IUI or IVF, and the chances of live birth from IVF.
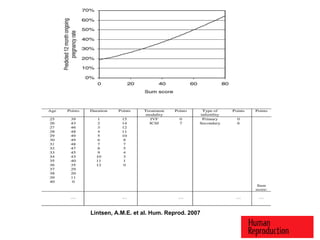
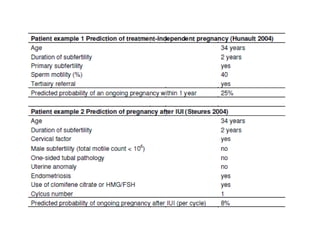
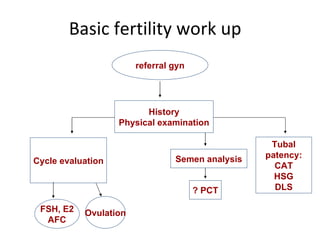
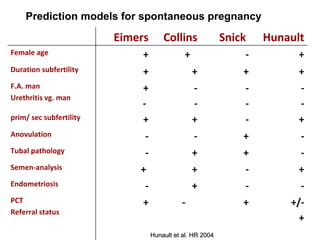
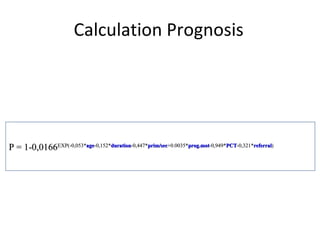
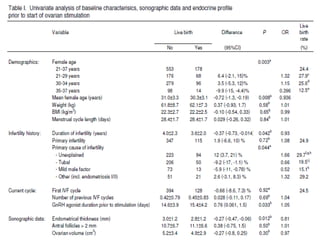
2. Key factors in these models include female age, duration of infertility, cause of infertility, ovarian reserve tests, and data from previous treatment cycles.
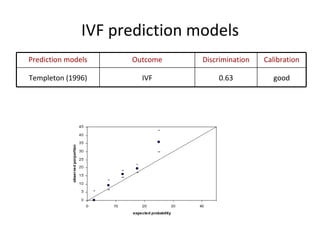
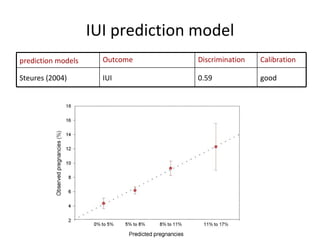
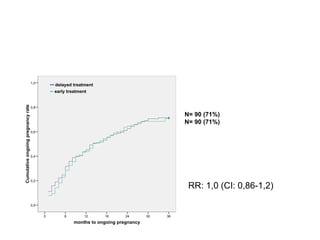
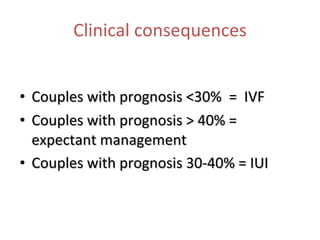
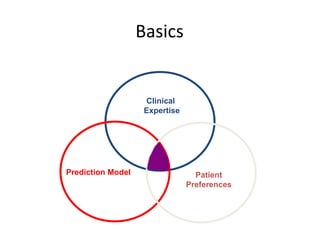
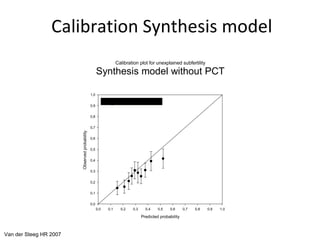
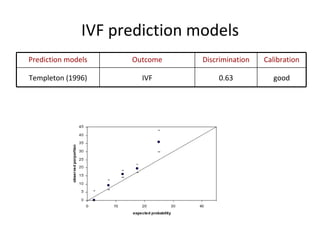
3. Existing prediction models have been shown to have good discrimination and calibration for outcomes like IUI or IVF success, though individual patient preferences must also be considered in treatment decisions.
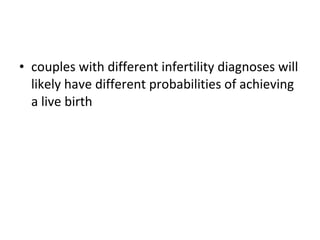
![Calculation The predicted probability ( P ) of achieving a live birth after IVF was calculated using the Templeton the model: Where y was defined as y = –2.028 + [0.00551x( age – 16)2] – [0.00028x(age – 16)3] + [i – (0.0690x no. of unsuccessful IVF attempts )] – (0.0711xtubal subfertility) + (0.7587xlive birth after IVF) + (0.2986 x previous pregnancy after IVF which did not result in a live birth) + (0.2277x live birth which was not a result of IVF) + (0.1117x previous pregnancy , not after IVF and which did not result in a live birth).](https://image.slidesharecdn.com/prognostic-110629014129-phpapp02/85/Prognostic-models-32-320.jpg)