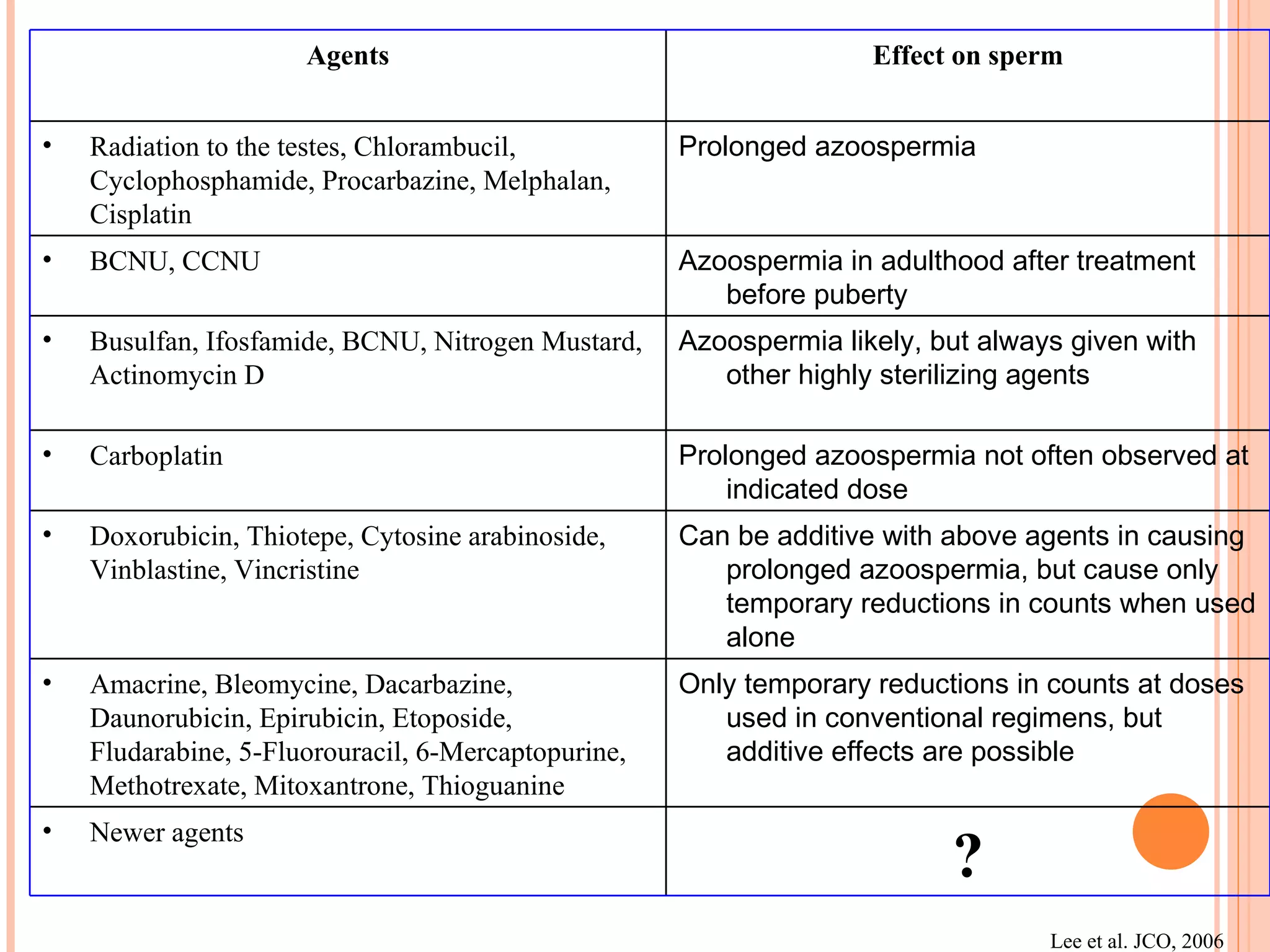
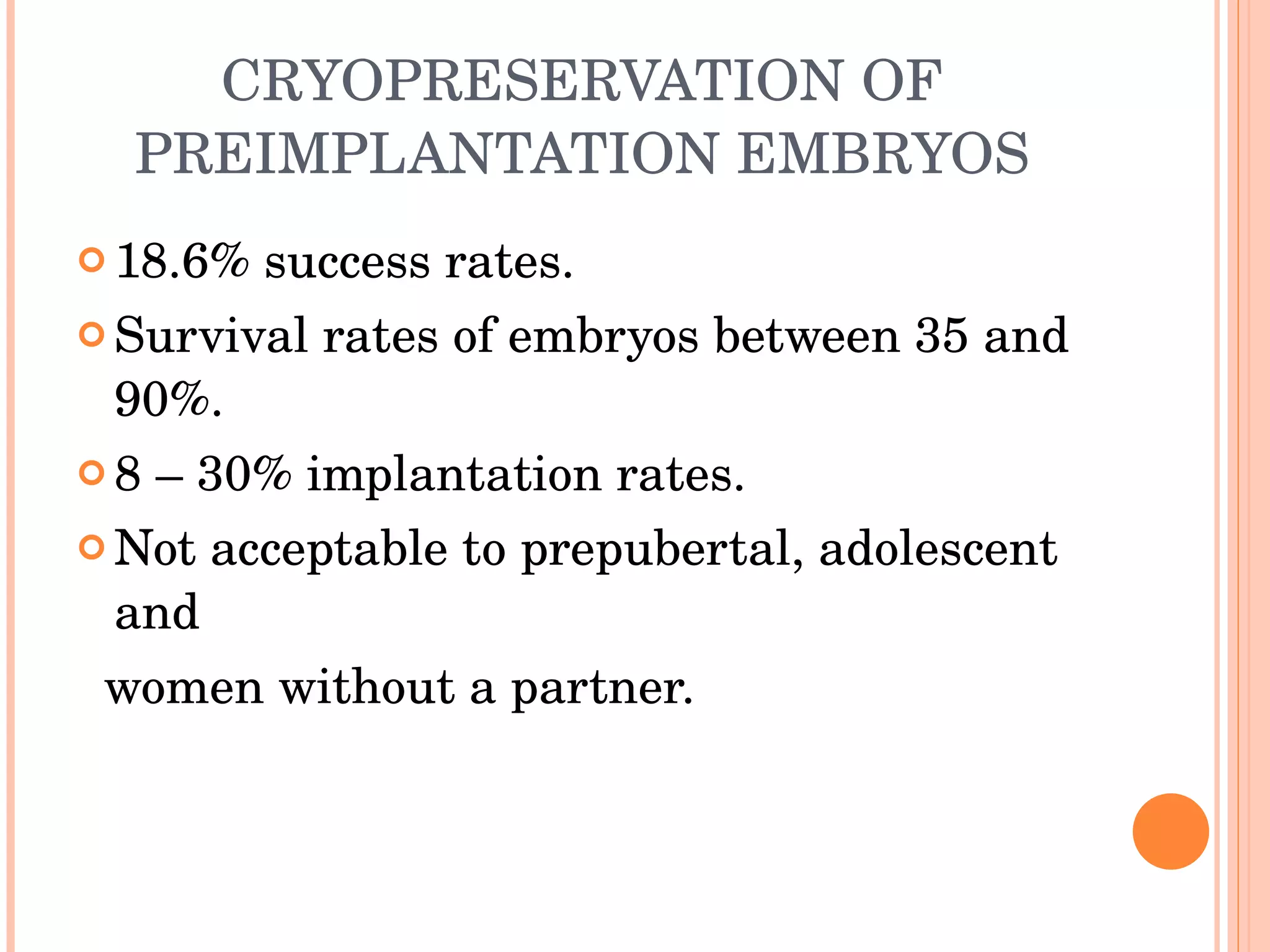
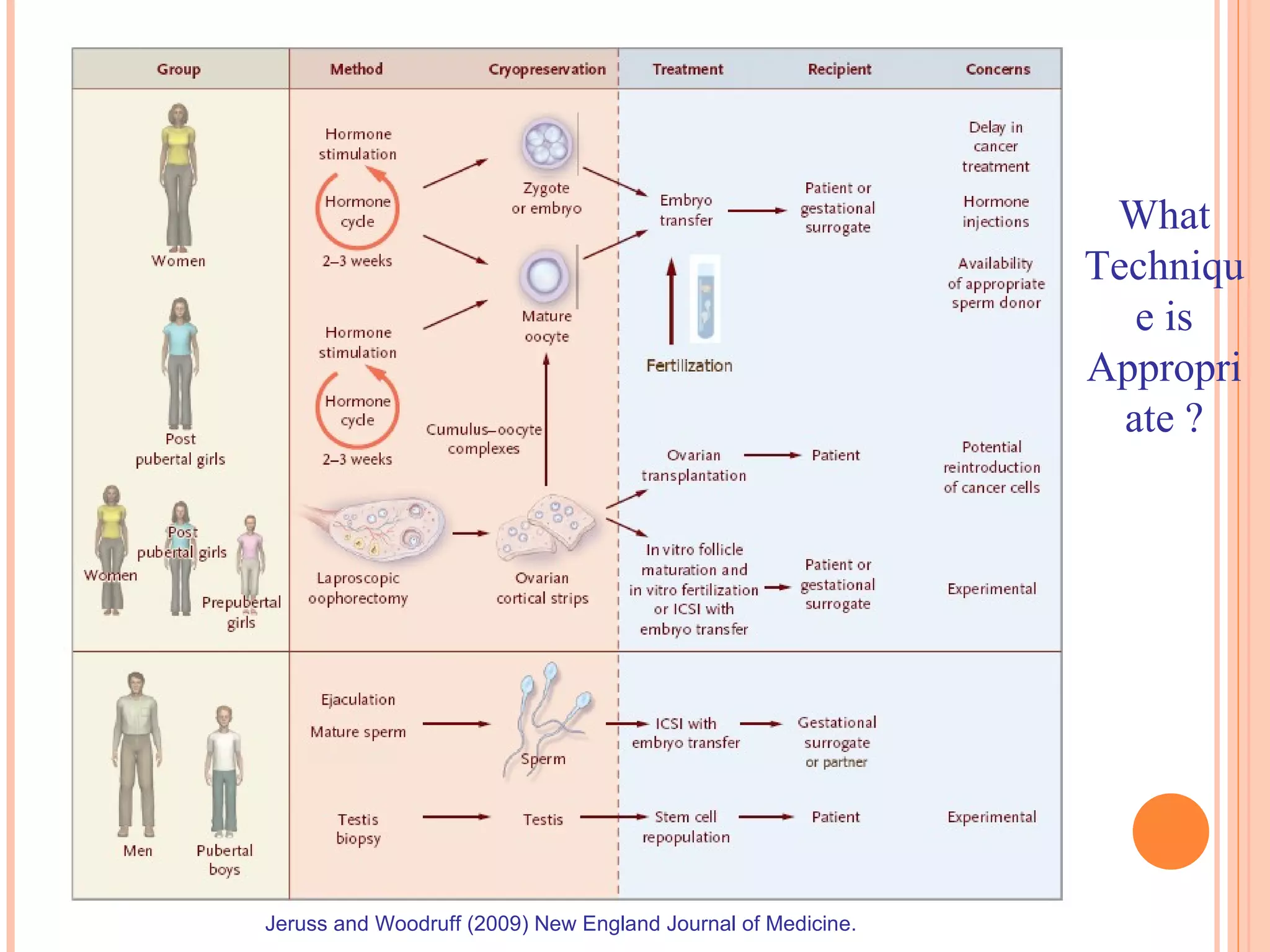
The document discusses various fertility preservation strategies for cancer patients undergoing chemotherapy or radiation therapy. It describes how certain cancers are more common in reproductive aged women and men. It then outlines different options for preserving fertility including pharmacological protection with GnRH analogues, IVF with embryo cryopreservation, oocyte cryopreservation, ovarian transposition, and ovarian tissue cryopreservation and transplantation. It notes the limitations, success rates, and complications of each method.