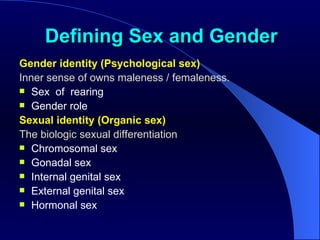
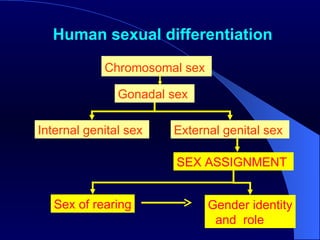
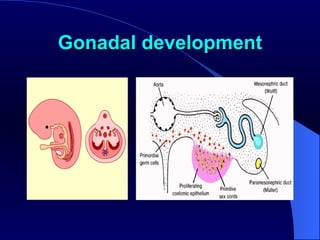
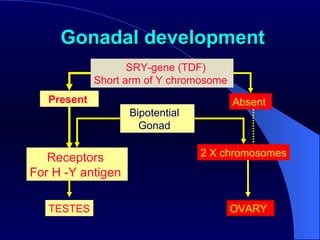
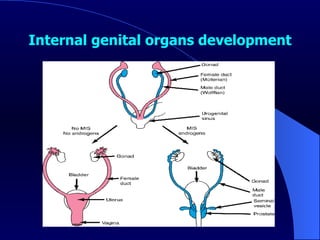
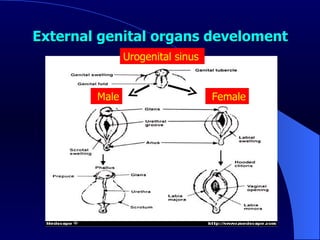
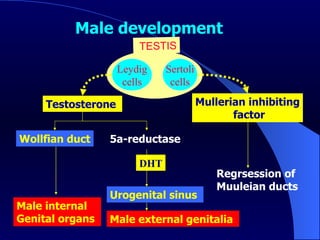
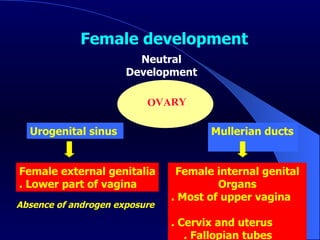
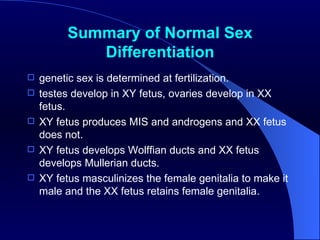
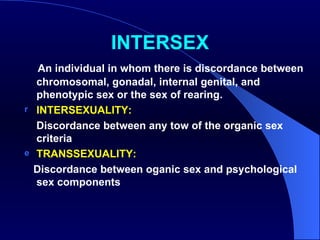
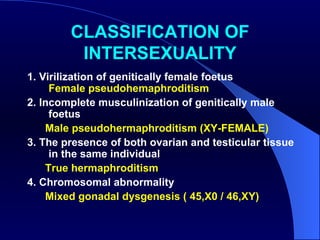
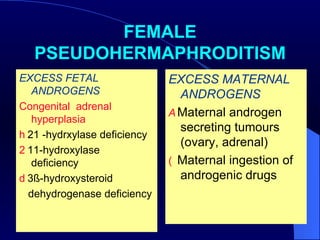
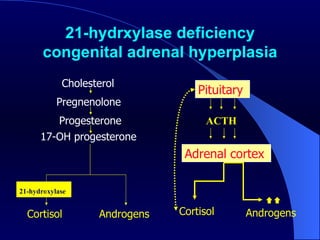
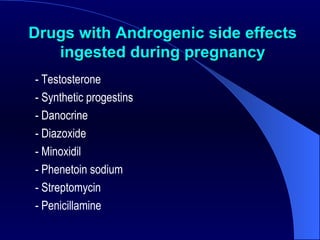
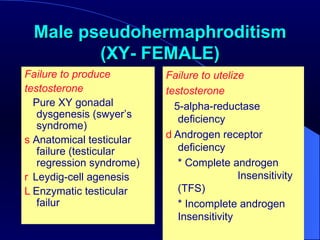
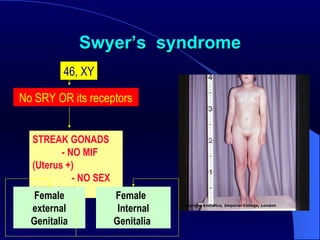
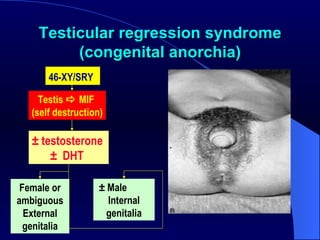
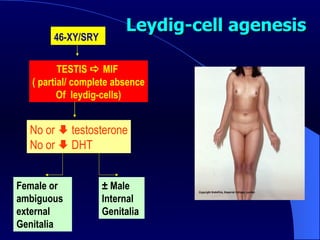
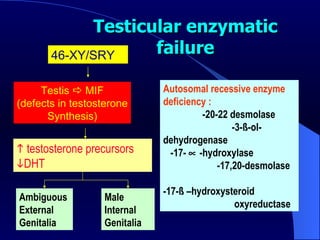
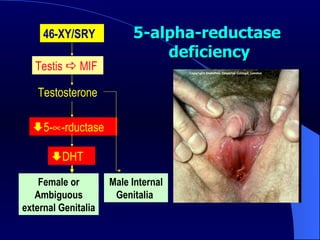
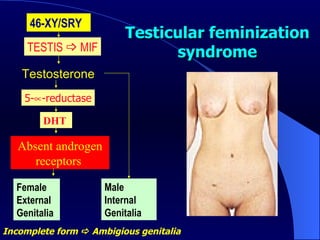
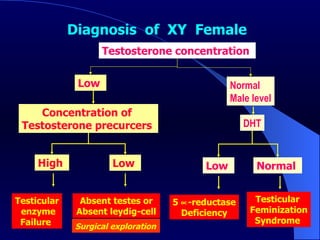
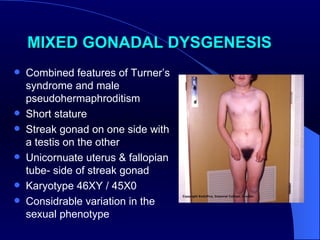
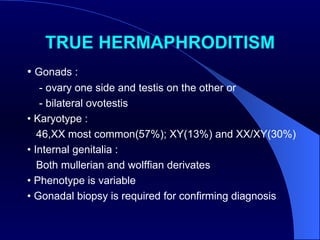
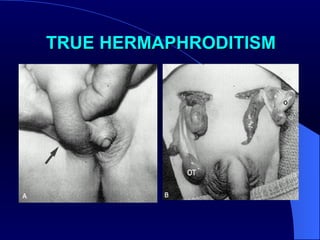
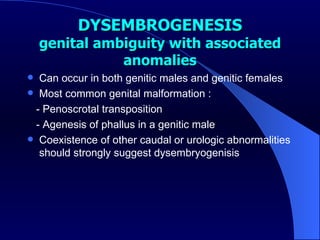
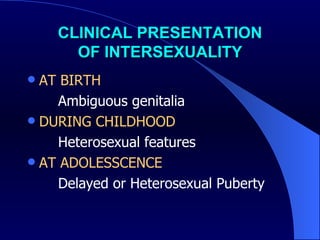
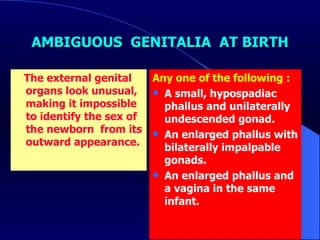
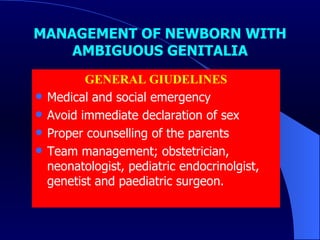
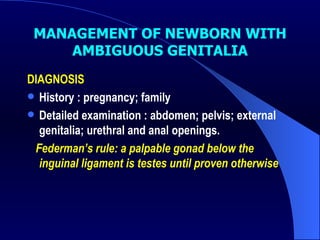
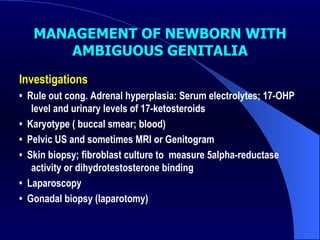
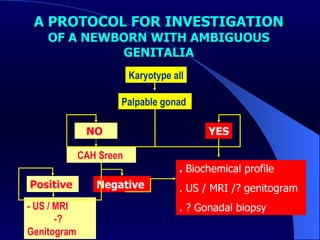
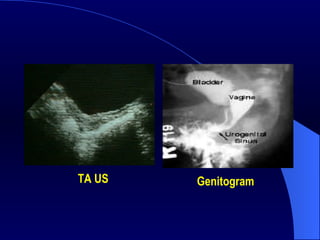
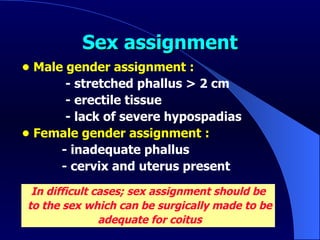
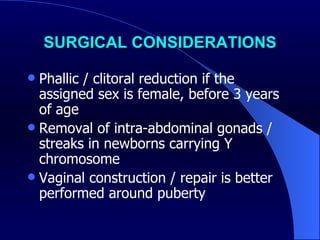
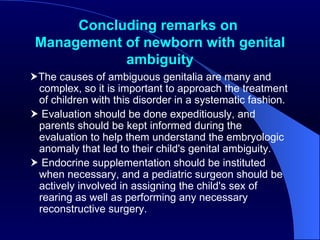
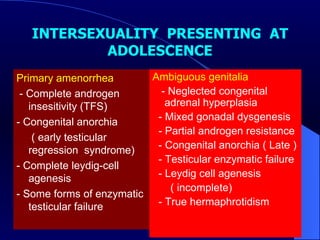
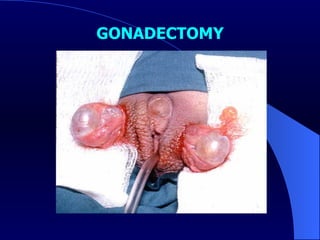
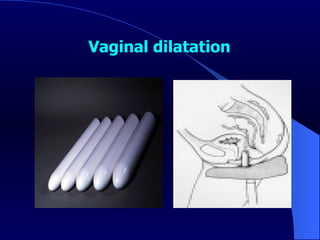
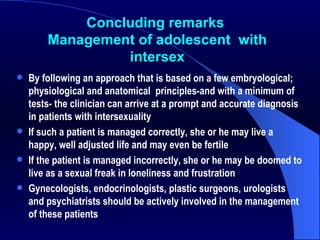
The document discusses intersexuality and sexual differentiation. It defines the different levels of sex including chromosomal, gonadal, genital and hormonal sex. Normal sexual differentiation is described where XY fetuses develop testes and masculinize, while XX fetuses develop ovaries. Intersex conditions occur when there is discordance between levels of sex. They include virilization of genetic females, incomplete masculinization of genetic males, and true hermaphroditism. The most common cause of intersex is congenital adrenal hyperplasia. Management of intersex newborns involves medical evaluation and counseling, with the goal of assigning sex by 18 months of age based on surgical and medical potential.